Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Proquest Summons
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2025) Volume 16, Issue 1
The Management of Placenta Accreta Spectrum with Internal Iliac Artery Balloon Occlusion: A Systematic Review and Meta-Analysis
Puvinathan D and Denise E. Jackson*Received: 11-Dec-2024, Manuscript No. JBDT-24-27886; Editor assigned: 13-Dec-2024, Pre QC No. JBDT-24-27886 (PQ); Reviewed: 27-Dec-2024, QC No. JBDT-24-27886; Revised: 03-Jan-2025, Manuscript No. JBDT-24-27886 (R); Published: 10-Jan-2025, DOI: 10.4172/2155-9864.25.16.612
Abstract
Background: Placenta Accreta Spectrum (PAS) is characterised by the invasion of the chorionic villi into the myometrium. It arises most commonly from previous Caesarean Sections (CS) in patients, wherein lower segment scars interrupt the decidualisation of the placenta when preparing for a foetus. Internal iliac artery balloon occlusion provides a way to block the blood flow to the uterus and in turn improve clinical outcomes for patients with PAS disorders. This review aims to determine the effectiveness of the balloon occlusion technique in reducing blood loss in patients with PAS, the resulting neonatal outcomes and the proportion of previous CS in PAS patients.
Methods: A systematic review was conducted by searching 4 databases for keywords. A meta-analysis was performed using OpenMeta-Analyst software using arscine transformed proportion, binary random effects and maximum likelihood, as well as RevMan web software, using a continuous, arm-level model.
Results: Fourteen eligible studies were included with data from a total of 927 patients. A statistically significant difference was found for all analyses. A decreased amount of estimated blood loss was found in the balloon group against the control group, neonates were found to have higher 5’ Apgar scores in the control group rather than the balloon group and a majority of patients were found to have had at least one previous caesarean section.
Conclusion: This review provides evidence that the balloon occlusion technique can provide PAS patients with better clinical outcomes in relation to the amount of blood lost during delivery.
Keywords
Internal iliac artery balloon occlusion; Procedure-related complications; Estimated blood loss; Caesarean section complications
Introduction
Background
PAS also known as Morbidly Adherent Placenta (MAP) or Abnormal Invasive Placenta (AIP), is a placental abnormality characterised by the abnormal invasion of placental chorionic villi into the myometrium [1]. The classifications of this spectrum of disorders have been misunderstood over time but have been redefined by Luke in 1966Background PAS also known as Morbidly Adherent Placenta (MAP) or Abnormal Invasive Placenta (AIP), is a placental abnormality characterised by the abnormal invasion of placental chorionic villi into the myometrium [1]. The classifications of this spectrum of disorders have been misunderstood over time but have been redefined by Luke in 1966 wherein the recognised [2]. The characteristics for each are distinctly PAS disorders are divided into three subcategories: placenta accreta, placenta increta and placenta percreta [1]. Placenta accreta is defined as the contact of the placental chorionic villi with the myometrium, without intervening the decidua layer which is located between the myometrium and the intervillous space [1-3]. The invasion of the chorionic villi into the myometrium is known as placenta increta, while placenta percreta is the penetration of the chorionic villi into the uterine serosa [1-3].
The underlying pathophysiology behind PAS has led to many theories; the most prevalent theory being the failure of the decidualisation of the endometrium in preparation for the foetus to allow an abnormally deep trophoblastic infiltration [4]. It is believed that instead of the decidua separating the chorionic villi from the uterine myometrium, as the placenta implants itself within the maternal uterine decidua layer and myometrium, the cytotrophoblast cells begin to detach themselves from the villi to invade the decidual stroma [4,5]. It is reported that a key histological feature of the development of placenta accreta is the total or partial absence of the decidua wherein the decidua is replaced by loose connective tissue [4].
The infiltration of the chorionic villi into the myometrium can cause significantly life-threatening effects to the patient [3]. Due to the adverse effects which may be caused by this abnormality, it is important to ensure that the management of these patients prior to, during and post-delivery are carefully considered to ensure minimal harm to the patient and the foetus.
As the prevalence of placenta accreta spectrum increases globally, it is important to provide patients with appropriate care in order to ensure that the outcome of pregnancies remains positive. In a 2005 study conducted in the United States by Wu et al., it was found that analysing cases from 1982-2002 the overall incidence of placenta through accreta was 1 in 533 [6]. In comparison, a 1997 study conducted by Miller et al., of placenta accreta cases between 1985 and 1994 stating that the overall incidence during this period was found to be 1 in 2510, resulting in as much as a 10-fold rise in the prevalence in many Western countries [5,7]. As these numbers increase, it is significant to have prepared a proper plan for the management of delivery in PAS cases to ensure that patient blood loss is kept to a minimum and ensure patient safety.
Risk factors
Previous caesarean sections have been shown to increase the likelihood of developing placenta accreta, along with the existence of placenta praevia supporting the theory that the biological dysfunction of the endometrium may result from the previous uterine scar of the lower segment [4,8,9]. With each respective caesarean delivery, the risk of developing placenta accreta substantially increases, with up to 88% of placenta accreta patients in a study already having existing placenta praevia [9]. Wu et al., demonstrated an 8-fold increased risk of placenta accreta occurring in patients with at least 2 caesarean section scars in comparison to patients who have not had a caesarean section [6,10]. It has also been demonstrated that the risk for placenta accreta increases with the existence of placenta praevia, as seen in a 2006 study by Silver et al, which stated that of 723 women with placenta praevia, the risk for placenta accreta was 3%, 11%, 40%, 61% and 67% for the first, second, third, fourth and fifth or more repeat caesarean deliveries [11].
