Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Euro Pub
- Google Scholar
- Quality Open Access Market
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2023) Volume 9, Issue 1
Study of the Recommended Dosage of the N-Acetyl Cysteine, Alpha Lipoic Acid, Bromelain and Zinc Preparation for the Treatment of Dysmenorrhea
Zuramis Estrada1,2 and Francisco Carmona3,4*2Centro Internacional de Investigación, Médico estético, uro-Ginecológico (CIMEG) Madrid, Madrid, Spain
3Department of Gynecology, University of Barcelona, Institut Clinic of Gynecology, Obstetrics and Neonatology (ICGON), Hospital Clinic, Institute of Biomedical Research August P, Spain
4Faculty of Medicine, University of Barcelona, Barcelona, Spain
Received: 18-Jan-2023, Manuscript No. JPMME-23-19601; Editor assigned: 20-Jan-2023, Pre QC No. JPMME-23-19601 (PQ); Reviewed: 03-Feb-2023, QC No. JPMME-23-19601; Revised: 10-Feb-2023, Manuscript No. JPMME-23-19601 (R); Published: 20-Feb-2023
Abstract
Background: Dysmenorrhea is defined as pain during menstruation and affects a large percentage of women with varying degrees of pain. Currently, gynecologists recommend a preparation composed of N-Acetyl Cysteine (NAC), alpha Lipoic Acid (LA), Bromelain (Br) and Zinc (Zn), (NAC/LA/Br/Zn) to relieve the symptoms of dysmenorrhea. However, there are no data on the most adequate dosage to recommend in patients with dysmenorrhea. Therefore, the aim of this study was to determine when the NAC/LA/Br/Zn preparation is recommended in patients with dysmenorrhea and on what basis specialists make this decision.
Methods: A survey was conducted among gynecologists with extensive experience recommending this preparation. Descriptive statistics including absolute numbers, frequencies (%) and means were used to explore the data.
Results: The most frequently recommended regimen is to begin with continuous administration for 90 days with 10-day breaks (69%). In patients with primary dysmenorrhea the most recommended approach is discontinuous therapy for mild pain (50.7%) and 90-day continuous therapy with 10-day breaks in patients with moderate or severe pain (47.9% and 71.2%, respectively). In the case of secondary dysmenorrhea, the most recommended approach is 90-day continuous therapy with 10-day breaks for any degree of pain (41.1%, 57.5% and 76.7% respectively). Most gynecologists (79%) adapt the regimen after clinical assessment of the degree of pain towards discontinuous administration patterns on the days around menstruation.
Conclusions: The most common regimen for the treatment of dysmenorrhea with the NAC/LA/Br/Zn preparation is to start treatment with 90 days of administration with 10-day breaks. The treatment can subsequently be continued with the same continuous regimen with breaks or adapted according to the degree of pain.
Keywords
Dysmenorrhea; N-Acetyl Cysteine; Alpha Lipoic Acid; Bromelain; Zinc; Antioxidants
INTRODUCTION
Dysmenorrhea is defined as pain during menstruation and is the most common gynecological condition, affecting a large percentage of women with varying degrees of pain [1-4]. Although there is no consensus on the prevalence of dysmenorrhea in the literature, between 17% and 81% of women present this condition, with 12% to 14% reporting severe dysmenorrhea [5]. Dysmenorrhea is classified as primary, when the underlying anomaly is unknown, or secondary, which is usually strongly associated with endometriosis or pelvic inflammatory disease, among other causes [4,6-10]. In recent years, the management of dysmenorrhea has become increasingly important because of the emotional, health and economic burden it entails and because of the need for new studies and research for effective treatments to alleviate the symptoms [11-15].
Treatments for dysmenorrhea can be classified as pharmacological, such as Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) and combined hormonal contraceptives, or non-pharmacological, including complementary treatments to reduce pain [16-19]. Currently, gynecologists recommend the preparation of N-Acetyl Cysteine (NAC), Alpha Lipoic Acid (LA), Bromelain (Br) and zinc (Zn) (NAC/LA/Br/Zn) due to its antioxidant, anti-inflammatory and analgesic properties [20-24].
However, there is a lack of evidence on how the NAC/LA/Br/Zn preparation is used in daily clinical practice, and thus, we decided to conduct a survey to gather information on the experience of gynecologists who recommend this preparation for the treatment of dysmenorrhea. Therefore, the aim of the study was to determine the doses of the preparation most frequently recommended for both Primary Dysmenorrhea (PD) and Secondary Dysmenorrhea (SD) and other causes of pain for which NAC/LA/Br/Zn is recommended as well as the characteristics of the patients and the adaptation of the treatment according to patient response [25,26].
Material and Methods
Survey approach
A total of 75 gynecologists from different geographical areas of Spain with extensive professional experience in the treatment of dysmenorrhea participated in the study. The survey was sent to gynecologists with experience treating patients with the NAC/ LA/Br/Zn preparation. The identities of all participants remained confidential during data collection and analysis. Participation by the specialists was voluntary, free and unconditional.
