Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- The Global Impact Factor (GIF)
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
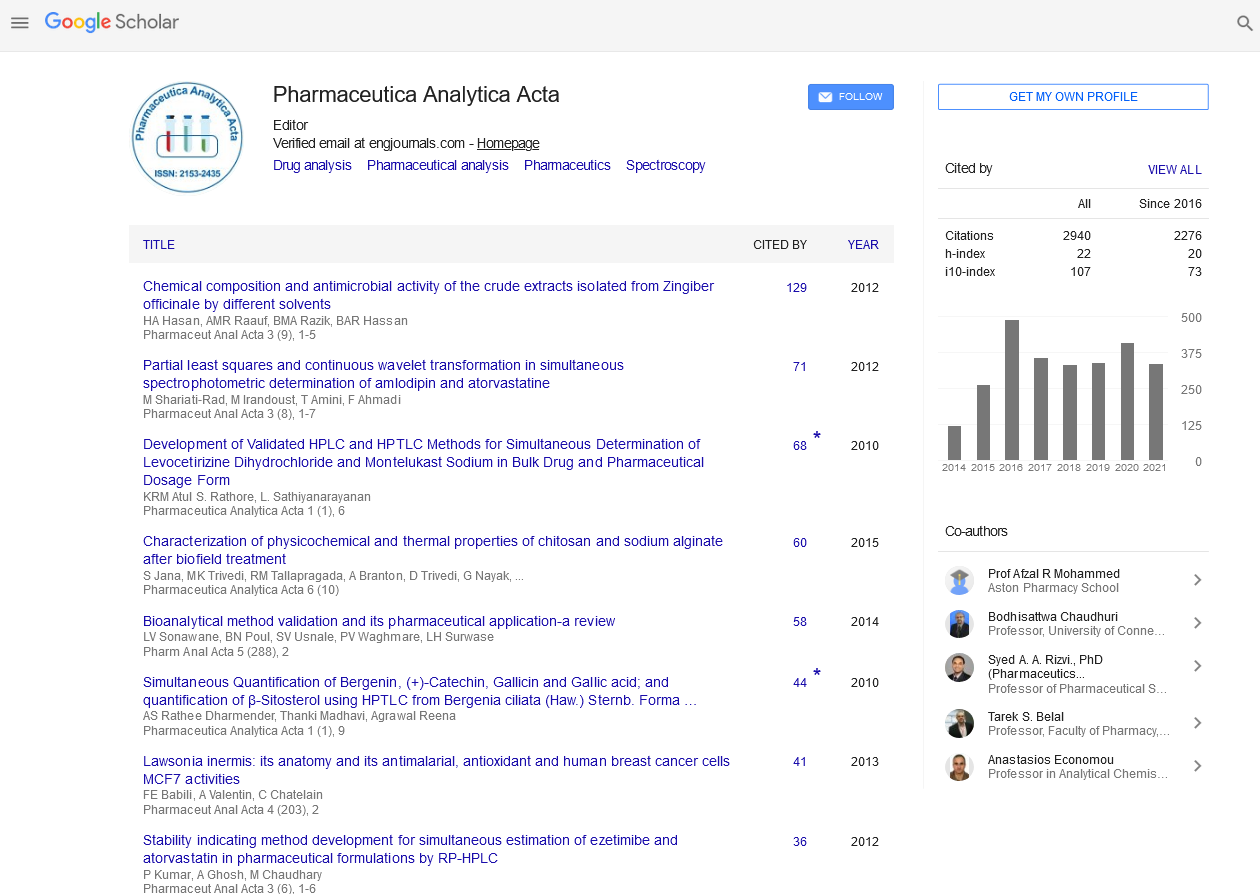
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Optimizing Antibiotic Pharmacodynamics for Clinical Practice
Kevin P Connors, Joseph L Kuti and David P Nicolau
With an absence of new antibiotics in the pipeline to address increasing resistance among gram-positive and gram-negative bacteria, new strategies are needed to retain utilization of currently available agents. As recommended in current guidelines for antimicrobial stewardship, dosage optimization through consideration of antibiotic pharmacodynamics provides a formidable approach to making good antibiotics better. Knowledge of the relationship between antibiotic concentration to microbiological potency and its effect on antibacterial activity leads to the design of dosing regimens that optimize killing of bacteria in the clinical setting. The activity of aminoglycosides is dependent on maximizing peak free drug concentrations in relation to their minimum inhibitory concentration (MIC), so giving larger doses less frequently has become the gold-standard strategy for optimizing their pharmacodynamics. In contrast, the activity of ?-lactam antibiotics is dependent on maximizing the time that free drug concentrations remain above the MIC; numerous approaches including continuous and prolonged infusion of these agents enable optimization of this pharmacodynamics parameter and improve clinical outcomes. This review discussed pharmacodynamics concepts as applied clinically for aminoglycosides, ?-lactams, and other classes of antibiotics.