Additional factors have been observed; specifically advanced maternal age, as well as other factors such as multiparity and previous uterine curettage. Asherman’s syndrome, smoking, chronic hypertension, endometriosis, manual removal of the placenta, myomectomy, hysteroscopic surgery, IVF procedures, adenomyosis and submucous fibroids have also been observed as risk factors for placenta accreta [4,6,12].
Internal iliac artery balloon occlusion
The internal iliac artery is located in the lower abdomen where it branches from the common iliac artery into internal and external iliac arteries; from here, the internal iliac artery serves as the main blood supply for the uterus as the uterine artery branches to supply the uterus [13]. The placement of a balloon in the internal iliac artery for caesarean deliveries allows for blockage of the primary blood supply to the uterus resulting in a reduced pressure through the uterine artery [14]. This can in turn assist during delivery by providing a clearer view of the area, as well as reducing the duration of the surgery and allowing for additional time for amending the operative plan if necessary to provide safer and well-designed care for the patient [14].
Scope of the review
Placenta accreta spectrum is a dangerous abnormality which can cause serious harm to both the mother and the foetus during delivery. In order to reduce the significant ramifications that could occur due to this abnormal placenta, internal iliac artery balloon occlusion may serve as an efficient way to reduce the amount of blood lost during delivery, while simultaneously providing medical professionals with additional time to make decision concerning the safety of the patient and foetus.
The aim of this study was specified using the Population, Intervention, Comparator and Outcome (PICO) framework, in which elements of the question are related back to PICO [15].
The aim of this study was to determine: Does internal iliac artery balloon occlusion (intervention) provide a way to reduce blood loss (outcome) during delivery in patients with placenta accreta spectrum (population) rather than standard caesarean delivery (comparator)?
This study evaluates the estimated blood loss of patients to determine if the ballon occlusion technique has allowed for an efficient blockage of the internal iliac artery to minimize unneccessary bleeding. It will also cover whether a previous caesarean section was observed in these cases.
Materials and Methods
Study design
In this systematic review, the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) procedure was implemented in order to gather articles for the investigation of the efficacy of using balloon occlusion devices for patients with placenta accreta spectrum [16].
Study search and selection
The search for relevant articles was done through PubMed, Scopus, Embase and ProQuest databases, with no restriction of time. Search terms used included “MTP activation”, “massive transfusion”, “traumatic haemorrhage” and “traumatic hemorrhage”.
Eligibility criteria
The eligibility criteria of articles obtained was determined through inclusion or exclusion criteria which were predetermined. Articles which investigated the management of placenta accreta spectrum through the use of balloon catheters were deemed eligible. Criteria for exclusion consisted of, a) Lack of full text article; b) Non-English publications; c) Articles which had not commenced recruiting of participants; d) Were not relevant to the research question asked.
Assessment of methodological quality
The studies selected were assessed based on the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) checklist for their methodological quality [17].
Data extraction
Data was extracted from the eligible studies with the author, publication year, country, study design, study period, study size and the parameters which were analysed. The parameters measured included estimated blood loss, previous caesarean section and neonatal outcomes. In articles which placenta accreta, increta and percreta were measured separately, only placenta accreta data was used.
Statistical analysis
To complete the meta-analysis, the Review Manager (Rev Man) web software was used for two-armed proportion analyses and is available on the Cochrane website, along with OpenMeta-Analyst software-used for one-armed proportion analysis – and was downloaded from the Brown University website [18,19]. A two-arm analysis was completed for the comparison of the estimated blood loss, neonatal outcomes and other injuries obtained between the study group and the control group. A one-armed analysis was used for the measurement of caesarean sections present in PAS patients. The one-armed analysis was measured using arscine transformed proportion, binary random effects and maximum likelihood method [20]. The results were presented in a forest plot format, with calculated p-values for the measurement of statistical significance, a 95% confidence level along with its respective p-value for the measurement of heterogeneity. The calculated p-value was considered as statistically significant if a value of <0.05 was observed [21-25].