The data on treatment times and the concentration of the preparation components were described previously by Lete, et al., in patients with endometriosis and were used as a reference for developing the survey [27]. The specialists were invited to participate by responding to a structured survey aimed at reporting the recommended dosage of the NAC/LA/Br/Zn preparation for patients with menstrual pain. The survey was structured in five sections: 1) previous considerations (reason for use of the preparation and patient characteristics); 2) PD (patient management and dosage); 3) SD and other causes of pain (patient management and dosage); 4) association of the NAC/LA/Br/Zn preparation with other drugs; 5) final considerations and comments by the specialists consulted. The survey consisted of 37 questions, 32 of which were single-answer questions, and 5 were multiple-choice questions. Open text fields were available for the questions to enter responses not included in the list, with the exception of five questions for which the proposed options were categorical. The full survey can be found in the Supplementary Material.
Data analysis and statistics
The gynecologists' responses were collected using the Google Forms tool (Google LLC), and downloaded into a Microsoft Excel 2019 file (Microsoft Office, Redmond, WA) for analysis. Open-ended questions were manually coded into general response categories by a single author using inductive coding with iterative sampling and recoding. In the multiple-choice questions, the number of times each answer was selected was analyzed. None of the participants' responses were excluded from the analysis. Descriptive statistics including absolute numbers, frequencies (%) and means were used to explore the data.
Results
The level of participation was high, with 73 of the 75 specialists (97.3%) invited to participate having completed all the sections of the survey. The gynecologists consulted recommended the NAC/ LA/Br/Zn preparation to patients with any type of menstrual pain, especially in women wishing to reduce the consumption of NSAIDs (48 responses), in those wishing to become pregnant (46 responses), and patients with pain who did not want to take contraceptives (32 responses) (possibility of multiple responses) (Figure 1A). The majority of the gynecologists recommended the NAC/LA/Br/Zn preparation to patients reporting any degree of pain (49%), followed by patients with moderate pain (with a score between 4 and 7 on the Visual Analogue Scale (VAS), 37%) or those with severe pain (>7 VAS, 14%) (Figure 1B).
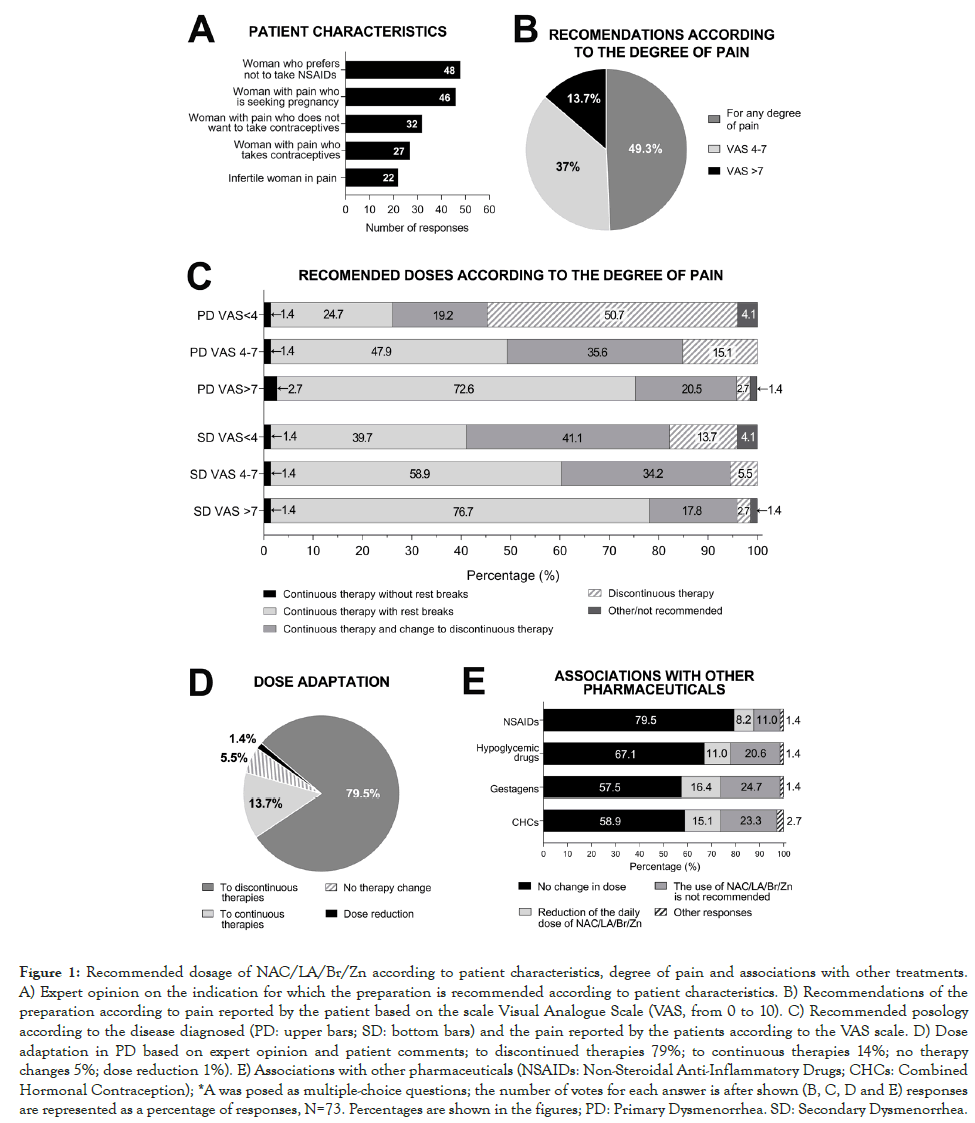
Figure 1: Recommended dosage of NAC/LA/Br/Zn according to patient characteristics, degree of pain and associations with other treatments. A) Expert opinion on the indication for which the preparation is recommended according to patient characteristics. B) Recommendations of the preparation according to pain reported by the patient based on the scale Visual Analogue Scale (VAS, from 0 to 10). C) Recommended posology according to the disease diagnosed (PD: upper bars; SD: bottom bars) and the pain reported by the patients according to the VAS scale. D) Dose adaptation in PD based on expert opinion and patient comments; to discontinued therapies 79%; to continuous therapies 14%; no therapy changes 5%; dose reduction 1%). E) Associations with other pharmaceuticals (NSAIDs: Non-Steroidal Anti-Inflammatory Drugs; CHCs: Combined Hormonal Contraception); *A was posed as multiple-choice questions; the number of votes for each answer is after shown (B, C, D and E) responses are represented as a percentage of responses, N=73. Percentages are shown in the figures; PD: Primary Dysmenorrhea. SD: Secondary Dysmenorrhea.
