Citations : 2345
Dentistry received 2345 citations as per Google Scholar report
Indexed In
- Genamics JournalSeek
- JournalTOCs
- CiteFactor
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2020) Volume 10, Issue 7
Shear Bond Strengths of 3 Commonly Used Orthodontic Adhesives
Samaneh Shams1, Stefan Abela2*, Manoharan Andiappan3, Alireza Hajiheshmati1 and Dirk Bister12Norfolk and Norwich University, Hospital NHS Foundation Trust, Private Practice, London and Ely, Cambridgeshire, UK
3Dentistry, Oral and Craniofacial Sciences, King’s College London, London, UK
Received: 27-Aug-2020 Published: 15-Sep-2020, DOI: 10.35248/2161-1122.20.10.568
Abstract
Background: The purpose of this study was to compare the Shear Bond Strengths (SBS) of three types of orthodontic adhesives and to compare the Adhesive Remnant Index (ARI) after debonding.
Materials and Methods: One hundred and seventy-four upper central incisors were extracted and randomly divided to 6 groups (n=29) based on the type of adhesive and two-time intervals post bonding (30 minutes (T1) and 24 hours (T2)): 1) Transbond XT™ 2) BracePaste®, 3) GoTo™. Stainless steel orthodontic brackets were bonded to the teeth. Debonding was completed by an instron machine and shear bond strength recorded together with the ARI following examination under stereo optical microscope with magnification of 10x. Normal distribution was tested using histograms, box plots, the Shapiro-Wilks test and the Kolmogorov-Smirnov’s test. The linear correlation between shear bond strength and ARI score was measured using Pearson’s correlation coefficient by individual test groups and for pooled data. To examine significance of ARI score by group multiple chi-square testing was used. All the analyses were carried out using SPSS version 25.0 and Stata version 15.0.
Results: The bond strength of Transbond XT™ was the highest and the strengths at T1 and T2 were not statistically different. The statistical significance was set at 5%. The bond strength of GoTo™ adhesive significantly increased from T1 (200.49N ± 49.77) to T2 (234.89N ± 39.83). BracePaste® showed a statistically significant reduction of its bond strength after 24 hours; 165.07 ± 22.56, down from 187.40N ± 36.90 at T1. This was also significantly less than for the former two adhesives. Water ageing of 24 hrs had a positive impact on Transbond™ and GoTo™ but a negative one on BracePaste®. Transbond XT™ showed the highest score of 3 for ARI at T1 70% and T2 46% followed by GoTo 52% and 35% and BracePaste® 48% and 33%.
Conclusion: Transbond XT™ and GoTo™ adhesives showed superior SBS at T1 and showed statistically higher SBS at T2 than for BracePaste®
Keywords
Shear bond strength; Orthodontic adhesive; Adhesive remnant index
Introduction
Adhesive bond strength is of importance in the successful practice of orthodontics as continuous failure of orthodontic appliances increases the cost of treatment, lengthens treatment time [1] and affects chair side time [2]. Anterior masticatory forces range between 13 kg-15 kg while posterior masticatory forces can exceed 30 kg [3]. An ideal adhesive should exhibit acceptable shear bond strength to withstand functional forces during orthodontic treatment, and simultaneously allow bracket removal without causing iatrogenic damage to the enamel surfaces. A minimum recommended clinical bond strength of 5.9 MPa-7.8 MPa has been previously suggested [4].
The bonding of most orthodontic components is carried out using composite materials. Aesthetics, speed, and comfort are the principal reasons for the popularity of these materials [4]. Alternative materials such as glass ionomer cements have been suggested in research and clinical practice although with less success due to their inferior mechanical properties. Most clinicians prefer composite resins for the attachment of orthodontic brackets to teeth [5].
Following the introduction of the acidetch technique [6] and the direct bonding of orthodontic brackets by Newman 1965 [7], a variety of adhesive materials been introduced for clinical use. Early generations of composites were chemical-cure; however, clinicians were unable to adequately control the setting time. The first in vitro study by Tavas et al. [8] examined the use of an ultraviolet curing light to polymerise composite resins when orthodontic bonding. This breakthrough allowed clinicians enough chairside time to accurately position brackets.