Results
Study selection
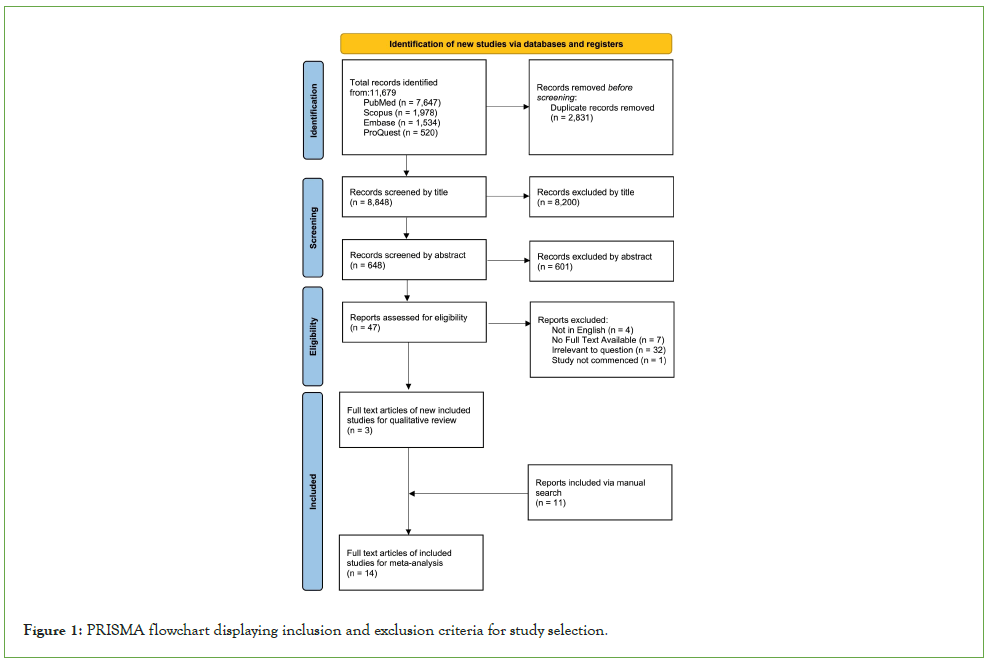
Study selection based on inclusion/exclusion criteria can be seen in (Figure 1). Through the database search, a total of 11,679 studies for screening. After removal of 2,832 duplicate articles, a total of 8,848 studies remained [25-27]. The studies were screened based on title and abstract where 8,200 and 601 studies were removed, respectively. Of the remaining 47 studies which were assessed for eligibility, 44 studies were removed based on the exclusion criteria of non-English publications, lack of full text availability, irrelevance to question and had not commenced recruiting for the trial. After exclusions, 3 studies remained which matched the eligibility criteria; following the addition of 11 studies via manual search, a total of 14 studies were included in the meta-analysis [27-30].
Figure 1: PRISMA flowchart displaying inclusion and exclusion criteria for study selection.
Study characteristics
The characteristics of each of the 14 studies are shown in (Table 1) wherein 12 of the 14 studies measure the estimated blood loss which occurred during the procedure (Table 1). Ten of the 14 studies highlighted the presence of a previous caesarean section which may have contributed to the development PAS patients. Six of the 14 studies report on the outcomes of the neonates after delivery. The majority of these studies had a retrospective study design wherein the study period ranged from 1991-2022 and were located across nine countries. The total sample size of the studies ranged from 6-163 [31].
| Study | Year | Country | Study Design | Study period | Study size | Parameters measured |
|---|---|---|---|---|---|---|
| Abouda et al. [20] | 2024 | Tunisia | Retrospective | 2020-2022 | 38 | Estimated blood loss and previous CS |
| Angileri et al. [21] | 2017 | Italy | Prospective | 2010-2016 | 37 | Previous CS |
| Cali et al. [22] | 2014 | Italy | Prospective | 2004-2009 | 53 | Estimated blood loss, previous CS and neonatal outcomes |
| Chen et al. [23] | 2020 | China | Prospective | 2017-2018 | 100 | Estimated blood loss and previous CS |
| Cho et al. [24] | 2020 | South Korea | Retrospective | 2010-2019 | 42 | Estimated blood loss and neonatal outcomes |
| Chou et al. [25] | 2003 | Taiwan | Prospective | 1999-2002 | 6 | Previous CS |
| Fan et al. [26] | 2017 | China | Prospective | 2015-2017 | 163 | Estimated blood loss, previous CS and neonatal outcomes |
| Overton et al. [27] | 2022 | USA | Retrospective | 2018-2020 | 30 | Estimated blood loss |
| Peng et al. [14] | 2020 | China | Retrospective | 2016-2019 | 104 | Estimated blood loss |
| Picel et al. [28] | 2018 | USA | Retrospective | 1991-2017 | 151 | Estimated blood loss and previous CS |
| Rosner-Tenerowicz et al. [29] | 2021 | Poland | Retrospective | Prior to 2021 | 29 | Estimated blood loss and previous CS |
| Savukyne et al. [30] | 2021 | Lithuania | Retrospective | 2016-2019 | 66 | Estimated blood loss, previous CS and neonatal outcomes |
| Tan et al. [1] | 2007 | Singapore | Retrospective | 2004-2005 | 25 | Estimated blood loss |
| Zhou et al. [31] | 2019 | China | Retrospective | 2014-2017 | 83 | Estimated blood loss and previous CS |
Note: CS: Caesarean Section
Table 1: Characteristics of eligible studies for the analysis of internal iliac artery balloon occlusion in patients with placenta accreta spectrum.