Recommended dosages
At the beginning of treatment with the preparation, gynecologists recommend the administration of NAC 600 mg/day, LA 200 mg/ day, Br 25 mg/day and Zn 10 mg/day (71.2% for PD, 80.8% for SD), while the remaining gynecologists recommend starting treatment with half the concentration, which may be doubled in the case of no response to treatment (27.8% for PD and 19.2% for SD) (Supplementary Figure).
The regimens recommended by specialists at the beginning of treatment may be continuous or discontinuous. The continuous regimen most commonly recommended by 69% of the specialists is continuous therapy with breaks (10 days of rest per 90-day treatment cycle) followed by continuous therapy without breaks (31% of the specialists) (Table 1). Discontinuous regimens entail administration of the preparation 7-15 days before menstruation (54%), 5 days before and 5 days after menstruation (24%), only 5 days before menstruation (15%) or other variations (7%) (Table 1).
| Administration | Posology | Type of dysmenorrhea | ||
|---|---|---|---|---|
| PD | SD | |||
| Continuous | 90 days with 10-day breaks | 69% | 52,00% | 65.70% |
| 90 days without 10-day breaks | 31% | 23.30% | 32.90% | |
|
100% | |||
| Discontinuous | 7-15 days before menstruation | 54% | 24.70% | 1.40% |
| 5 days after & 5 days before menstruation | 24% | |||
| 5 days after menstruation | 15% | |||
| other variations | 7% | |||
|
100% | 100% | 100% | |
Note: N=73. |
||||
Table 1: Recommended dosages of the NAC/LA/Br/Zn preparation on initiation of dysmenorrhea treatment.
For the treatment of dysmenorrhea, the most commonly recommended therapy at the start of treatment is continuous administration with 10-day breaks every 90 days of treatment (52.0% for PD and 65.7% for SD). In the case of PD, 23.3% of specialists recommend long-duration therapies (>90 days) and 11% short-duration (<90 days). In the case of SD, 24.7% also recommend continuous administration without breaks at the start of treatment while 1.4% recommend short-duration therapies (<90 days) (Table 1).
The decision to recommend the regimen is based on the pain reported by patients. For PD patients with mild pain, most specialists recommend discontinuous therapies (50.7%), followed by continuous therapy with breaks (24.7%) and administration for 90 days followed by a change to discontinuous therapy (19.2%). For patients with moderate or severe pain, the most recommended option is continuous therapy with breaks (47.9% and 72.6%, respectively), followed by administration for 90 days with change to discontinuous (35.6% and 20.5%, respectively) (Figure 1C and Table 2).
| Dysmenorrhea | Grade of pain (visual analogue scale) | Posology | ||||
|---|---|---|---|---|---|---|
| Continuous therapy without rest breaks | Continuous therapy with rest breaks | 90 days of administration and switch to discontinuous therapy | Discontinuous therapy | Other/not recommended | ||
| Primary | VAS<4 | 1.40% | 24.70% | 19.20% | 50.70% | 4.10% |
| VAS 4-7 | 1.40% | 47.90% | 35.60% | 15.10% | 0.00% | |
| VAS>7 | 2.70% | 72.60% | 20.50% | 2.70% | 1.40% | |
| Secondary | VAS<4 | 1.40% | 39.70% | 41.10% | 13.70% | 4.10% |
| VAS 4-7 | 1.40% | 58.90% | 34.20% | 5.50% | 0.00% | |
| VAS>7 | 1.40% | 76.70% | 17.80% | 2.70% | 1.40% | |
Note: 1) Continuous therapy without breaks; 2) Continuous therapy with breaks (10 days off per 90-day treatment cycle); 3) 90 days of administration and switch to discontinuous therapy; 4) Discontinuous therapy (5 days before menstruation and 5 days after or 7-15 days before menstruation), N=73. |
||||||
Table 2: Recommended posology according to the disease diagnosed and the pain reported by the patients according to the VAS scale.