The aims and objectives of this study were to compare the Shear Bond Strength (SBS) and failure response of Transbond XT™, GoTo™ and BracePaste® in vitro. The effect of time on their bond strength at T1, 30 minutes post bonding and at T2, 24 hours post bonding was also assessed. In previous studies, Transbond XT™ has shown superior bond strength in comparison to other composite resins [9-12]. BracePaste® and Go-To™ adhesives have been introduced to the market more recently, but there has been no studies comparing bond strength of the three materials.
The null hypotheses (H0) was that there is no difference in the SBS between the three tested adhesives and that there is no difference in the failure response denoted by the Adhesive Remnant Index (ARI) between same three tested adhesives at p<0.05.
Materials and Methods
One hundred and seventy-four previously extracted and intact upper central incisors were collected. The exclusion criteria ruled out teeth with caries, restorations, enamel hypoplasia, enamel defects, and cracks. All teeth were directly examined under normal surgery light and those exhibiting enamel infractions were excluded from the study [13].
In accordance with research guidelines, no ethical committee approval was needed for this study due its in vitro nature. All teeth obtained were previously extracted due to clinical reasons and consent was obtained at the clinical stage from patients prior to the extraction procedure.
All collected teeth were immersed in distilled water containing thymol crystals (0.1% weight/volume) to inhibit bacterial growth. All the samples were stored in dark conditions at 10°C ± 5°C [14]. The teeth were then embedded in silicon rubber moulds filled with cold cured acrylic to a level 1 mm apical to the cement enamel junction. Following embedding, all the sampled teeth were checked for parallelism of their labial surface using an analysing rod.
The bonding procedure was standardised and 37% phosphoric acid was applied to the enamel surface for 30 seconds and rinsed with water for 20 seconds before drying with oil-free compressed air until the tooth surface appeared frosted. Transbond XT™ primer (3M Unitek, Monrovia, CA, USA) was applied and gently distributed with an oil-free compressed air to ensure that a thin layer of primer remained on the surface. Specimens were then light cured with light (XL 3000 3M Dental Products, Model 5530-134) for 10 seconds.
Teeth were randomly allocated to 6 groups of 29 each. For all samples, upper central incisor metal brackets (94 upper right and 80 upper left) were bonded (Victory series™, slot size 0.022” × 0.028”, MBT Appliance System Prescription, 3M/Unitek, Monrovia, CA, USA).
Group 1: Transbond XT™ light cure orthodontic adhesive was applied and tested for shear bond strength 30 minutes post bonding
Group 2: Transbond XT™ light cure orthodontic adhesive applied and tested for bond strength 24 hours post bonding
Group 3: BracePaste® light cure orthodontic adhesive used (American orthodontics, Washington, USA) and tested for bond strength 30 minutes post bonding
Group 4: BracePaste® light cure orthodontic adhesive applied and tested for bond strength 24 hours post bonding
Group 5: GoTo™ light cure orthodontic adhesive used (Reliance orthodontics, IL, USA) and tested for bond strength 30 minutes post bonding.
Group 6: GoTo™ light cure orthodontic adhesive used and tested for bond strength 24 hours post bonding.
Table 1 shows the manufacturer’s details of the components of the three different orthodontic adhesives used [15].
| Brand name manufacturer | Monomer | Filler | Percentage of inorganic fillers |
|---|---|---|---|
| BracePaste American Orthodontics, Sheboygan, WI, USA | Bis-EMA TD | Bis-GMA and Bis-EMA particles are used as resin fillers. Silanated quartz, silaneted silica | 72% |
| GoTo, Reliance Orthodontics, IL, USA | Not available | UDMA, Bis-GMA | N/A |
| Transbond XT, 3M, Unitek, CA, USA | Bis-EMA, Bis-GMA | Silaneted quartz, silaneted silica. | 70-80% |
Key: Bis-GMA: Bisphenol A-glycidyl Dimethacrylated; Bis-EMA: Ethoxylated Bisphenol Adimethacrylate; UDMA: Urethane Dimethacrylate; TD: Tetramethylene Dimethacrylate
Table 1: Description of the adhesive materials used.