The data used for the meta-analysis can be seen in (Table 2). Mean and standard deviation data for estimated blood loss was obtained from each study; when data was unavailable, it was estimated through calculations proposed by Wan et al., wherein the mean and standard deviation of data are estimated based on the available values of median, range and sample size [32]. When measuring PAS patients with a previous caesarean section, the number of patients with a previous caesarean section was used to compare against the total number of patients in the study. Data for neonatal outcomes measures the Apgar score of the newborns after 5 minutes; the mean and standard deviation were used for the data. One study had a calculated standard deviation which was determined through the equation proposed by Wan et al., for determining the standard deviation [30,32].
| Study | Year | N | Mean Estimated Blood Loss (mL) a | PAS patients with a previous CS d | Neonatal outcomes (Apgar score) e |
|---|---|---|---|---|---|
| Abouda et al. [20] | 2024 | 16/38 | 1828 ± 324/2888 ± 863 c | 35/38 | - |
| Angileri et al. [21] | 2017 | 37 | - | 28/37 | - |
| Cali et al. [22] | 2014 | 30/53 | 846.67 ± 280.06/1156.52 ± 576.69 | 53/53 | 8.8 ± 0.41/8.65 ± 0.98 |
| Chen et al. [23] | 2020 | 50/100 | 2630 ± 1585/2221 ± 1694 | 100/100 | - |
| Cho et al. [24] | 2020 | 17/42 | 2319 ± 875/4425 ± 2250c | - | 8.1 ± 0.5/8.5 ± 0.75 |
| Chou et al. [25] | 2003 | 6 | - | 6/6 | - |
| Fan et al. [26] | 2017 | 74/163 | 1236 ± 138.2/1694 ± 144.3 | 163/163 | 7.4 ± 0.2/7.1 ± 0.2 |
| Overton et al. [27] | 2022 | 10/30 | 1425 ± 1000/1170 ± 750c | - | - |
| Peng et al. [14] | 2020 | 48/104 | 1504.17 ± 1123.44/1108.04 ± 1008.32 | - | - |
| Picel et al. [28] | 2018 | 90/151 | 2360 ± 1620/3290 ± 2710 | 134/151 | - |
| Rosner-Tenerowicz et al. [29] | 2021 | 15/29 | 1800 ± 1025/2342.85 ± 1050 b, c | 23/29 | - |
| Savukyne et al. [30] | 2021 | 19/66 | 1257.90 ± 1525/1072.34 ± 1150 b, c | 38/66 | 8.90 ± 1/8.98 ± 0.75 b |
| Tan et al. [1] | 2007 | 11/25 | 2011 ± 1150/3316 ± 750c | - | - |
| Zhou et al. [31] | 2019 | 58/83 | 1215 ± 72.57/1602 ± 862.47 | 83/83 | - |
Note: N is presented as total in study group, or total in balloon group/total in study. a Mean of balloon group only, or mean of balloon group ± standard deviation/mean of control gro/standard deviation; b Mean was estimated though calculations [32]; c Standard deviation was estimated through calculations [32]; d PAS patients number with one or more CS/total number of PAS patients (PAS-Placenta Accreta Spectrum; CS-Caesarean Section); e Neonatal outcomes are presented as an Apgar score at 5 minutes (5’).
Table 2: Summary data of eligible studies included in meta-analysis of mean preoperative, intraoperative and post-operative outcomes.
Methodological quality assessment
All studies included in this analysis underwent assessment through the STROBE checklist to evaluate their methodological company; this can be seen in (Table 3). All included studies had clear titles and abstract, along with introductions that provided adequate information regarding the background and rationale of the procedure. All studies had sufficient details in reference to their study methods, however two studies had limited information regarding the selection of their participants [25,29]. One study had described the statistical methods in their discussion section rather than their methods section and one study had failed to mention their statistical methods at all [20,25]. The 14 studies were successful in describing the study participant characteristics; the majority of studies were found to be successful in regard to discussing significant limitations of their study, however one study had failed to mention any limitations [29]. The major limitation mentioned was the small sample size of the studies. The retrospective nature of the trials was also mentioned, resulting in an unavoidable bias when selecting participants, along with the single-centre focus for certain studies.
| Year | Title and abstract | Introduction | Methods | Results | Discussion | |||
|---|---|---|---|---|---|---|---|---|
| Clear title and abstract with study design indicated | Explains scientific background and rationale | Details study methods | Eligibility criteria and selection of participants provided | Describe statistical methods | Give characteristics of study participants | Summarises key results and discusses potential limitations | ||
| Abouda et al. [20] | 2024 | Y | Y | Y | Y | N d | Y | Y |
| Angileri et al. [21] | 2017 | Y | Y | Y | Y | Y | Y | Y |
| Cali et al. [22] | 2014 | Y | Y | Y | Y | Y | Y | Y |
| Chen et al. [23] | 2020 | Y | Y | Y | Y | Y | Y | Y |
| Cho et al. [24] | 2020 | Y | Y | Y | Y | Y | Y | Y |
| Chou et al. [25] | 2003 | Y | Y | Y | Y c | Y b | Y | Y |
| Fan et al. [26] | 2017 | Y | Y | Y | Y | Y | Y | Y |
| Overton et al. [27] | 2022 | Y | Y | Y | Y | Y | Y | Y |
| Peng et al. [14] | 2020 | Y | Y | Y | Y | Y | Y | Y |
| Picel et al. [28] | 2018 | Y | Y | Y | Y | Y | Y | Y |
| Rosner-Tenerowicz et al. [29] | 2021 | Y | Y | Y | Y c | Y | Y | N a |
| Savukyne et al. [30] | 2021 | Y | Y | Y | Y | Y | Y | Y |
| Tan et al. [1] | 2007 | Y | Y | Y | Y | Y | Y | Y |
| Zhou et al. [31] | 2019 | Y | Y | Y | Y | Y | Y | Y |
Note: Y-criteria fulfilled; N-criteria not fulfilled. a No limitations discussed; b Mentioned in Discussion; c Limited information; d No statistical methods discussed.