In contrast to PD, in SD patients with mild pain, most specialists recommended 90 days with a change to discontinuous therapy (41,1%), followed by continuous therapy with breaks (39.7%) and discontinuous therapy (13.7%) (Figure 1C and Table 2). For patients with moderate or severe pain, the most recommended option is continuous therapy with breaks (58.9% and 76.7%, respectively), followed by administration for 90 days with a change to discontinuous (34.2% and 17.8%, respectively) (Figure 1C and Table 2).
In relation to other causes of pain, 63% of gynecologists recommend the preparation, while 33% only recommend it for endometriosis or dysmenorrhea associated with endometriosis, and the remaining 4% recommend it when all other treatments fail. Among those recommending the preparation, the most commonly recommended dosage is continuous therapy with 10-day breaks (47.4%), followed by administration for 90 days with a change to discontinuous therapy (31.6%), and 17.6% recommend discontinuous therapies (7-15 days before menstruation or 5 days before and 5 days after, both recommended with the same frequency).
Regarding dose adaptation, 79.5% of gynecologists recommend switching from continuous to discontinuous administration, while other gynecologists recommend switching from discontinuous to continuous administration (13.7%), without adapting the regimen (5.5%) or choosing other options (1.4%) (Figure 1D). Among specialists who recommend switching to discontinued therapies, the most recommended regimens are administration 7-15 days before menstruation (44%), 5 days before (19%) or 5 days before and after menstruation (16%). Specialists recommend an indefinite duration of treatment (57.7%) or for more than 90 days (47.9%), and patient evaluation every 90 days (56.2%), or more frequently (35.6%).
Association of the preparation with other pharmaceuticals
Some patients who are recommended the NAC/LA/Br/Zn preparation are also being treated with other pharmaceuticals. While some gynecologists recommend the preparation without modification of the dosage when patients are receiving NSAIDs, gestagens or a combination of hormonal contraception (79.5%, 57.5% and 58.9%, respectively), others modify the dosage of the preparation (8.2%, 16.4% and 15.1%, respectively). Some specialists do not recommend the preparation when patients are being treated with NSAIDs, gestagens, combination of hormonal contraceptives (11%, 24.7% and 23.3% respectively). In cases in which patients are being treated with hypoglycemic drugs, 67.1% of gynecologists recommend the NAC/LA/Br/Zn preparation without modifying the regimen, compared to 20.6% who do not recommend the preparation in these cases and 11% who reduce the daily dose (Figure 1E).
Combined use with hygienic-sanitary measures
In addition to treatment, most patients are recommended a series of hygienic-dietary measures, based on healthy eating, exercise and avoiding stress. Ninety percent of gynecologists recommend the NAC/LA/Br/Zn preparation along with all hygienic-dietary measures, 6% recommend the preparation alone and 4% recommend the preparation with a healthy diet. Ninety percent of specialists do not modify the dose of the preparation when recommending hygienic-dietary guidelines.
Patient satisfaction and reported adverse effects
Depending on the progression of pain reported by the patients, 92% of specialists adapt the dose of the preparation compared to 8% who do not. For gynecologists who adapt the dose, the most frequent change is from continuous to discontinuous treatment (60%) compared to those who report changes from discontinuous to continuous regimens (26%). Finally, the study participants stated that the NAC/LA/Br/Zn preparation is well tolerated by patients, with gastrointestinal discomfort being the only adverse effect detected by 11% of the gynecologists consulted (Supplementary Figure 1D).
Discussion
This is the first study to describe the dosages of the NAC/LA/ Br/Zn preparation most recommended by gynecological experts in patients with dysmenorrhea. The most frequently recommended regimen is to begin with continuous administration for 90 days with 10-day breaks. In subsequent evaluations, specialists may maintain this dosage or change it if the patient reports a reduction in pain. In addition, this study sheds light on how gynecologists recommend the NAC/LA/Br/Zn preparation according to patient characteristics, the degree of pain, the type of dysmenorrhea and the association with other pharmaceuticals.
Given the lack of data in the literature on the guidelines for recommending the NAC/LA/Br/Zn preparation in clinical practice, further studies are needed to determine the most adequate dosages and the patients to whom it should be administered. It is important to know the opinion of gynecologists who have experience recommending the preparation to patients with dysmenorrhea to establish the most adequate indications used for administration. The methodology chosen to obtain this information was a survey of gynecologists in Spain, which is a validated approach that has been used in other clinical settings [28-31].
At the beginning of the treatment for dysmenorrhea, the most frequently recommended regimen is continuous administration of the NAC/LA/Br/Zn preparation for 90 days with 10-day breaks, although one third of those consulted recommend continuous administration without breaks. In subsequent evaluations, the specialist may recommend continuing with this regimen or may change to a discontinuous dose if the pain has subsided. In patients initially reporting mild pain, the specialist may recommend starting therapy with discontinuous administration of the preparation. The most frequently recommended discontinuous regimens involve administering the preparation 7-15 days before menstruation or 5 days before and 5 days after. Administration of the preparation around the days of menstruation results in a reduction in menstrual pain. Some specialists stated that the regimen can be switched to a continuous dose in patients reporting an increase in pain following a discontinuous dose.
