Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- Google Scholar
- SHERPA ROMEO
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2020) Volume 8, Issue 7
Simultaneously Fenestrated Thoracic Endovascular Repair in Aortic Arch and Thoraco Abdominal Saccular Aneurysms
Akiko Yamagata*, Satoru Domoto, Takashi Azuma, Yoshihiko Yokoi, Minako Hayakawa, Shogo Isomura and Hiroshi NiinamiReceived: 06-Oct-2020 Published: 27-Nov-2020, DOI: 10.35248/2329-6925.20.8.401
Abstract
A 71-year-old man with a history of mitral valve repair presented with distal arch and thoracoabdominal saccular aneurysms. Echocardiography showed a low ejection fraction and moderate residual mitral regurgitation. Open surgery and debranching Thoracic Endovascular Aortic Repair (TEVAR) for these aneurysms with two administrations of general anesthesia were considered high risk for this patient. We successfully performed two simultaneous procedures: fenestrated total arch TEVAR for one vessel reconstruction for the saccular aneurysm of the distal arch, and fenestrated thoracoabdominal TEVAR for three vessel reconstructions for thoracoabdominal saccular aneurysms. The patient’s postoperative course was uneventful.
Keywords
One-stage surgery; Fenestrated total arch TEVAR; Fenestrated thoracoabdominal TEVAR
Introduction
Although fenestrated and thoracoabdominal total arch thoracic endovascular aortic repair (TEVAR) face several challenges, evidence suggests that they are minimally invasive [1]. Either one-or two-stage surgery is the optimal therapeutic strategy for concomitant thoracic and abdominal aortic disease. One-stage surgery is reportedly associated with spinal cord ischemia. On the other hand, problems in time and technique of two-stage surgery may increase the risk of residual aneurysm rupture [2]. Recently, the uses of more sophisticated devices have enabled simultaneous treatment. This is the first report of simultaneous fenestrated total arch TEVAR with one vessel reconstruction of a distal arch saccular aneurysm and three vessel reconstructions via fenestrated thoracoabdominal TEVARs for thoracoabdominal saccular aneurysms.
Case Report
Informed consent was obtained from the patient for publication of this case report and accompanying images, and the study was approved by the appropriate ethics review board.
A 71-year-old man presented to our hospital with a thoracic aortic aneurysm (TAA) and thoracoabdominal aneurysm (TAAA). He underwent mitral valve repair 14 years prior. Computed tomography (CT) revealed saccular TAA at the distal arch and saccular TAAA just above the left renal artery (RA) (Figure 1). His echocardiography revealed a low ejection fraction of 28% and moderate residual mitral regurgitation. We considered that even open surgery and debranching TEVAR for these aneurysms together with two administrations of general anesthesia placed this patient at a high risk. It is difficult to reconstruct the thoracoabdominal aorta with an off-the-shelf device. We also considered that twostage surgery would increase residual rupture risk because of the saccular nature of his aneurysms. After critiquing all of our options, we determined simultaneous total fenestrated TEVAR for aortic arch and thoracoabdominal saccular aneurysms would be the least invasive.
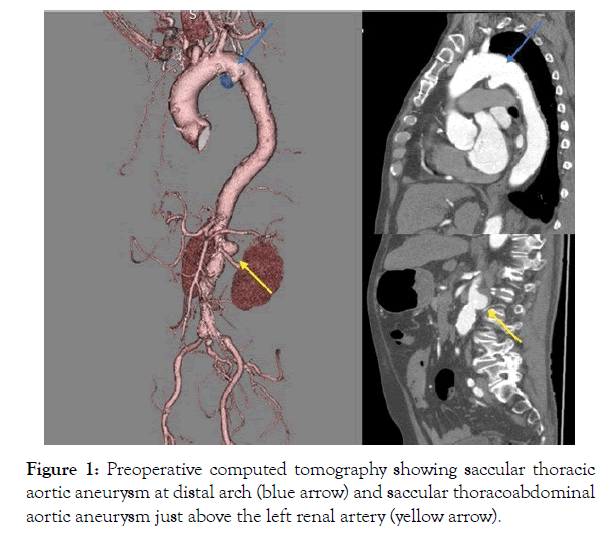
Figure 1: Preoperative computed tomography showing saccular thoracic aortic aneurysm at distal arch (blue arrow) and saccular thoracoabdominal aortic aneurysm just above the left renal artery (yellow arrow).