Table 3: Evaluation of studies included in meta-analysis according to the STROBE (Strengthening the Reporting of observational studies in epidemiology) checklist.
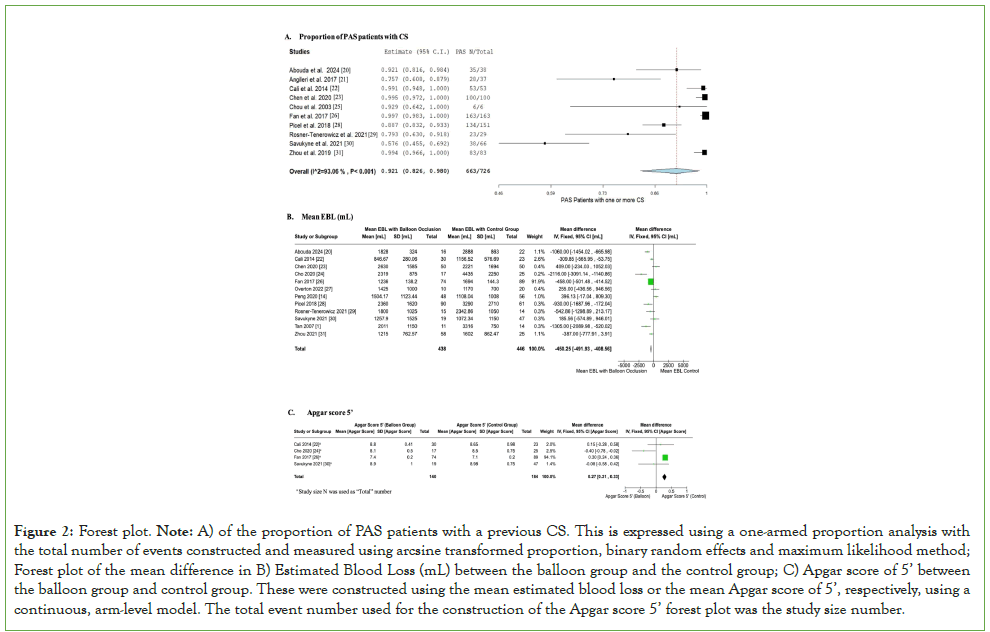
Meta-analysis on the proportion of Caesarean section in PAS patients
A one-arm proportion analysis was conducted for the PAS patients with one or more previous caesarean section. The analysis was carried out on 10 of the 14 studies which highlight data for previous caesarean sections in patients with placenta accreta spectrum. The data used for the analysis can be seen in Table 2. The forest plot constructed, which can be seen in Figure 2A, has a statistically significant p-value of <0.001. The heterogeneity showed an I2 of 93.06% and a p-value of <0.001. The upper bound was 0.980 and the lower bound was 0.826, with a 95% CI. The high heterogeneity of this plot suggests a high amount of variability within the data. The overall point estimate was 92.1% with a total of 663 of the 726 patients analysed having had at least one previous caesarean section.
Meta-analysis on the proportion of estimated blood loss and neonatal outcomes
A meta-analysis was performed and a forest plot was created on the mean difference of Estimated Blood Loss (EBL) between the balloon occlusion group and control group of each respective study. Of the studies included, 12 of the 14 studies were used for this analysis; the data used for this analysis can be seen in Table 2. The forest plot constructed, which can be seen in Figure 2B, is a two-arm proportion analysis that was found to be statistically significant with a p-value of <0.001. The mean difference between the balloon groups and the control groups was found to be -450.25, with an upper bound of -408.56 and a lower bound of -491.93. The CI was 95%. The heterogeneity was found to have a p-value of <0.001 and an I2 of 81%; this high heterogeneity signifies a large amount of variation in the data. The plot shows more favour towards the balloon occlusion arm and most of the data lies to the left of the line of null effect.
Figure 2: Forest plot. Note: A) of the proportion of PAS patients with a previous CS. This is expressed using a one-armed proportion analysis with the total number of events constructed and measured using arcsine transformed proportion, binary random effects and maximum likelihood method; Forest plot of the mean difference in B) Estimated Blood Loss (mL) between the balloon group and the control group; C) Apgar score of 5’ between the balloon group and control group. These were constructed using the mean estimated blood loss or the mean Apgar score of 5’, respectively, using a continuous, arm-level model. The total event number used for the construction of the Apgar score 5’ forest plot was the study size number.
Similarly, a two-arm proportion analysis was performed for the neonatal outcomes on the newborns. The mean difference of Apgar scores of 5 minutes was compared between the balloon group and the control group. This analysis was conducted with the data from four of the 14 studies. The data used for the analysis can be seen in Table 2. The forest plot constructed, which can be seen in Figure 2C, showed a statistically significant result of a p-value <0.001. The heterogeneity was an 80% I2 with a p-value of 0.002, indicating a high variability between the data. The mean difference of the data was found to be 0.27, with an upper bound of 0.33 and a lower bound of 0.21. The CI was 95%. The black diamond on the plot shows more favour towards the control, as it lies to the right of the line of null effect (Figure 2).