In patients with PD, gynecologists recommend and adapt the dose of the preparation according to the pain described by the patient. When the pain is moderate or severe, gynecologists usually opt for continuous treatment, while discontinuous treatment is more frequently recommended for mild pain. Upon reevaluation, the tendency is to reduce the number of doses of the preparation because it continues to be effective in reducing pain, although in some cases it can be changed from a discontinuous to a continuous regimen if the patient reports increased pain with a discontinuous regimen. However, in women with SD, continuous therapy followed by re-evaluation is the most recommended treatment for patients with any degree of pain. This may be due to the fact that patients with SD have previously been diagnosed with endometriosis, which is the probable cause of the pain, and therefore, gynecologists most often recommend long-acting regimens to reduce pain following the dose reported in the study by Lete, et al., [27]. This study also reported that the preparation is recommended for patients with other causes of pelvic pain, since it was also found to be effective in reducing pain in these patients. The therapy most commonly recommended for other causes of pelvic pain, as well as for PD and SD, is the administration of the preparation for 90 days with 10-day breaks.
This preparation has shown to be effective in patients diagnosed with pelvic pain associated with endometriosis with the use of NAC 600 mg/day, LA 200 mg/day, Br 25 mg/day and Zn 10 mg/day for 6 months [27]. In this prospective, open-label clinical study of Lete, et al., patients taking the preparation reported a reduction in pain from 6.7 to 3.5 on the VAS scale and a reduction in the intake of NSAIDs, whether administered regularly or on menstrual days. The evidence available to date indicates that separately the individual compounds are beneficial for patients with endometriosis-associated menstrual pain, but at different doses or treatment times than those recommended in daily clinical practice. Treatment with NAC significantly reduced pain caused by dysmenorrhea and vaginal bleeding when administered for 90 days at the same concentration as in this study [32,33]. A reduction of painful symptoms associated with endometriosis has also been described with lower doses of NAC (150 mg/day), short treatments (60 days) and in combination with other molecules [34]. The use of LA as a treatment for dysmenorrhea and chronic pelvic pain associated with endometriosis reported greater efficacy in reducing pain when administered in combination with other compounds [35]. Continuous treatment and treatment on the days before menstruation have shown positive results in reducing pain [35,36]. One case report described that the administration of Br (2000 mg/ day changing to 3000 mg/day 3 days before menses) in combination with other compounds and acupuncture significantly reduced pain (from 8 to 2 on the VAS scale) [37]. Other studies administering bromelain extract (1.5 mg/mL in phosphate-buffered saline, 5 minutes vaginal irrigation) showed immediate relief in 62% of patients [38,39]. Zn supplementation has been reported to prevent uterine spasms and cramps, inducing a reduction in prostaglandin synthesis by reducing cyclooxygenase-2 activity and an improvement in endometrial tissue microcirculation [40-42]. The administration of Zn at concentrations between 20 and 126 mg/day for 3-6 days before and after menstruation reduced pain in the first menstrual cycle after the first intake, although the reduction in pain was greater in subsequent cycles [43-45]. Regarding doses, concentrations higher than 30 mg/day did not show a better additional effect, probably due to the poor absorption of Zn in the intestine [42,46].
Numerous therapeutic strategies and drugs approved by regulatory agencies are currently available to treat endometriosis and associated symptoms such as dysmenorrhea. In most cases, specialists recommend the preparation in conjunction with the prescribed treatment (between 60% and 80%) as opposed to those who do not (between 10% and 25%). Gynecologists more frequently recommend the preparation when it is associated with NSAIDs, probably because of the anti-inflammatory properties of the preparation and because it can complement or reduce the administration of NSAIDs [27]. The preparation is less frequently recommended when the patient is being treated with hormonal contraception or with a combination of progestogens. This may be because oral contraceptive treatments are able to inhibit ovulation and endometrial proliferation, reducing or eliminating menstrual pain, resulting in specialists less frequently recommending the combination in these cases.
Clinical guidelines for the management of patients with menstrual pain also include some non-pharmacological strategies or recommendations, such as exercise, healthy diet and natural remedies. Although there is no solid scientific evidence in this regard, the components of the preparation have antioxidant, anti-inflammatory and analgesic properties [35,41,47]. Therefore, specialists recommend the preparation for its effectiveness in reducing pain as a complement to promoting healthy habits.
The NAC/LA/Br/Zn preparation is well tolerated by patients, with adverse reactions reported in only 11% of patients. The adverse reactions reported include mild gastrointestinal discomfort, such as epigastralgia, gastralgia, abdominal bloating, gastric intolerance or heartburn. In relation to the components of the preparation, gastric problems such as nausea, vomiting, diarrhea, pain and heartburn have been reported as adverse effects, albeit infrequent (1:1000), of NAC [48].
Conclusion
The most common regimen for the treatment of dysmenorrhea with the NAC/LA/Br/Zn preparation (600 mg/day, 200 mg/ day, 25 mg/day and 10 mg/day) is to start treatment with 90 days of administration with 10-day breaks. In subsequent evaluations with the specialist, the treatment can be continued with the same continuous regimen with breaks or adapted according to the degree of pain. In the case of adapting the therapy to a discontinuous dosage, the regimen most frequently recommended by specialists is the administration of the preparation 7-15 days before menstruation.