All brackets were coated with a small layer of adhesive, positioned and subjected to 300 g of force using a force gauge (Correx Co, Bern, Switzerland) for 10 seconds as described by Bishara et al. [16]. Excess bonding resin was removed using a small scaler. An Extech force gauge (Model:475040, FLIR Commercial System, 9 Townsend West, Nashua, NH 03063, USA) was used to ensure a uniform pressure and adhesive thickness.
The adhesives were cured with a 3 M Elipar S10 light curing unit with a wavelength of 430 nm-480 nm and an intensity of 1200 mW/cm2. The tip of the light cure unit was placed as close as possible to the bracket and cured on both proximal aspects for 10 seconds each side.
The samples to be tested at 24 hours were stored in distilled water in an incubator at 37°C before testing. The remaining samples were prepared for the chisel shear test 30 minutes post bonding.
The specimens were mounted in an Instron testing machine (Model 5569a, Instron Cooperation, 825 University Ave, Norwood, MA, 02062-2643, USA). A crosshead speed of 0.5 mm/ min was occlusogingivally applied to the base of the bracket using a chisel. The force required to dislodge the bracket was measured in Newtons (N).
During the shear bond test, 19 of the specimens were excluded as either the acrylic or the enamel surfaces fractured. Four of the failures were in group 3, four were in group 5, five were in group 1, two were in group 4, one in group 6 and three were in group 2.
The results of each test were recorded digitally using Bluehill ® 2 software (Norwood, MA, USA). The bond strength in Newtons was then calculated on the basis of a bracket area of 9.01 mm2.
The Adhesive Remnant Index (ARI) by Årtun and Bergland [17] shown in Table 2, was used for the assessment of residual adhesive and the site of bond failure. All debonded enamel surfaces were examined under a stereooptical microscope at ten times magnification [17].
| 0 | No adhesive on the tooth |
| 1 | <1/2 of the adhesive on the tooth |
| 2 | >1/2 of the adhesive left on the tooth |
| 3 | All adhesive left on the tooth and distinct impression of the bracket mesh |
Table 2: The Adhesive Remnant Index (ARI) by Årtun and Bergland [17].
Sample size calculation
A power calculation for this study was based on an Analysis of Variance (ANOVA) for comparing the mean bond strength between 3 different adhesives at two time points. A study with an effect size of 0.3 and a power of 80% was estimated to require a total sample of 111 (19 per adhesive per time point) to test the principal and interactive effects of mean bond strength at the 5% level of confidence, using two tailed tests. The power calculation was carried out using G*Power software 3.1.9.2.
Statistical analysis
The difference in mean bond strengths between the adhesives at different times and their interactions were compared using linear models after confirming normal distribution. Normal distribution was tested using histograms, box plots, the Shapiro-Wilks test and the Kolmogorov-Smirnov’s test. The statistical significance was set at 5%.
The linear correlation between shear bond strength and ARI score was measured using Pearson’s correlation coefficient by individual test groups and for pooled data. To examine significance of ARI score by group multiple chi-square testing was used. All the analyses were carried out using SPSS version 25.0 and Stata version 15.0.
Results
The bond strengths of Transbond XT™ at T1 and T2 were not statistically different; however, the bond strength for GoTo™ adhesive significantly increased from T1 (200.49N ± 49.77) to T2 (234.89N ± 39.83). BracePaste ® showed a statistically significant reduction in bond strength after 24 hours at T2 to 165.07 ± 22.56, down from 187.40N ± 36.90. These strength values were statistically significantly lower than for Transbond XT™ and GoTo™. Table 3 below show the mean bond strengths at T1 and T2 and the comparison between the different adhesives’ bond strengths at T1 and T2 respectively.
| Time | Adhesive | n | Mean (SD) | Median (min, max) |
|---|---|---|---|---|
| 30 minutes (T1) | BracePaste® | 25 | 187.40 (36.90) | 190.55 (108.12, 280.63) |
| GoTo™ | 25 | 200.49 (49.77) | 191.52 (125.99, 294.87) | |
| Transbond XT™ | 24 | 233.34 (49.76) | 229.18 (150.20, 323.51) | |
| 24 hours | BracePaste® | 27 | 165.07 (22.56) | 163.41 (127.72, 203.92) |
| GoTo™ | 28 | 234.89 (39.83) | 234.20 (167.66, 298.36) | |
| Transbond XT™ | 26 | 252.53 (39.72) | 257.77 (193.06, 320.22) |
Key: n: Number; SD: Standard Deviation; Min: Minimum; Max: Maximum
Table 3: Summary statistics of bond strength in Newtons, for various adhesives and different times.
