Indexed In
- Open J Gate
- Genamics JournalSeek
- ResearchBible
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
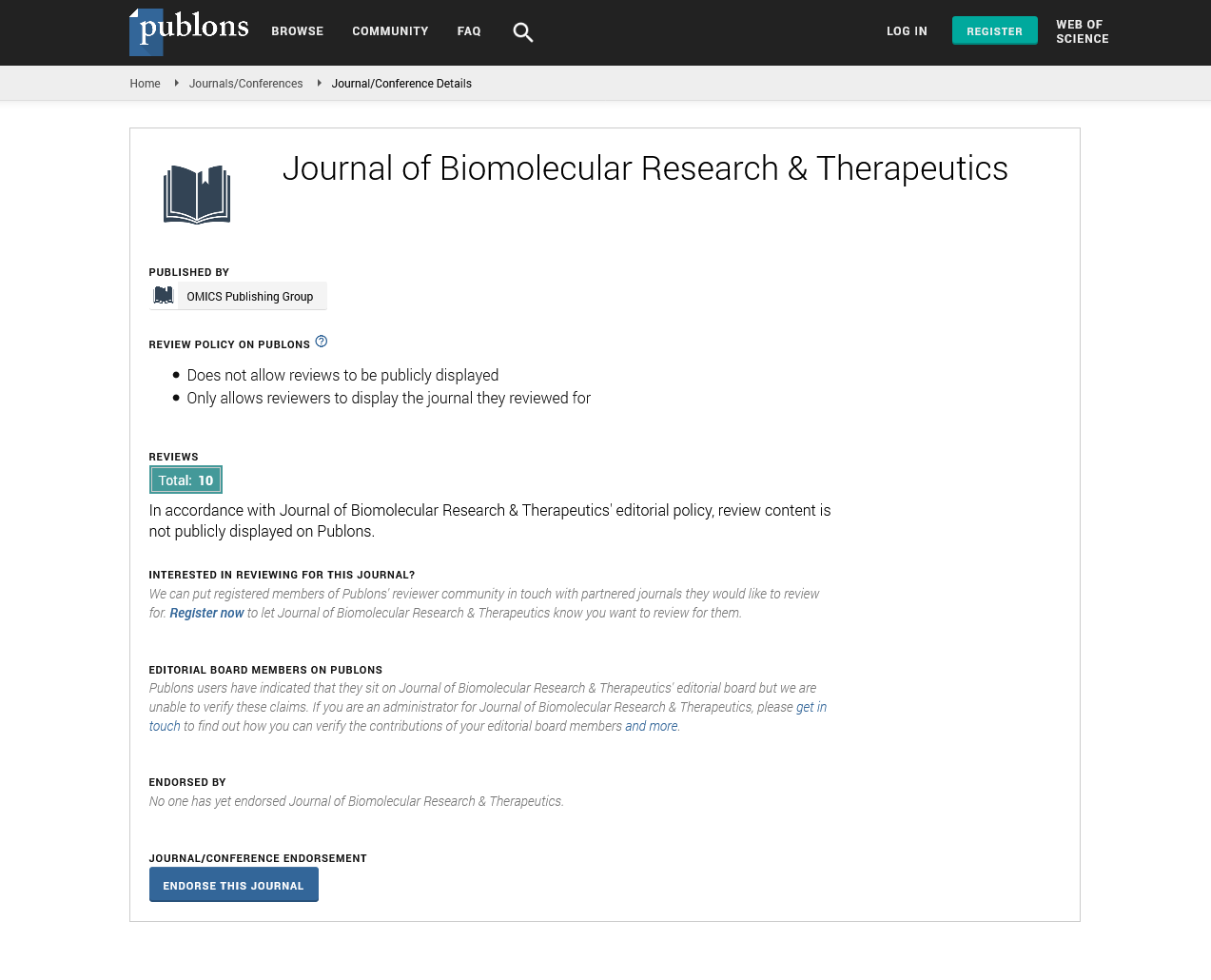
- Publons
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Opinion - (2025) Volume 14, Issue 2
The Role of Biomarkers in Personalized Cancer Therapy
Chen Wei*Received: 28-Mar-2025, Manuscript No. BOM-25-29598; Editor assigned: 31-Mar-2025, Pre QC No. BOM-25-29598; Reviewed: 14-Apr-2025, QC No. BOM-25-29598; Revised: 19-Apr-2025, Manuscript No. BOM-25-29598; Published: 28-Apr-2025, DOI: 10.35248/2167-7956.25.14.438
Description
The identification and use of biomarkers have become central to the advancement of personalized cancer therapy. Biomarkers are measurable biological indicators that can reflect the presence, progression, or response to treatment of a disease. In oncology, biomarkers help clinicians tailor treatment strategies to individual patients, improving efficacy while reducing unnecessary side effects.