Discussion
PAS Patients with previous caesarean section
The analysis of the proportion of placenta accreta spectrum patients with one or more previous caesarean section provided a statistically significant result of <0.001, along with the overall point result of 92.1% as 663 of the 726 patients had had a previous caesarean section. The heterogeneity provided a p-value of <0.001 and an I2 of 93.06%, demonstrating high variability between the data used in the analysis; due to this high variability, the conclusions drawn from the data obtained may not be certain. The blue diamond which represents the pooled effect of all of the data, as well as the horizontal points of the diamond which represent the 95% confidence interval. There are two studies which fall completely out of this 95% confidence interval and are therefore outliers which are unlikely to be representative of true values [26,30]. The weighting of each of the studies in the analysis was fairly consistent, with nine of the 10 studies all having a weighting between 9% and 11%; one study had a weighting of 6.5% possible due to the small sample size of the study [25]. It was found that a majority of the patients in the studies had a history of a previous caesarean section which will greatly contribute to the development of the placenta accreta spectrum subtypes. A majority of the patients in the study had only had one previous caesarean section rather than more than one; the least number of patients had had no previous caesarean sections. Overall, based on this analysis, it is likely that previous caesarean sections will contribute to the development of placenta accreta spectrum in patients.
Estimated blood loss in placenta accreta spectrum
The mean difference between the control and balloon groups for estimated blood loss was found to be -450.25. Therefore, the analysis of the estimated blood loss between the balloon occlusion groups and the control groups shows more favour towards the experimental (balloon occlusion). The black diamond on the plot also lies to the left of the line of null effect, indicating a favour towards the use of balloon occlusion in patients with placenta accreta spectrum. The studies had a high amount of heterogeneity within the data with an I2 of 81% and a p-value of <0.001. This signifies a large amount of variation between the data due to issues other than chance and may possibly result in uncertain conclusions drawn from the data. As the standard deviation for one study conducted was substantially lower than other studies used in the analysis, with Fan et al., having a standard deviation of 138.2 and 144.8 for the balloon and control groups, respectively, it resulted in a weighting of 91.9% in comparison to the remaining studies which all each had a weighting of less than 3% due to their standard deviations ranging from 280.06 to 1620 in the balloon group and 576.69 to 2710 for the control group [26]. This may have skewed the data towards favouring the balloon. Overall, the data from conducting this analysis demonstrates a decreased amount of blood loss within the balloon group in comparison to the control group by favouring the balloon group. By using the balloon catheter technique for placenta accreta spectrum patients, it can provide a better clinical outcome for patients during delivery by reducing the need for transfusion due to excess blood loss.
Effect of balloon occlusion on neonatal outcomes
Apgar scores, which measure the baby’s ability to adapt to the environment shortly after birth, provide a way to clinically assess the baby’s condition [33]. An Apgar score of 7 or greater at 5 minutes after birth demonstrates that a baby is able to adapt well to the new environment [33]. The neonatal outcomes analysis, which used the mean Apgar score at 5 minutes from each study, showed a minor difference in the balloon group against the control group. Although the p-value was statistically significant at <0.001, the mean difference of 0.27 demonstrates a small favouring for the control group over the balloon group. The black diamond lies to the right of the line of null effect, demonstrating more favour towards the control side, however due to the small number of studies used in this analysis, this data may be skewed. The largest weighted study which was conducted by Fan et al., had a weighting of 94.1%, whereas the remaining three studies each had a weighting of less than 3%; this may be another reason why this data is skewed towards the control [26]. The heterogeneity presented a p-value of 0.002 and an I2 of 80% which indicates that the data has a high amount of variability, which may result in uncertain conclusions. Overall, this analysis demonstrates that Apgar scores of 5 minutes were higher in the control group in comparison to the balloon group. In comparison, the balloon group and the control group both had mean Apgar scores of over 7, which demonstrates that all newborns in the analysis had a good ability to adapt well to the environment. The mean difference of 0.27 indicates that there was a small difference in the Apgar scores of the balloon group and the control group, however all neonates were within the healthy range.
Limitations
There are many limitations to this review; the major limitation being the small number of prospective studies which were able to be used for the analysis. As a majority of the studies were retrospective, it may begin to introduce some bias into the data which was collected.
The sample sizes of each study were consistently small and therefore may also interfere with the analysis by introducing variation and bias which would not otherwise be present in a larger sample size.
The high heterogeneity in all three of the analyses conducted indicate a large amount of variation within the data which may not be chance; this would lead to analyses in which conclusions may not be able to be accurately drawn as the data may be inaccurate.
During collection of the data to conduct the analyses, there was a lack of mean data available as well as a lack in the standard deviations present which made it difficult to construct the forest plots; due to this, it was necessary to estimate the mean and the standard deviation through calculations using the median, minimum and maximum values and sample size. As a result, the data estimated from these studies may be inaccurate and provide an imprecise result of the true nature of the procedures.
Finally, the weighting of the studies in the neonatal outcomes and the estimated blood loss showed that the study by Fan et al., had the most weighting amongst all the studies at 94.1% and 91.9%, respectively [26]. This is due to the remaining studies having much more variation in their standard deviations and therefore, a larger 95% confidence interval.
