Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review - (2019) Volume 4, Issue 1
The Impact of Microanatomy and Changing Physiology of Stratum Corneum the Skin Barrier, on Evolution of Atopic Dermatitis
Virendra N Sehgal*Received: 04-May-2018 Published: 09-Jan-2019
Abstract
The impact of evolving changing pattern in the character of stratum corneum, the sturdy skin barrier is highlighted, while taking stock of salient features of microanatomy and physiology. The role of cornified envelope, in particular, is vividly brought out as a vital pre-requisite to maintain and sustain the natural texture of stratum corneum. Thus the sequence of events leading to mobilization of filaggrin and valley of proteins to initiate and perpetuate the intricate mechanism in the natural history (evolution) of atopic dermatitis is focused attention to. Accordingly, up-to-date literature on the subject matter is reviewed in an endeavour to arrive at its contemporary prevalent status, and to encourage the on-going research.
Keywords
Atopic Dermatitis; Skin; Filaggrin
Introduction
Atopic Dermatitis (AD) is a pre-eminent age oriented entity with a continuous clinical spectrum ensuing in infancy, to March to childhood, adolescent, adult and senile/elderly [1] characterize by pruritus, with or without lichenification and xerosis. The entity has been in the reckoning ever since its inception, and is a matter of an intriguing dialogue, especially for its etio-pathogenesis, which has thus far been largely speculative. The emergence of stratum corneum, a formidable skin barrier, as a target tissue has added refreshing dimensions in the on-going research to find plausible explanation for the sequence of events in AD. A substantive work on its micro-anatomy [2,3] and related physiological components/changes (Figure 1) is startling [4].
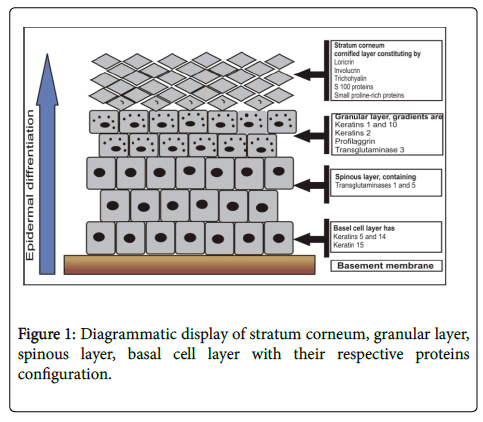
Figure 1. Diagrammatic display of stratum corneum, granular layer, spinous layer, basal cell layer with their respective proteins configuration.
Graphic is displaying the layers of epidermis and their proteins configuration. The accumulated data thus far seems conducive. In fact, the current status is directionally accrued to offer adequate work job for continuing research, and endeavour to provide an impetus is made, in the following text.
Microanatomy and Physiology of Stratum Corneum
Stratum corneum, the horny layer [1] (latin) is a fascinating, outermost layer of the epidermis [2,3] stratum lucidum, stratum granulosum, stratum spinosum and stratum basale are its other layers. Stratum corneum is formed by 15-20 layers of flattened dead cells with no nuclei (anucleated) and organelles; the corneocytes (Figure 2) their cytoplasm contains birefringent filamentous scleroprotein, the keratin.
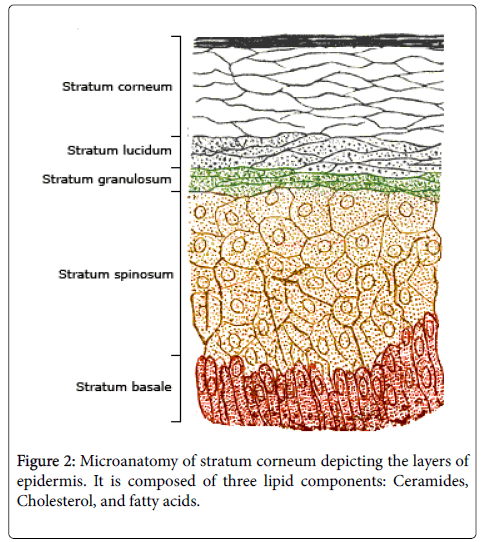
Figure 2. Microanatomy of stratum corneum depicting the layers of epidermis. It is composed of three lipid components: Ceramides, Cholesterol, and fatty acids.