Table 4 also highlights that at 30 minutes, there was a statistically significant difference in bond strength between GoTo™ and Transbond XT™; however, this difference was nullified at 24 hours, T2. At 30 minutes there was a statistically significant difference in bond strength between BracePaste® and Transbond XT™ and this difference was consistent throughout the observation period until T2. The bond strength difference for BracePaste® and GoTo™ at 30 minutes was not significant; however, the difference became significant at 24 hours.
| Factor | Effect | 95% confidence interval | P-value |
|---|---|---|---|
| At 30 mins | |||
| BracePaste® vs GoTo™ | -13.09 | -35.74 to 9.55 | 0.26 |
| BracePaste® vs TransBond XT™ | -45.94 | -68.82 to -23.06 | <0.0001* |
| GoTo™ vs Transbond XT™ | -32.85 | -55.73 to -9.97 | 0.005 |
| At 24 hours | |||
| BracePaste® vs GoTo™ | -69.81 | -91.41 to -48.42 | <0.0001* |
| BracePaste®vs TransBond XT™ | -87.45 | -109.45 to -65.45 | <0.0001* |
| GoTo™ vs Transbond XT™ | -17.64 | -39.44 to 4.17 | 0.112 |
| Between Time points (30 mins vs 24 hours) | |||
| BracePaste® | 22.32 | 0.10 to 44.54 | 0.049* |
| GoTo™ | -34.4 | -56.43 to -12.37 | 0.002* |
| Transbond XT™ | -19.19 | -41.85 to 3.47 | 0.1 |
*Denotes statistically significant
Table 4: Results of linear model for comparing bond strength between adhesives and time.
Figure 1 illustrates the above findings with the adhesives’ mean bond strength variation over time between T1 and T2.
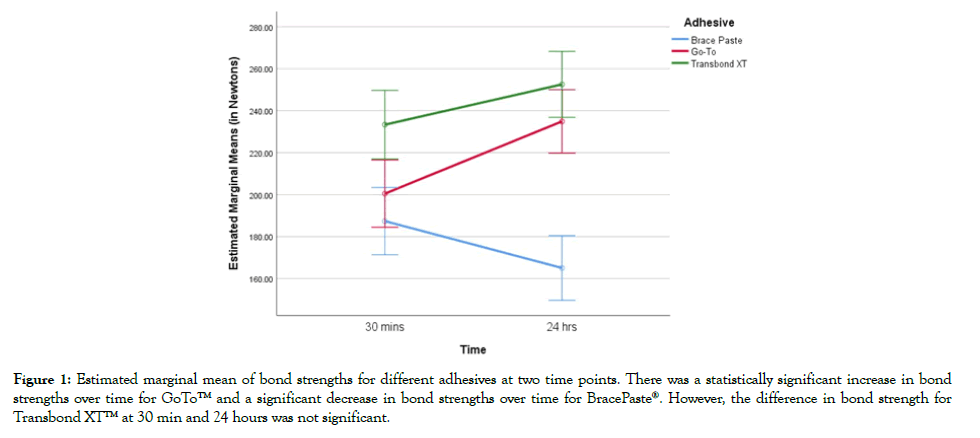
Figure 1: Estimated marginal mean of bond strengths for different adhesives at two time points. There was a statistically significant increase in bond strengths over time for GoTo™ and a significant decrease in bond strengths over time for BracePaste®. However, the difference in bond strength for Transbond XT™ at 30 min and 24 hours was not significant.
*Denotes statistically significant.