The study obtained a wide participation of gynecologists who are experienced in treating dysmenorrhea and who recommend the NAC/LA/Br/Zn preparation in daily clinical practice. The gynecologists responded freely without any prior consideration, including all their answers in the analysis. We obtained a great deal of information on how the preparation is recommended in patients with any degree of pain at the beginning of treatment and after re-evaluations, as well as the association with other treatments or therapies. In addition, details were obtained on how patients with dysmenorrhea are evaluated, segmented and followed so that they receive the most appropriate dosage. The results obtained justify and support further studies on the effectiveness of the preparation in patients with dysmenorrhea.
Limitations
This study did not include the testimony of patients, or clinical data related to patients with dysmenorrhea treated with the preparation. According to the main objective of the study, the survey was especially aimed at gynecologists who had experience recommending the preparation.
Supplementary Material
Supplementary figure and study's survey
Sources of Funding
The study was funded by a grant from Adamed Spain S.L.U, who was not involved in the design of the study, data collection or interpretation.
Acknowledgments
The authors would like to thank the colleagues that responded to the survey: I. Adiego Calvo; M. Al Adib Mendiri; R. Alania López; A. Alonso García; C. Alonso García; J. Armengol Santacreu; A. Bahillo Varela; R. Baltà i Arandes; R. M. Barceló Tortella; A. I. Barqueros Ramírez; R. Barrientos Naz; A. Biterna Tejeiro; I. Bonal Cea; P. Burguete Fenollosa; E. S. Cabo Silva; R. Campos Caballero; A. Cañadas Molina; A. Carazo Piñeiro; A. Carballo García; M. J. Carballo Martínez; M. Carrascoso Altares; T. Casanova Sanchis; A. Cearsolo Michelena; C. Chacón Aguilar; A. Chassignet Martin; M. C. Chicharro Cassuso; R. Curiel Rodado; J. Dapena González; Miriam de la Flor López; Lucia Diaz Meca; V. Domínguez Rubio; M. J. Fernández Ramírez; E. Fresnadillo Humet; R. Galvan García; O. Gómez Pardo; N. Fernández Aller; M. González Jareño; E. González Rodríguez; C. Grau Bravo; E. Grau Civit; F. Hamadache Chabouni; R. Herrera Recio; A. Jodar Santibáñez; M. Juárez Cuervo; I. Juárez Pallarés; S. Landeo Agüero; M. Lapresta Moros; E. López Pérez; J. López Pérez; D. Lubian López; C. Marcos Santos; C. Miyares Erausquin; F. Moreno Aguayo; M. J. Moreno Pérez; T. Muñoz Fernández; I. Navarro Alonso; M. C. Paladino Decile; M. I. Parra Ribes; M. D. Pérez-Jaraíz López-Zaballa; A. Prades Sanchis; C. Puertas; M. A. Quiñones Chávez; B. Ramos Balbona; R. Reboredo García; E. Recari Elizalde; F. Rubio Fernández; E. Ruipérez Pacheco; J. Sánchez Orta; C. Caninzzo Naccarato; J.F. Subiris González; C. Troncoso Miranda.
Authors Contribution Statement
Zuramis Estrada and Francisco Carmona have contributed equally to the conceptualization, formal analysis and writing of the original draft.
References
- Dawood MY. Primary dysmenorrhea: Advances in pathogenesis and management. Obstet Gynecol. 2006;108(2):428-441.
[Crossref] [Google Scholar] [Pub Med]
- Chan WY, Fuchs F, Powell AM. Effects of naproxen sodium on menstrual prostaglandins and primary dysmenorrhea. Obstet Gyneco. 1983;61(3):285-291.
- Ferries-Rowe E, Corey E, Archer JS. Primary dysmenorrhea: Diagnosis and therapy. Obstet Gyneco. 2020;136(5):1047-1058.
[Crossref] [Google Scholar] [Pub Med]
- Ylikorkala O, Dawood MY. New concepts in dysmenorrhea. Am J Obstet Gynecol. 1978;130(7):833-847.
[Crossref] [Google Scholar] [Pub Med]
- Latthe P, Latthe M, Say L, Gülmezoglu M, Khan KS. WHO systematic review of prevalence of chronic pelvic pain: A neglected reproductive health morbidity. BMC Public Health. 2006;6(1):1-7.
[Crossref] [Google Scholar] [Pub Med]
- French L. Dysmenorrhea in adolescents. Paediatr Drugs. 2008;10(1):1-7.
[Crossref] [Google Scholar] [Pub Med]
- Giudice LC, Kao LC. Endometriosis Lancet. 2004;364(9447):1789-1799.
[Crossref] [Google Scholar] [Pub Med]
- Sanfilippo J, Erb T. Evaluation and management of dysmenorrhea in adolescents. Clin Obstet Gynecol. 2008;51(2):257-267.
[Crossref] [Google Scholar] [Pub Med]
- Stuparich MA, Donnellan NM, Sanfilippo JS. Endometriosis in the adolescent patient. Semin Reprod Med. 2017;35(1):102-109.
[Crossref] [Google Scholar] [Pub Med]
- Harel Z. Dysmenorrhea in adolescents and young adults: An update on pharmacological treatments and management strategies. Expert Opin Pharmacother. 2012;13(15):2157-2170.