It forms a formidable barrier to protect underlying tissue(s) from Infection; Dehydration; Chemicals and Mechanical stress.
Desquamation, the process of cell shedding, is a regular feature for balancing the proliferating keratinocytes that are formed in the stratum basale. These cells have the potential to migrate through the epidermis towards the surface, which may take about 14 days for the process to complete.
The advent of stratum corneum [5], an impeccable skin barrier, has emerged as a prime factor in the evolving pathogenesis of the atopic dermatitis. The skin barrier functions6 emanate from the sequence of events namely:-
• Transformation of living keratinocytes to non-living corneocytes.
• Cell membrane is replaced by a layer of ceramides covalently linked to structural proteins, the cornified envelope, surrounding the cells in the stratum corneum [6].
• Thus, facilitating cellular adhesion with adjacent cells in the epidermis by the modified desmosomes.
• The complexes thus formed are degraded by proteases, permitting cell to be shed. Hence, desquamation as well as cornified envelope are its essential pre-requisite [7,8]. Furthermore, up-regulation of serine protease activity may cause adverse structural changes in consequence to degradation of certain proteins, which are the part component of epidermal structure and its functions, thus interfering in the formation of the stratum corneum intercellular lipid membrane, regulating epidermal water flux and gradient, resulting in induction of TH2 (Subset Type pattern) of inflammation, the hallmark profile of atopic skin. Therefore mentioned formulation supplemented by alteration in lipid ratios and changes in lipid-directed enzymes may play a decisive role in the impairment of barrier functions, associated with atopic dermatitis.
• A dense network of keratin, a protein forming the cells of stratum corneum, helps keep the skin hydrated by preventing water evaporation and also by absorbing water. It possesses ‘spring back’ or stretchy properties, a weak glutenous protein bond pulls the skin back to its natural shape.
Filaggrin
Filaggrin [9], filament aggregating protein, is a unique filament-associated protein that binds to keratin fibers in epithelial cells. 10 to 12 filaggrin units are post-translationally hydrolized from a large pro-filaggrin precursor protein during terminal differentiation of epidermal cells. Thus, filaggrin is a key protein that facilitates terminal differentiation of the epidermis, and formation of the skin barrier. Besides, it’s specifically contributes to its physical strength, hydration status, skin pH, and buffering capacity among other physio-chemical properties. Impairment or loss of functions of filaggrin, the epidermal barrier protein is, therefore, a major pre-disposing factor in the pathogenesis of AD. In humans, pro-filaggrin is encoded by the FLG gene, which is part of the S100 fused-type protein (SFTP) family within the epidermal differentiation complex on chromosome 1q21 [10,11].
Filaggrin, is a key component of the stratum corneum that is derived from a larger precursor protein and contributes to its physical strength, hydration status, skin pH, and buffering capacity among other physio-chemical properties [12].
Glimpses into the structure and function of stratum corneum, the skin barrier is a salient overture for comprehending the upheaval in it functions in atopic dermatitis, in particular. It is, therefore, relevant to recall its clinical presentations namely; early age of onset, atopy, personal and/or family history, Immunoglobulin E reactivity and xerosis [13]. Moreover, AD seem to possess a clinical spectrum span from infantile, childhood, adolescent, adult and senile (elderly), xerosis being the common denominator with or without lichenification [1].