The adhesive remnant index for all groups at 30 minutes, showing no association between the adhesive index and the materials at 30 minutes (p=0.07) is tabulated in Table 5, whilst Table 6 summarises the adhesive remnant index for all groups at 24 hours. There was no association between the adhesive index and the materials at 24 hours (p=0.15).
| Material | Index 0 | Index 1 | Index 2 | Index 3 |
|---|---|---|---|---|
| BracePaste® | 0% | 20% | 32% | 48% |
| GoTo™ | 4% | 0% | 44% | 52% |
| Transbond XT™ | 4.20% | 4.20% | 20.80% | 70.80% |
Table 5: Frequency distribution of ARI at 30 minutes in each adhesive group.
| Material | Index 0 | Index 1 | Index 2 | Index 3 |
|---|---|---|---|---|
| BracePaste® | 0% | 10.70% | 35.70% | 53.60% |
| GoTo™ | 0% | 3.70% | 33.30% | 63.00% |
| Transbond XT™ | 7.70% | 3.80% | 42.30% | 46.20% |
Table 6: Frequency distribution of ARI at 24 hours in each adhesive group.
Discussion
The introduction of the acidetch technique to the practice of orthodontics fostered the development of resin materials. Since then, numerous adhesives have been commercialised and introduced to the market with claims of achieving an ideal bond strength. The light cure resins used in this study were Transbond XT™, GoTo™ and BracePaste®.
Transbond XT™ bond strength has been well researched and documented in past literature [9,10,12].
The GoTo™ adhesive has been recently launched onto the market with no evidence of superiority. BracePaste® is also a comparatively new orthodontic adhesive. Its main active components are Bis- EMA, Ethoxylated bisphenol A-dimethacrylate and TD: Tetramethylene dimethacrylate.
The manufacturer claims comparable bond strength to Transbond XT™ as the Bis-GMA and Quartz Silica components are similar. The resin’s increased viscosity has been proposed to aid positioning and prevent ‘drifting’ of the brackets. However to date, no clinical trials have been conducted to analyse its shear bond strengths and efficiency and the manufacturer’s claims remain scientifically unfounded.
Bond strength values of 6 MPa-8 MPa have been determined as clinically acceptable by Reynolds and many others [18]; however, caution needs to be applied when interpreting results of in vitro studies, due to the potential higher strength readings in comparison to in vivo situations [12,19,20]. Intra-oral variable factors such as saliva, masticatory forces and acid which can lead to shear bond strength reduction that are not accounted for in laboratory studies [21].
The results of this study showed that the highest bond strength values at both 30 minutes and 24 hours were achieved with Transbond XT™ (233.34 N ± 49.76 at 30 minutes and 252.53 N ± 39.72 at 24 hours). GoTo™ showed slightly lower values at 200.49 N ± 49.77 at T1 and 234.89 ± 39.83 at T2. There was no statistically significant difference between GoTo™ and Transbond XT™.
BracePaste® demonstrated the lowest bond strength values (187.40 N ± 36.90 at 30 minutes and 165.07 N ± 22.56 at 24 hours).
The differences in bond strength between the three different composite resins could have arisen due to differences in filler content and resin composition. A high concentration of filler particles of different sizes leads to better mechanical properties, with lower polymerisation shrinkage and a higher degree of cure. The strongest bond for metal orthodontic brackets is achieved with adhesives containing highly filled Bis-GMA diacrylate resin [22]. Transbond XT™ has been widely used for comparison and the bond strength values of this material achieved here are in accordance with previous studies [11,23]. There have been no previous studies comparing the bond strengths of GoTo™ and BracePaste® adhesives.
The bond strengths of GoTo™ and Transbond XT™ groups increased favourably between T1 and T2 which is similar to the findings reported by Bishara et al. and Alexandra et al. [16,23]. The increase in bond strength with time arises after the initial release of free radicals at the periphery of the resin and the internal diffusion of the free radicals occur over time, which results in further polymerisation of the resins under the bracket base [24].
BracePaste® not only exhibited lower shear bond strengths, it also showed a significant reverse correlation between bond strength value and time. At T2, the bond strength value was significantly less than at T1. This negative correlation with time could have arisen due to hydrolysis of the adhesive following exposure to fluids. This exposure resulted in a degradation of the material and a decrease in the mechanical properties.
In this study, 90% of all brackets debonded with an ARI score of 2 and 3 at both T1 and T2. Only 10% had an ARI score of 0 or 1. Low ARI scores (0 or 1) could be deemed advantageous due to the reduced amount of adhesive needed to be removed from the tooth surface [16,25,26]. In contrast, higher ARI scores of and 2 and 3 could be unfavourable due to the increased need of prolonged adhesive removal resulting in enamel damage [27-29]. Contemporary evidence by Faria et al. [30] suggests that there is no evidence to suggest iatrogenic damage following a debonding procedure as newer aluminium oxide disc polishing system has shown to remove adhesive without significantly damaging the tooth surface. Higher ARI scores (2 or 3) may be more desirable in clinical orthodontics.
