Indexed In
- JournalTOCs
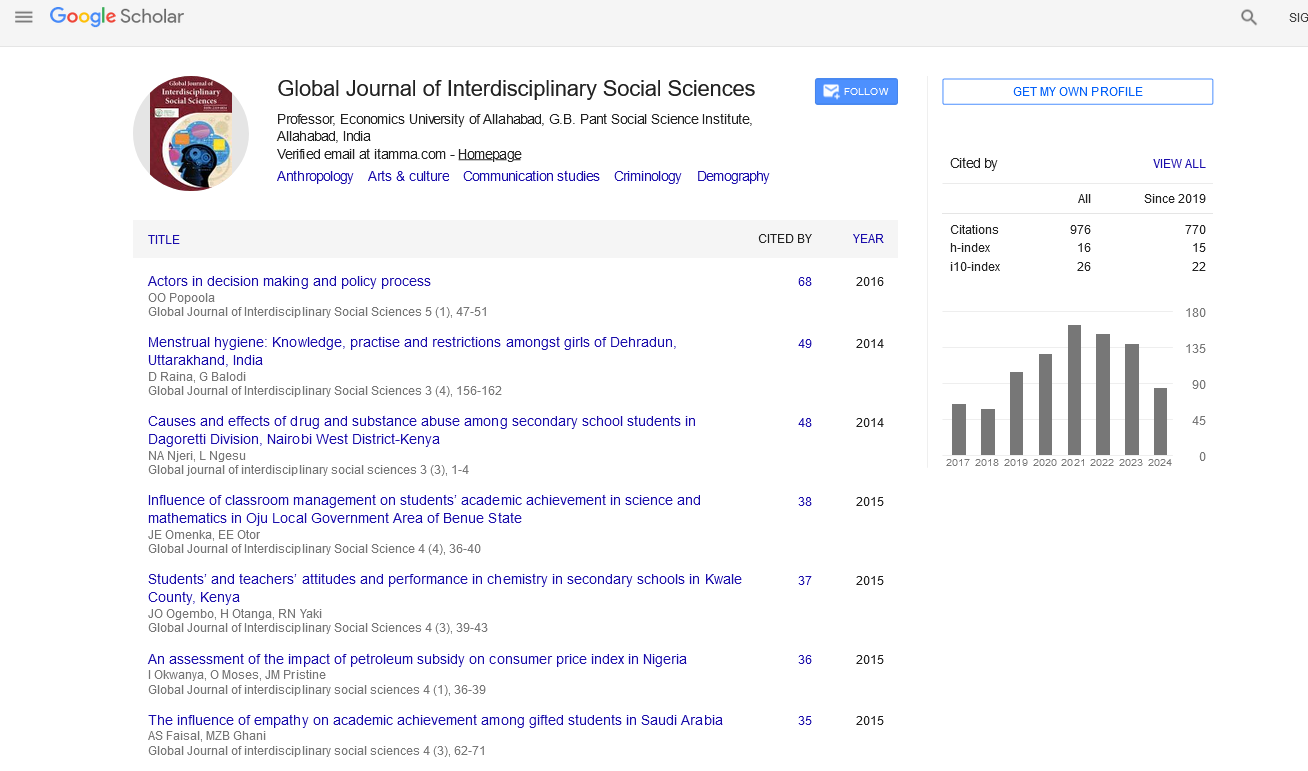
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Womens Health Promotion Through Empowerment in Community Activities: The Case of an Elderly Ultraorthodox Jewish Population
Meni Koslowsky
A popular area of research for understanding the relationship between mind and body is empowerment. Empowerment refers to individuals’ feelings that they will be able to manage the challenges in one’s personal and public life by gaining actual or even imagined control over one's experiences. Empowerment has been shown to have a positive impact on a person’s mental and physical health. In particular, women, and within that group, senior citizens, have been helped by empowerment interventions and a related concept, active aging. Findings indicate that empowerment for women leads to healthier lives and further research in this area is strongly encouraged, especially for identifying which type of woman is most likely to be affected. In the present study, this concept was applied to a group of ultra-orthodox Jewish women aged 55 and over who were encouraged to attend health promoting activities in a community center. A careful examination of the relevant literature did not reveal previous empirical research with this group. The study hypotheses focused on testing whether attendance at the community center creates benefits medically, psychologically, and, especially, a change in participants’ overall well-being.
Scales for measuring loneliness, depression, and well-being were administered to these women when they joined the program and follow-up testing was planned periodically. Analysis of pre-test data for participants who completed all the protocols (N=43) showed that, as expected, well-being was significantly correlated with loneliness (-0.38) and depression (-0.39) evaluation using the temperature-dependent photovoltaic power and the reference power ratio measured at standard test conditions is suggested. In other publications, the total increase in efficiency is measured. This makes it impossible to compare the cooling methods and to assess the application reasonability of the cooling systems and the gained benefit of each employed system. Thus there is a need for a universal value or criterion to assess the effectivity of the given cooling method and technique.
Incorporating the needs of at-risk populations into national health care initiatives is essential. Israel has identified ultra-Orthodox Jewish, or Haredi, women, as at risk of increased morbidity and mortality, yet actual data on this insular community are lacking. We reviewed published research on Israeli Haredi women’s health status, behaviors and health care access and examined methodologies. If providers and health care systems are not working together to provide culturally competent care, patients may have untoward health consequences, receive poor quality care, and be dissatisfied with the care they receive. The quality of patient-health professional interactions is decreased. Lower-quality patient-health professional interactions are associated with decreased satisfaction in the healthcare provider. In fact, African Americans, Asian Americans, Latinos, and Muslims report that the quality of their care was diminished because of their ethnicity or race.
Why are religion and spirituality important in healthcare? Religion and spirituality are important factors in the majority of patients seeking care. Unfortunately, health providers may not take religious beliefs into account when they are dealing with difficult medical decisions for patients and their families.
In the history of man, religious leaders and health providers were often the same. Only within recent times has medicine taken on a scientific approach that has resulted in a separation between medicine and religion.
The challenge for health professionals is in understanding that patients often turn to their religious and spiritual beliefs when making medical decisions. Religion and spirituality can impact decisions regarding diet, medicines based on animal products, modesty, and the preferred gender of their health providers. Some religions have strict prayer times that may interfere with medical treatment.
Healthcare providers should be respectful of a patient’s religious and spiritual needs. Many patient’s anxieties are reduced when they turn to their faith during healthcare challenges. Because many patients turn to their beliefs when difficult healthcare decisions are made, it is vital for healthcare professionals to recognize and accommodate the patient's religious and spiritual needs. Health professionals should provide an opportunity for patients to discuss their religious and spiritual beliefs and tailor their evaluation and treatment to meet their specific needs.
Published Date: 2020-11-28;