Currently, it is classified into Extrinsic atopic dermatitis (eAD ) [14] IgE associated allergic atopic dermatitis, and Intrinsic atopic dermatitis (iAD) non-allergic atopic eczema/dermatitis syndrome (AEDS) [15] The former have elevated Th2- and decreased Thl-expressing cells in the peripheral blood, with elevated interleukin, IL-4 and IL-13 expression. AD seems to be controlled by genetic factors [16]. The Immune System [17] and its dysfunction [18] is a subject of intriguing investigation, and is sequentially recounted; IgE Interactions between IgE-bearing antigen-presenting cells, T-cell activation, mast-cell degranulation, keratinocytes, eosinophils, and a combination of immediate and cellular immune responses are the hallmark of extrinsic atopic dermatitis (eAD) [19] Moreover, Inflammatory dendritic epidermal cells, a distinct dendritic cells population, could induce the Th2. It is, therefore, worthwhile to name genetic disorders which may have pre-disposition to hay fever, allergic rhinitis, bronchial asthma, including atopic dermatitis the atopic-diathesis. Pre-eminent amongst them are Agammaglobulinemia/X-linked hypogammaglobulinemia (XLA) [20] (X-linked recessive), Anhidrotic ectodermal dysplasia [21,22] (X-linked recessive), Cystic fibrosis(CF) [23-25] (Autosomal recessive), Hurler's syndrome [26] (Autosomal recessive), Hyper IgE syndrome (HIES) [27] (Autosomal dominant or autosomal recessive), Netherton's syndrome [28] (Autosomal recessive), Wiskott-Aldrich syndrome/thrombocytopenia [29], (X-linked recessive), and Down syndrome(DS,DNS) trisomy21 [30] (Autosomal dominant, Autosomal recessive).
Topical Therapy, Evolving Scenario’s Application in Day-to-Day Practice
Although, several treatment options are in vogue, its treatment continues to loom large, because its etiopathogenesis is largely seem to be enigmatic [31,32] nevertheless, the endeavors to unfold it are relentlessly continuing. The advent of stratum corneum [31-33] the impeccable skin barrier has taken the central stage. Accordingly, its micro-anatomy (structure) and physiology (function) has added refreshing dimensions. The alterations in its patho-physiology have been a definitive step forward, enshrining the role of flaggrin [34] and serine proteases [35] in particular. The changing pattern in the former may impede its physical strength, hydration status, skin pH, and buffering capacity amongst other physio-chemical properties. Filaggrin [36,37], the epidermal barrier protein is, therefore, a major pre-disposing factor in the pathogenesis of AD. In addition, up-regulation of serine protease activity may cause adverse structural changes due to degradation of certain proteins, the part component of epidermal structure and its functions, thus interfering in the formation of the stratum corneum intercellular lipid membrane, regulating epidermal water flux and gradient, resulting in induction of TH2 (Subset Type pattern) of inflammation. Simultaneous, immune system [38] and its dysfunction through IgE mediated sequence of events capped by genetic [39] undertones may initiate and/or perpetuate the clinical expression of AD. Hence, the preceding rumblings responsible for the clinical connotation of AD, may bring to the fore newer modalities to counter the intricate often difficult to treat condition. Thus, atopic dermatitis treatment envisages [40]
Eliminating inflammation and infection; Hydrating the skin; Controlling pruritus, and Avoiding exacerbative factors.
Addition of moisturizer to a low-potency corticosteroid lotion in separate regimens is effective in treating the signs and symptoms of mild-to-moderate atopic dermatitis [40,41].
REFERENCES
- Sehgal VN (2018) Atopic dermatitis (AD) age orientation revisited: A Position Paper; Cutis. (In press).
- Bouwstra JA, Honeywell-Nguyen PL, Gooris GS, Ponec M (2003) Structure of the skin barrier and its modulation by vesicular formulations. Prog Lipid Res 42: 1-36.
- Ovaere P, Lippens S, Vandenabeele P, Declercq W (2009) The emerging roles of serine protease cascades in the epidermis. Trends Biocheml Sci 34: 453-463.
- Sandilands A, Sutherland C, Irvine AD, McLean WH (2009) Filaggrin in the frontline: role in skin barrier function and disease. J Cell Sci 122: 1285-1294.
- Elias PM, Hatano Y, Williams ML (2008) Basis for the barrier abnormality in atopic dermatitis: outside-inside-outside pathogenic mechanisms. J Allergy Clin Immunol 121: 1337-1343.