Conclusion
This systematic review and meta-analysis present that balloon occlusion intervention in the iliac artery may be a suitable alternative for patients with placenta accreta spectrum to deliver rather than standard caesarean delivery. The estimated blood loss between the balloon group and the control group displayed that there was a significant difference between the two groups and therefore favoured the balloon group. This balloon technique can help to provide patients with a better clinical outcome during delivery by reducing the need for transfusion as a result of the reduced blood loss. When comparing the neonatal outcomes between the two groups for the Apgar scores at 5 minutes, there was favour towards the control group. This demonstrates that newborns were better adapted to the environment in standard caesarean delivery compared to a caesarean delivery with a balloon catheter intervention. However, as all neonates had shown a healthy Apgar score at 5 minutes, it indicates a small favour towards the control group. It was also discussed that Placenta Accreta Spectrum is more likely if the patient had already had a previous caesarean section; this was indicated by the caesarean history of the patients in the analysis wherein a majority of the patients had had at least one previous caesarean section prior to their placenta accreta spectrum diagnosis being made. This review provides evidence that the implementation of balloon occlusion catheters within the internal iliac artery will offer a way to substantially reduce the amount of blood lost during delivery in comparison to standard caesarean delivery. However, further research on the topic is highly encouraged to provide supplemental substantial evidence for the use of balloon occlusion catheters during delivery.
References
- Tan CH, Tay KH, Sheah K, Kwek K, Wong K, Tan HK, et al. Perioperative endovascular internal iliac artery occlusion balloon placement in management of placenta accreta. AJR Am J Roentgenol. 2007;189(5):1158-1163.
[Crossref] [Google Scholar] [PubMed]
- Luke RK, Sharpe JW, Greene RR. Placenta accreta: The adherent or invasive placenta. Am J Obstet Gynecol. 1966;95(5):660-668.
[Crossref] [Google Scholar] [PubMed]
- Konijeti R, Rajfer J, Askari A. Placenta percreta and the urologist. Rev Urol. 2009;11(3):173-176.
[Crossref] [Google Scholar] [PubMed]
- Jauniaux E, Jurkovic D. Placenta accreta: Pathogenesis of a 20th century iatrogenic uterine disease. Placenta. 2012;33(4):244-251.
[Crossref] [Google Scholar] [PubMed]
- Sellmyer MA, Desser TS, Maturen KE, Jeffrey RB, Kamaya A. Physiologic, histologic and imaging features of retained products of conception. Radiographics. 2013;33(3):781-796.
[Crossref] [Google Scholar] [PubMed]
- Wu S, Kocherginsky M, Hibbard JU. Abnormal placentation: Twenty-year analysis. Am J Obstet Gynecol. 2005;192(5):1458-1461.
[Crossref] [Google Scholar] [PubMed]
- Miller DA, Chollet JA, Goodwin TM. Clinical risk factors for placenta previa-placenta accreta. Am J Obstet Gynecol. 1997;177(1):210-214.
[Crossref] [Google Scholar] [PubMed]
- Boulton FE. Guidelines for transfusion for massive blood loss. A publication of the British Society for Haematology. British Committee for Standardization in Haematology Blood Transfusion Task Force. Clin Lab Haematol. 1988;10(3):265-273.
[Crossref] [Google Scholar] [PubMed]
- Armstrong CA, Harding S, Matthews T, Dickinson JE. Is placenta accreta catching up with us? Aust N Z J Obstet Gynaecol. 2004;44(3):210-213.
[Crossref] [Google Scholar] [PubMed]
- Petrov DA, Karlberg B, Singh K, Hartman M, Mittal PK. Perioperative internal iliac artery balloon occlusion, in the setting of placenta accreta and its variants: The role of the interventional radiologist. Curr Probl Diagn Radiol. 2018;47(6):445-451.
[Crossref] [Google Scholar] [PubMed]
- Silver RM, Landon MB, Rouse DJ, Leveno KJ, Spong CY, Thom EA, et al. Maternal morbidity associated with multiple repeat cesarean deliveries. Obstet Gynecol. 2006;107(6):1226-1232.
[Crossref] [Google Scholar] [PubMed]
- Sivan E, Spira M, Achiron R, Rimon U, Golan G, Mazaki-Tovi S, et al. Prophylactic pelvic artery catheterization and embolization in women with placenta accreta: Can it prevent cesarean hysterectomy? Am J Perinatol. 2010;27(6):455-461.
[Crossref] [Google Scholar] [PubMed]
- Selcuk I, Yassa M, Tatar I, Huri E. Anatomic structure of the internal iliac artery and its educative dissection for peripartum and pelvic hemorrhage. Turk J Obstet Gynecol. 2018;15(2):126-129.
[Crossref] [Google Scholar] [PubMed]
- Peng Y, Jiang L, Peng C, Wu D, Chen L. The application of prophylactic balloon occlusion of the internal iliac artery for the treatment of placenta accreta spectrum with placenta previa: A retrospective case-control study. BMC Pregnancy Childbirth. 2020;20(1):349.
[Crossref] [Google Scholar] [PubMed]
- Speckman RA, Friedly JL. Asking structured, answerable clinical questions using the Population, Intervention/Comparator, Outcome (PICO) framework. PM R. 2019;11(5):548-553.