Molecular biomarkers such as genetic mutations and gene expression patterns provide critical insights into tumor biology. For instance, mutations in the epidermal growth factor receptor have been associated with responsiveness to tyrosine kinase inhibitors in lung cancer patients. Similarly, HER2 amplification in breast cancer guides the use of targeted monoclonal antibodies that specifically inhibit tumor growth.
In addition to genetic markers, protein-based biomarkers provide valuable diagnostic and prognostic information. Elevated levels of prostate-specific antigen are commonly used in the early detection and monitoring of prostate cancer. Meanwhile, circulating tumor markers such as Carcinoembryonic Antigen and CA-125 assist in tracking disease progression and treatment response across different types of cancers.
The advent of liquid biopsy technology has further revolutionized biomarker detection. Liquid biopsies analyze circulating tumor DNA and other components in blood samples, offering a non-invasive alternative to traditional tissue biopsies. This enables real-time monitoring of tumor evolution and resistance mechanisms, allowing clinicians to adjust treatments more effectively.
Biomarkers also guide immunotherapy approaches. Programmed death-ligand 1 expression is used to predict patient response to checkpoint inhibitors, a class of drugs that reinvigorate immune cells to attack tumors. Identifying patients likely to respond enhances the efficiency of immunotherapy and spares others from unnecessary exposure to costly and potentially toxic treatments.
Challenges remain in standardization and validation of biomarkers across diverse patient populations. Variability in laboratory techniques, sample quality and interpretation can affect reliability. Collaborative international efforts are underway to establish guidelines that ensure consistency and clinical utility.
The integration of biomarkers into clinical practice is advancing rapidly due to progress in genomic sequencing and proteomics. These technologies provide comprehensive molecular profiles of tumors, enabling clinicians to match therapies more precisely. As databases expand and computational tools improve, the predictive power of biomarkers will continue to strengthen personalized cancer therapy.
Biomarker-driven treatments represent a shift toward individualized medicine, where decisions are guided by the unique molecular characteristics of each patient’s tumor. By aligning therapeutic choices with biological evidence, oncology is moving closer to delivering treatments that maximize benefit while minimizing harm.
Beyond their established role in diagnosis and therapeutic guidance, biomarkers are increasingly being employed in early cancer detection and risk assessment. Advances in high-throughput screening methods have identified biomarker signatures capable of detecting malignancies at very early stages, often before symptoms arise. For example, panels of circulating microRNAs and methylated DNA fragments are under investigation as tools for screening high-risk populations, potentially enabling earlier intervention and improved survival rates.
Moreover, biomarkers have become essential in monitoring Minimal Residual Disease (MRD) the small number of cancer cells that may remain after treatment and cause relapse. Sensitive detection of MRD through biomarkers allows for timely therapeutic adjustments, increasing the chances of sustained remission. This is particularly relevant in hematologic malignancies, where MRD-guided treatment decisions are now part of clinical protocols.
Personalized biomarkers also play a critical role in overcoming drug resistance, one of the most significant hurdles in cancer therapy. Tumors often evolve mechanisms to evade targeted treatments, such as acquiring secondary mutations or activating alternative signaling pathways. Serial biomarker assessments through liquid biopsies enable the identification of these resistance mechanisms in real-time, guiding clinicians to switch or combine therapies before clinical progression becomes evident.
In the research arena, the discovery of novel biomarkers is accelerating due to advances in multi-omics approaches, integrating genomics, transcriptomic, proteomics and metabolomics data. These comprehensive analyses reveal complex networks driving tumor behavior and uncover previously unknown biomarkers that could serve as new therapeutic targets or predictors of response.
Lastly, patient-derived organoids and xenograft models that replicate individual tumor biology allow functional testing of treatments based on biomarker profiles. This innovative approach provides an additional layer of personalization, potentially predicting drug efficacy in a patient-specific context before administering therapy.
As biomarker science evolves, it continues to transform oncology into a truly personalized discipline. The ongoing integration of cutting-edge technologies and collaborative efforts promises to enhance early detection, improve treatment outcomes and reduce toxicities, ultimately offering patients more precise and effective cancer care.
Citation: Wei C (2025). The Role of Biomarkers in Personalized Cancer Therapy. 14.438
Copyright: © 2025 Wei C. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.