- Bissett DL (2009) Common cosmeceuticals. Clin Dermatol 27: 435-445.
- Harding CR, Long S, Richardson J, Rogers J, Zhang Z, et al. (2003) The cornified cell envelope: an important marker of stratum corneum maturation in healthy and dry skin. Int J Cosmet Sci 25: 157-167.
- Kypriotou M, Huber M, Hohl D (2012) The human epidermal differentiation complex: cornified envelope precursors, S100 proteins and the ‘fused genes’ family. Exp Dermatol 21: 643-649.
- Levin J, Friedlander SF, Del Rosso JQ (2013) Atopic Dermatitis and the Stratum Corneum: Part 1: The Role of Filaggrin in the Stratum Corneum Barrier and Atopic Skin. J Clin Aesthet Dermatol 6: 16-22.
- Markova NG, Marekov LN, Chipev CC, Gan SQ, Idler WW, et al. (1993) Profilaggrin is a major epidermal calcium-binding protein. Mol Cell Biol 13: 613-625.
- Palmer CN, Irvine AD, Terron-Kwiatkowski A, Zhao Y, Liao H, et al. (2006) Common loss-of-function variants of the epidermal barrier protein filaggrin are a major predisposing factor for atopic dermatitis. Nat Genet 38: 441-446.
- Levin J, Friedlander SF, Del Rosso JQ (2013) Atopic Dermatitis and the Stratum Corneum: Part 2: Other Structural and Functional Characteristics of the Stratum Corneum Barrier in Atopic Skin. J Clin Aesthet Dermatol 6: 49–54.
- Eichenfield LF, Hanifin JM, Luger TA, Stevens SR, Pride HB (2003) Consensus conference on pediatric atopic dermatitis. J Am Acad Dermatol 49: 1088-1095.
- Wüthrich B, Schmid-Grendelmeier P (2003) The atopic eczema/dermatitis syndrome. Epidemiology, natural course, and immunology of the IgE-associated ("extrinsic") and the nonallergic ("intrinsic") AEDS. J Investig Allergol Clin Immunol 13: 1–5.
- Schmid-Grendelmeier P, Simon D, Simon HU, Simon HU, Akdis CA, et al. (2001) Epidemiology, clinical features, and immunology of the "intrinsic" (non-IgE-mediated) type of atopic dermatitis (constitutional dermatitis). Allergy 56: 841–849.
- Barnes KC (2010) An Update on the Genetics of Atopic Dermatitis: Scratching the Surface in 2009. J Allergy Clin Immunol 125: 16–31.
- Miraglia del Giudice M, Decimo F, Leonardi S, Maioello N, Amelio R, et al. (2006) Immune dysregulation in atopic dermatitis. Allergy Asthma Proc 27: 451-455.
- Levin J, Fallon Friedlander S, Del Rosso JQ (2013) Atopic Dermatitis and the Stratum Corneum: Part 3: The Immune System in Atopic Dermatitis. J Clin Aesthet Dermatol 6: 37–44.
- Karimkhani C, Silverberg JI, Dellavalle RP (2015) Defining intrinsic vs. extrinsic atopic dermatitis. Dermatol Online J 21.
- Lankisch P, Laws HJ, Weiss M, Borkhardt A (2014) Agammaglobulinemia and lack of immunization protection in exudative atopic dermatitis. Eur J Pediatr 173: 117-119.
- William J, Berger T, Elston D (2005) Andrews' Diseases of the Skin: Clinical Dermatology. 10th ed. Saunders.
- Koguchi-Yoshioka H, Wataya-Kaneda M, Yutani M, Murota H, Nakano H, et al. (2015) Atopic diathesis in hypohidrotic/anhidrotic ectodermal dysplasia. Acta Derm Venereol 95: 476-479.
- Nelson LA, Callerame ML, Schwartz RH (1979) Aspergillosis and Atopy in Cystic Fibrosis, Am Rev Respir Dis 120: 863-873.