[Crossref] [Google Scholar] [PubMed]
- Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1.
[Crossref] [Google Scholar] [PubMed]
- Skrivankova VW, Richmond RC, Woolf BAR, Davies NM, Swanson SA, VanderWeele TJ, et al. Strengthening the Reporting of Observational Studies in Epidemiology using Mendelian Randomisation (STROBE-MR): Explanation and elaboration. BMJ. 2021;375:2233.
[Crossref] [Google Scholar] [PubMed]
- The Cochrane Collaboration. Review Manager (RevMan). Version (8.7.0). 2024.
- Wallace BC, Dahabreh IJ, Trikalinos TA, Lau J, Trow P, Schmid CH. Closing the gap between methodologists and end-users: R as a computational back-end. J Stat Soft. 2012;49(5):1-15.
- Abouda SH, Aloui H, Jaouad H, Marzouk SB, Frikha H, Hammami R, et al. Prophylactic occlusion balloons of both internal iliac arteries in caesarean hysterectomy for placenta accreta spectrum disorder reduces blood loss: A retrospective comparative study. Eur J Obstet Gynecol Reprod Biol X. 2024;22:100310.
[Crossref] [Google Scholar] [PubMed]
- Angileri SA, Mailli L, Raspanti C, Ierardi AM, Carrafiello G, Belli AM. Prophylactic occlusion balloon placement in internal iliac arteries for the prevention of postpartum haemorrhage due to morbidly adherent placenta: Short term outcomes. Radiol Med. 2017;122(10):798-806.
[Crossref] [Google Scholar] [PubMed]
- Cali G, Forlani F, Giambanco L, Amico ML, Vallone M, Puccio G, et al. Prophylactic use of intravascular balloon catheters in women with placenta accreta, increta and percreta. Europ J Obstetric Gynecol Reproduct Biol. 2014;179:36-41.
[Crossref] [Google Scholar] [PubMed]
- Chen M, Liu X, You Y, Wang X, Li T, Luo H, et al. Internal iliac artery balloon occlusion for placenta previa and suspected placenta accreta: A randomized controlled trial. Obstet Gynecol. 2020;135(5):1112-1119.
[Crossref] [Google Scholar] [PubMed]
- Cho SB, Hong SJ, Lee S, Won JH, Choi HC, Ha JY, et al. Preoperative prophylactic balloon-assisted occlusion of the internal iliac arteries in the management of placenta increta/percreta. Medicina (Kaunas). 2020;56(8).
[Crossref] [Google Scholar] [PubMed]
- Chou MM, Hwang JI, Tseng JJ, Ho ESC. Internal iliac artery embolization before hysterectomy for placenta accreta. J Vasc Interv Radiol. 2003;14(9):1195-1199.
[Crossref] [Google Scholar] [PubMed]
- Fan Y, Gong X, Wang N, Mu K, Feng L, Qiao F, et al. A prospective observational study evaluating the efficacy of prophylactic internal iliac artery balloon catheterization in the management of placenta previa-accreta. Medicine. 2017;96(45).
[Crossref] [Google Scholar] [PubMed]
- Overton E, Booker WA, Mourad M, Moroz L, Nhan Chang C-L, Breslin N, et al. Prophylactic endovascular internal iliac balloon placement during cesarean hysterectomy for placenta accreta spectrum. Am J Obstet Gynecol MFM. 2022;4(5):100657.
[Crossref] [Google Scholar] [PubMed]
- Picel AC, Wolford B, Cochran RL, Ramos GA, Roberts AC. Prophylactic internal iliac artery occlusion balloon placement to reduce operative blood loss in patients with invasive placenta. J Vasc Interv Radiol. 2018;29(2):219-224.
[Crossref] [Google Scholar] [PubMed]
- Rosner-Tenerowicz A, Fuchs T, Pomorski M, Sliwa J, Zimmer-Stelmach A, Zimmer M. The clinical evaluation of internal iliac arteries balloon occlusion for placenta accreta spectrum. Ginekol Pol. 2021;92(3):210-215.
[Crossref] [Google Scholar] [PubMed]
- Savukyne E, Liubiniene L, Strelcoviene Z, Nadisauskiene RJ, Vaboliene E, Machtejeviene E, et al. Experience of managing suspected placenta accreta spectrum with or without internal iliac artery balloon occlusion in two lithuanian university hospitals. Medicina (Kaunas). 2021;57(4).
[Crossref] [Google Scholar] [PubMed]
- Zhou X, Sun X, Wang M, Huang L, Xiong W. The effectiveness of prophylactic internal iliac artery balloon occlusion in the treatment of patients with pernicious placenta previa coexisting with placenta accreta. J Matern Fetal Neonatal Med. 2021;34(1):93-98.
[Crossref] [Google Scholar] [PubMed]
- Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14(1):135.
[Crossref] [Google Scholar] [PubMed]
- Australian Institute of Health and Welfare. Canberra (Australia). Australian Institute of Health and Welfare; Australia's mothers and babies. 2024.
Citation: Puvinathan D, Jackson DE (2025). The Management of Placenta Accreta Spectrum with Internal Iliac Artery Balloon Occlusion: A Systematic Review and Meta-Analysis. J Blood Disord Transfus. 16:612.
Copyright: © 2025 Puvinathan D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.