Before starting the surgery, we prepared the physician-modified fenestrated stent grafts, namely, a Najuta Thoracic Stent Graft System (Kawasumi Laboratories.Inc., Tokyo, Japan) with three holes, and a Zenith Alpha™ Thoracic Endovascular Graft (William Cook Europe, Bjaererskov, Denmark) with four holes (Figure 2). Hydrogel-reinforced fenestrations were made using AZUR® Hydro Coils® (Terumo Corporation, Micro Vention Inc, USA, CA), which were fixed around each fenestration to achieve easy cannulation and rigid connection with a bridging stent. We made an “access window” on the cranial and caudal sides of the Zenith Alpha™ graft, which was a hole that was opened to communicate from the outside to the inside of the stent graft. One loop of EN Snare® (Merit Medical Systems, Inc., USA, UT) was sutured around thehole as an X-ray opaque marker.
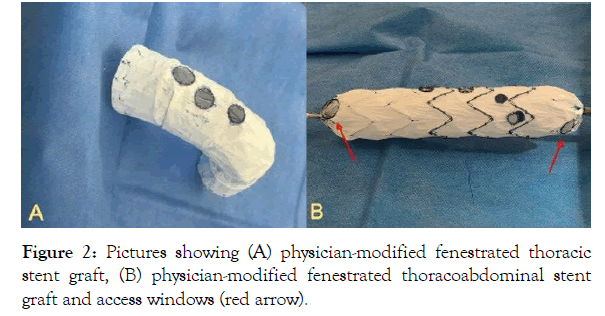
Figure 2: Pictures showing (A) physician-modified fenestrated thoracicstent graft, (B) physician-modified fenestrated thoracoabdominal stent graft and access windows (red arrow).
Under general anesthesia, we placed in advance Zenith® TX2® TAA Endovascular Grafts with Pro-Form (William Cook Europe, Bjaererskov, Denmark) at zone 3 of the distal arch via the right common femoral artery. Then, we placed the Najuta Thoracic Stent Graft System at the aortic arch in zone 0. We placed GORE® VIABAHN® Endoprosthesis (W. L. Gore & Associates, Flagstaff, Arizona, USA) at the left sub clavian artery (LSA) to connect it to the port of the Najuta Thoracic Stent Graft System to prevent migration and type 3 endoleak. Before full deployment, we placed afenestrated Zenith Alpha™ and cannulated the superior mesenteric artery (SMA) and bilateral RA from the access window. We placed the VIABAHN® Endoprosthesis in the SMA and bilateral RA to connect it to the port of the Zenith Alpha™. We placed the GORE® EXCLUDER® AAA Endoprosthesis cuff (W. L. Gore & Associates, Flagstaff, Arizona, USA) to cover the access window. No endoleak was observed on the final aortography. We maintained the mean arterial pressure>90 mmHg during the procedure by administering catecholamine. The procedure time was 349 minutes, fluoroscopy time was 107 minutes, and the amount of contrast medium was 180 mL.
The patient’s postoperative course was uneventful. Postoperative CT showed no endoleak and patency of the branches (Figure 3). Two years after surgery, CT imaging confirmed that TAA did not expand, while TAAA appeared to have shrunk. There were no findings of endoleak and aneurysmal enlargement at the two-year follow-up.
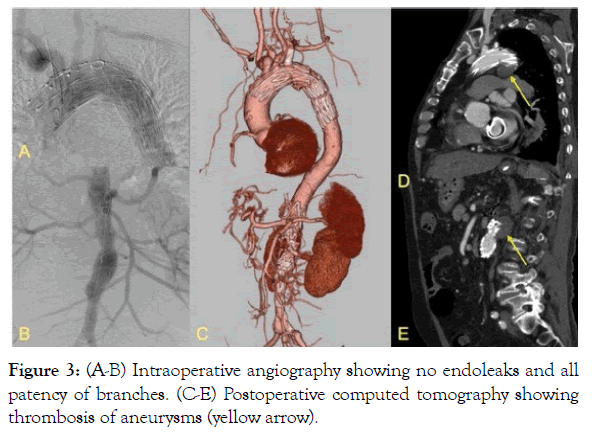
Figure 3: (A-B) Intraoperative angiography showing no endoleaks and all patency of branches. (C-E) Postoperative computed tomography showing thrombosis of aneurysms (yellow arrow).
Results and Discussion
Despite our positive outcomes, it remains controversial whether one- or two-stage surgery is the optimal therapeutic strategy for patients with concomitant thoracic and abdominal aortic disease. One-stage surgery is reportedly associated with spinal cord ischemia. Conversely, two-stage surgery may increase the risk of a residual aneurysm rupture as well as the risks of subjecting high-risk patients to two administrations of general anesthesia. Nonetheless, the feasibility of one-stage surgery has been previously reported [2,3].