- Quinton PM (2007) Cystic fibrosis: lessons from the sweat gland. Physiology (Bethesda) 22: 212–225.
- Lela B (2012) Mucopolysaccharidosis Type I at eMedicine, Molecular diagnostics fundamentals, methods, and clinical applications(2nd ed.). Philadelphia, F.A. Davis Co p, Unite States, pp: 351.
- Ohameje NU, Loveless JW, Saini SS (2006) Atopic dermatitis or hyper-IgE syndrome? Allergy Asthma Proc 27: 289-291.
- Hannula-Jouppi K, Laasanen SL, Heikkilä H, Tuomiranta M, Tuomi ML, et al. (2014) IgE allergen component-based profiling and atopic manifestations in patients with Netherton syndrome. J Allergy Clin Immunol 134: 985-988.
- Sullivan KE, Mullen CA, Blaese RM, Winkelstein JA (1994) A multi-institutional survey of the Wiskott-Aldrich syndrome. J Pediatr 125: 876-885.
- Schepis C, Barone C, Siragusa M, Romano C (1997) Prevalence of atopic dermatitis in patients with Down syndrome: a clinical survey. J Am Acad Dermatol 36: 1019-1021.
- Sehgal VN, Khurana A, Mendiratta V, Saxena D, Srivastava G, et al. (2016) K.Atopic Dermatitis: Clinical Connotations, Especially a Focus on Concomitant Atopic Undertones in Immunocompromised/Susceptible Genetic and Metabolic Disorders. Indian J Dermatol 61: 241-50.
- Sehgal VN, Khurana A, Mendiratta V, Saxena D, Srivastava G, et al. (2015) Atopic Dermatitis; Etio-Pathogenesis, An Overview. Indian J Dermatol 60: 327-31.
- Elias PM, Hatano Y, Williams ML (2008) Basis for the barrier abnormality in atopic dermatitis: outside-inside-outside pathogenic mechanisms. J Allergy Clin Immunol 121: 1337–1343.
- Levin J, Friedlander SF, James Q (2013) Atopic Dermatitis and the Stratum Corneum: Part 1: The Role of Filaggrin in the Stratum Corneum Barrier and Atopic Skin. J Clin Aesthet Dermatol 6: 16–22.
- Ovaere P, Lippens S, Vandenabeele P, Declercq W (2009) The emerging roles of serine protease cascades in the epidermis. Trends Biochem Sci 34: 453–463.
- Markova NG, Marekov LN, Chipev CC, Gan SQ, Idler WW, et al. (1993) Profilaggrin is a major epidermal calcium-binding protein. Mol Cell Biol 13: 613–625.
- Palmer CN, Irvine AD, Terron-Kwiatkowski A, Zhao Y, Liao H, et al. (2006) Common loss-of-function variants of the epidermal barrier protein filaggrin are a major predisposing factor for atopic dermatitis. Nat Genet 38: 441-446.
- Miraglia del Giudice M, Decimo F, Leonardi S, Maioello N, Amelio R, et al. (2006) Immune dys-regulation in atopic dermatitis. Allergy Asthma Proc 27: 451-455.
- Barnes KC (2010) An Update on the Genetics of Atopic Dermatitis: Scratching the Surface in 2009. J Allergy Clin Immunol 125: 16–31.
- Schnopp C, Holtmann C, Stock S, Remling R, Fölster-Holst R, et al. (2002) Topical Steroids under Wet-Wrap Dressings in Atopic Dermatitis A Vehicle-Controlled Trial. Dermatol 204: 56–59
- Hanifin JM, Hebert AA, Mays SR, Paller AS, Sherertz EF, et al. (1998) Effects of a low-potency corticosteroid lotion plus a moisturizing regimen in the treatment of atopic dermatitis. Cur Therap Res 59: 227–233.
Citation: Sehgal VN (2019) The Impact of Microanatomy and Changing Physiology of Stratum Corneum, the Skin Barrier, on Evolution of Atopic Dermatitis. J Dermatitis 4:116.
Copyright: © 2019 Sehgal VN, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