[Crossref] [Google Scholar] [Pub Med]
- Weissman AM, Hartz AJ, Hansen MD, Johnson SR. The natural history of primary dysmenorrhoea: A longitudinal study. BJOG. 2004;111(4):345-352.
[Crossref] [Google Scholar] [Pub Med]
- Burnett MA, Antao V, Black A, Feldman K, Grenville A, Lea R, et al. Prevalence of primary dysmenorrhea in Canada. J Obstet Gynaecol Can. 2005;27(8):765-770.
[Crossref] [Google Scholar] [Pub Med]
- Harlow SD, Park M. A longitudinal study of risk factors for the occurrence, duration and severity of menstrual cramps in a cohort of college women. Br J Obstet Gynaecol. 1996;103(11):1134-1142.
[Crossref] [Google Scholar] [Pub Med]
- Pawłowski B. Prevalence of menstrual pain in relation to the reproductive life history of women from the Mayan rural community. Ann Hum Biol. 2004;31(1):1-8.
[Crossref] [Google Scholar] [Pub Med]
- Osayande AS, Mehulic S. Diagnosis and initial management of dysmenorrhea. Am Fam Physician. 2014;89(5):341-346.
- Patel V, Tanksale V, Sahasrabhojanee M, Gupte S, Nevrekar P. The burden and determinants of dysmenorrhoea: A population‐based survey of 2262 women in Goa, India. BJOG: An International Journal of Obstetrics & Gynaecology. 2006;113(4):453-463.
[Crossref] [Google Scholar] [Pub Med]
- Dawood MY. Ibuprofen and dysmenorrhea. Am J Med. 1984;77(1):87-94.
[Crossref] [Google Scholar] [Pub Med]
- Marjoribanks J, Proctor M, Farquhar C, Sangkomkamhang US, Derks RS. Nonsteroidal anti-inflammatory drugs for primary dysmenorrhoea. Cochrane Database Syst Rev. 2003(4):CD001751.
[Crossref] [Google Scholar] [Pub Med]
- Zhang WY, Li Wan Po A. Efficacy of minor analgesics in primary dysmenorrhoea: A systematic review. Br J Obstet Gynaecol. 1998;105(7):780-789.
[Crossref] [Google Scholar] [Pub Med]
- Milsom I, Andersch B. Effect of various oral contraceptive combinations on dysmenorrhea. Gynecol Obstet Invest. 1984;17(6):284-292.
[Crossref] [Google Scholar] [Pub Med]
- Milsom I, Sundell G, Andersch B. The influence of different combined oral contraceptives on the prevalence and severity of dysmenorrhea. Contraception. 1990;42(5):497-506.
[Crossref] [Google Scholar] [Pub Med]
- Armstrong C. ACOG Practice Bulletin No. 110: Noncontraceptive uses of hormonal contraceptives. Obstet Gynecol 2010;110(1):206–218.
[Crossref] [Google Scholar] [Pub Med]
- Barnard ND, Scialli AR, Hurlock D, Bertron P. Diet and sex-hormone binding globulin, dysmenorrhea, and premenstrual symptoms. Obstet Gynecol. 2000;95(2):245-250.
[Crossref] [Google Scholar] [Pub Med]
- Proctor M, Farquhar C, Stones W, He L, Zhu X, Brown J. Transcutaneous electrical nerve stimulation for primary dysmenorrhoea. Cochrane Database Syst Rev. 2002(1):CD002123.
[Crossref] [Google Scholar] [Pub Med]
- Mayer JM, Mooney V, Matheson LN, Erasala GN, Verna JL, Udermann BE, et al. Continuous low-level heat wrap therapy for the prevention and early phase treatment of delayed-onset muscle soreness of the low back: A randomized controlled trial. Arch Phys Med Rehabil. 2006;87(10):1310-1307.
[Crossref] [Google Scholar] [Pub Med]
- Pattanittum P, Kunyanone N, Brown J, Sangkomkamhang US, Barnes J, Seyfoddin V, et al. Dietary supplements for dysmenorrhoea. Cochrane Database Syst Rev. 2016;2016(3).
- Lete I, Mendoza N, de la Viuda E, Carmona F. Effectiveness of an antioxidant preparation with N-acetyl cysteine, alpha lipoic acid and bromelain in the treatment of endometriosis-associated pelvic pain: LEAP study. Eur J Obstet Gynecol Reprod Biol. 2018;228:221-224.
[Crossref] [Google Scholar] [Pub Med]
- Agostinis C, Zorzet S, De Leo R, Zauli G, De Seta F, Bulla R. The combination of N-acetyl cysteine, alpha-lipoic acid, and bromelain shows high anti-inflammatory properties in novel in vivo and in vitro models of endometriosis. Mediators Inflamm. 2015;2015:918089.
[Crossref] [Google Scholar] [Pub Med]
- Tamma PD, Aucott SW, Milstone AM. Chlorhexidine use in the neonatal intensive care unit: Results from a national survey. Infect Control Hosp Epidemiol. 2010;31(8):846-849.
[Crossref] [Google Scholar] [Pub Med]
- Corsini I, Ficial B, Fiocchi S, Schena F, Capolupo I, Cerbo RM, et al. Neonatologist performed echocardiography (NPE) in Italian neonatal intensive care units: A national survey. Ital J Pediatr. 2019;45:1-7.