Of all TEVAR complications, SCI is the most devastating. Independent risk factors for the development of delayed onset SCI include perioperative hypotension (mean arterial pressure<70 mmHg), concomitant thoracic and abdominal aortic repair, and left subclavian artery coverage without revascularization. The simultaneous closure of two independent arterial spinal cord vessels, particularly when combined with hypotension after device deployment, is reportedly the most important risk factor for symptomatic SCI. Therefore, it is necessary to prevent perioperative hypotension [4,5]. We performed one-stage surgery with a mean arterial pressure>90 mmHg during the procedure using catecholamine, and there were no subsequent findings of neurologic impairment.
The main difficulty of fenestrated TEVAR is accurately positioning the fenestrations. Given the variations in aortic arch anatomy, it is necessary to customize devices so they suit each individual’s anatomy, as off-the-shelf devices lack customization features and are therefore unlikely to produce similarly positive outcomes across patients [6]. Therefore, fenestrated total arch TEVAR was performed with a physician-modified fenestrated stent graft, which is not a practice unique to this case study [7].
In our patient, we used hydrogel-reinforced fenestration with AZUR® Hydro Coils® fixed around each fenestrated hole to achieve easy cannulation and rigid connection with a bridging covered stent to prevent type 3 endoleak. AZUR® Hydro Coils® consist of a platinum wire covered by a hydrogel polymer. Once the coils are placed in a blood vessel, the hydrogel is activated upon contact with the blood and subsequently commence the process of volume expansion. Hydrogel increases to approximately three to four times its original size [8].In our case, the hydrogel coating expanded by 80% within 3 min and reached maximal expansion approximately 20 minutes after it was deployed. It serves as a marker and prevents endoleak from the connection of the fenestrated hole of the stent graft and the reconstructed branch. We also performed fenestrated thoracoabdominal TEVAR using this technique. We reconstructed the LSA, SMA, and bilateral RA to prevent type 3 endoleak because they were close to the aneurysms.
Conclusion
Simultaneous total fenestrated TEVAR for aortic arch and thoracoabdominal saccular aneurysms produced positive results without neurological complications. We therefore recommend hydrogel-reinforced fenestration as a useful technique for endoleak prevention. It was an effective treatment for a patient who was at a high risk for thoracotomy, laparotomy, and debranching TEVAR.
REFERENCES
- David A, Grace J. TEVAR: Endovascular Repair of the Thoracic Aorta. Semin Intervent Radiol. 2015;32:265-271.
- Kirkwood ML, Pochettino A, Fairman RM,Jackson BM, Wang GJ, Szeto WY, et al. Simultaneous thoracic endovascular aortic repair and endovascular aortic repair is feasible with minimal morbidity and mortality. J Vasc Surg. 2011;54:1588-1591.
- Guo Y, Cai H, Yang B, Jin H. Simultaneous endovascular repair for thoracic and abdominal aortic pathologies: Early and midterm results. Ann Vasc Surg. 2017;40:178-182.
- Xue L, Luo S, Ding H, Zhu Y, Liu Y, Huang W, et al. Risk of spinal cord ischemia after thoracic endovascular aortic repair. J Thorac Dis. 2018;10:6088-6096.
- Domoto S, Azuma T, Nakazawa K, Yokoi Y, Hayakawa M, Yamagata A. Safety and efficacy of the percutaneous thoracic endovascular repair with regional anesthesia. Gen Thorac Cardiovasc Surg. 2020;1-7.
- Joseph G. Fenestrated total arch thoracic endovascular aortic repair: Coming of age. Adv Interv Cardiol. 2019;15:387-390.
- Furuta A, Azuma T, Yokoi Y, Domoto S, Niinami H. The midterm results of thoracic endovascular aortic repair with a precurved fenestrated endograft in zone 0-1. Eur J Cardiothorac Surg. 2020;58:722-729
- Ferral H. Hydrogel-coated coils: Product description and clinical applications. Semin Intervent Radiol. 2015;32:343-348.
Citation: Yamagata A, Domoto S, Azuma T, Yokoi Y, Hayakawa M, Isomura S, et al. (2020) Simultaneously Fenestrated Thoracic Endovascular Repair in Aortic Arch and Thoraco Abdominal Saccular Aneurysms. J Vasc Med Surg.8:401
Copyright: © 2020 Yamagata A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