[Crossref] [Google Scholar] [Pub Med]
- Lazcano-Gomez G, Alvarez-Ascencio D, Haro-Zuno C, Turati-Acosta M, Garcia-Huerta M, Jimenez-Arroyo J, et al. Glaucoma medication preferences among glaucoma specialists in Mexico. J Curr Glaucoma Pract. 2017;11(3):97-100.
[Crossref] [Google Scholar] [Pub Med]
- Porpora MG, Brunelli R, Costa G, Imperiale L, Krasnowska EK, Lundeberg T, et al. A promise in the treatment of endometriosis: An observational cohort study on ovarian endometrioma reduction by N-acetylcysteine. Evid Based Complement Alternat Med. 2013;2013:240702.
[Crossref] [Google Scholar] [Pub Med]
- Aghaamoo S, Zandbina A, Saffarieh E, Nassiri S. The effect of N‐acetyl cysteine on the volume of uterine leiomyoma: A randomized clinical trial. Int J Gynaecol Obstet. 2021;154(3):521-525.
[Crossref] [Google Scholar] [Pub Med]
- Fadin M, Nicoletti MC, Pellizzato M, Accardi M, Baietti MG, Fratter A. Effectiveness of the integration of quercetin, turmeric, and N-acetylcysteine in reducing inflammation and pain associated with endometriosis. In-vitro and in-vivo studies. Minerva Ginecol. 2020;72(5):285-291.
[Crossref] [Google Scholar] [Pub Med]
- de Leo V, Cagnacci A, Cappelli V, Biasioli A, Leonardi D, Seracchioli R. Role of a natural integrator based on lipoic acid, palmitoiletanolamide and myrrh in the treatment of chronic pelvic pain and endometriosis. Minerva Ginecol. 2019;71(3):191-195.
[Crossref] [Google Scholar] [Pub Med]
- Yousefi M, Kavianpour M, Hesami S, Nooshabadi MR, Haghighian HK. Effect of alpha-lipoic acid at the combination with mefenamic acid in girls with primary dysmenorrhea: Randomized, double-blind, placebo-controlled clinical trial. Gynecol Endocrinol. 2019; 35(9):782-786.
[Crossref] [Google Scholar] [Pub Med]
- Martin BR. Multimodal care for headaches, lumbopelvic pain, and dysmenorrhea in a woman with endometriosis: A case report. J Chiropr Med. 2021;20(3):148-157.
[Crossref] [Google Scholar] [Pub Med]
- Hunter RG, Henry GW, Heinicke RM. The action of papain and bromelain on the uterus. Am J Obstet Gynecol. 1957;73(4):867-874.
[Crossref] [Google Scholar] [Pub Med]
- Simmons C. The relief of pain in spasmodic dysmenorrhoea by bromelain. Lancet. 1958;272(7051):827-830.
[Crossref] [Google Scholar] [Pub Med]
- Kelly RW, Abel MH. Copper and zinc inhibit the metabolism of prostaglandin by the human uterus. Biol Reprod. 1983;28(4):883-889.
[Crossref] [Google Scholar] [Pub Med]
- Prasad AS. Clinical, immunological, anti-inflammatory and antioxidant roles of zinc. Exp Gerontol. 2008;43(5):370-377.
[Crossref] [Google Scholar] [Pub Med]
- Eby GA. Zinc treatment prevents dysmenorrhea. Med Hypotheses. 2007;69(2):297-301.
[Crossref] [Google Scholar] [Pub Med]
- Zekavat OR, Karimi MY, Amanat A, Alipour F. A randomised controlled trial of oral zinc sulphate for primary dysmenorrhoea in adolescent females. Aust N Z J Obstet Gynaecol. 2015;55(4):369-373.
[Crossref] [Google Scholar] [Pub Med]
- Farrah AM, Halim B, Kaban Y. Effectiveness of zinc supplementation in treating dysmenorrhea. Bali Med J. 2017;6(1):34-7.
- Sangestani G, Khatiban M, Marci R, Piva I. The positive effects of zinc supplements on the improvement of primary dysmenorrhea and premenstrual symptoms: A double-blind, randomized, controlled trial. J midwifery reproductive health. 2015;3(3):378-384.
- Teimoori B, Ghasemi M, Hoseini ZS, Razavi M. The efficacy of zinc administration in the treatment of primary dysmenorrhea. Oman Med J. 2016;31(2):107-111.
[Crossref] [Google Scholar] [Pub Med]
- Hikisz P, Bernasinska-Slomczewska J. Beneficial properties of bromelain. Nutrients. 2021;13(12):4313.
[Crossref] [Google Scholar] [Pub Med]
- Kerr F, Dawson A, Whyte IM, Buckley N, Murray L, Graudins A, et al. The Australasian Clinical toxicology investigators collaboration randomized trial of different loading infusion rates of N-acetylcysteine. Ann Emerg Med. 2005;45(4):402-408.
[Crossref] [Google Scholar] [Pub Med]
Citation: Estrada Z, Carmona F (2023) Study of the Recommended Dosage of the N-Acetyl Cysteine, Alpha Lipoic Acid, Bromelain and Zinc Preparation for the Treatment of Dysmenorrhea. J Pain Manage Med. 9:191.
Copyright: �© 2023 Estrada Z, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