Conclusion
Transbond XT™ appeared to offer the best shear bond strength which may have a positive translation to the clinical setting. The second best adhesive’s shear bond strength was GoTo™ followed by BracePaste®. This superiority was proved at both T1 and T2 timescales. This study further suggests that Transbond XT™ and GoTo™ displayed comparable bond strengths and the difference in bond strengths was not statistically significant. The difference between these two adhesives was even closer after 24 hours and the strengths for both adhesives increased between T1 and T2. This study allows clinicians to consider GoTo™ as a more cost effective alternative adhesive to Transbond XT™ without affecting the clinical performance expectations. Clinicians could also advise patients that the strength of adhesive used increases with time and extra caution should be taken with the diet in the first 24 hours following placement of fixed appliances.
The specific conclusions of this study includes the following:
• No statistically significant difference was found between SBS of GoTo and BracePaste at 30 minutes
• Statistically significant differences between SBS of BracePaste vs Transbond XT and GoTo vs Transbond XT at 30 minutes
• No statistically significant difference was found between SBS of GoTo vs Transbond XT at 24 hours
• Statistically significant differences between SBS of BracePaste vs GoTo and Transbond XT at 24 hours
Conflict of Interest
The authors of this study do not hold any financial interests nor connections, direct or indirect, and there is no risk of bias in the work reported or the conclusions, implications or opinions stated. There is no commercial nor other sources of funding for any of the authors or for the associated department, personal relationships, or direct academic competition.
REFERENCES
- Jassem HA, Retief DH, Jamison HC. Tensile and shear strengths of bonded and rebonded orthodontic attachments. Am J Orthod. 1981;79:661-668.
- Jung MH. Survival analysis of brackets and tubes: A twelve-month assessment. Angle Orthod. 2014;84:1034-1040.
- Helkimo E, Carlsson GE, Helkimo M. Bite force and state of dentition. Acta Odontol Scand. 1977;35:297-303.
- Reynolds I. A review of direct orthodontic bonding. Br J Orthodont. 1975;2:171-178.
- Chitnis D, Dunn WJ, Gonzales DA. Comparison of in-vitro bond strengths between resin-modified glass ionomer, polyacid-modified composite resin, and giomer adhesive systems. Am J Orthod Dentofacial Orthop. 2006;129:e311-e336.
- Buonocore MG. A simple method of increasing the adhesion of acrylic filling materials to enamel surfaces. J Dent Res. 1955;34:849-853.
- Newman GV. Epoxy adhesives for orthodontic attachments: progress report. Am J Orthod. 1965;51:901-912.
- Tavas MA, Watts DC. Bonding of orthodontic brackets by transillumination of a light activated composite: an in vitro study. Br J Orthod. 1979;6:207-208.
- Chamda RA, Stein E. Time-related bond strengths of light-cured and chemically cured bonding systems: an in vitro study. Am J Orthod Dentofacial Orthop. 1996;110:378-382.
- Millett DT, Hallgren A, Cattanach D, McFadzean R, Pattison J, Robertson M, et al. A 5-year clinical review of bond failure with a light-cured resin adhesive. Angle Orthod. 1998;68:351-356.
- Rix D, Foley TF, Mamandras A. Comparison of bond strength of three adhesives: composite resin, hybrid GIC, and glass-filled GIC. Am J Orthod Dentofacial Orthop. 2001;119:36-42.
- Hajrassie MK, Khier SE. In-vivo and in-vitro comparison of bond strengths of orthodontic brackets bonded to enamel and debonded at various times. Am J Orthod Dentofacial Orthop. 2007;131:384-390.
- Zachrisson BU, Skogan O, Hoymyhr S. Enamel cracks in debonded, debanded, and orthodontically untreated teeth. Am J Orthod. 1980;77:307-319.
- Fox NA, McCabe JF, Buckley JG. A critique of bond strength testing in orthodontics. Br J Orthod. 1994;21:33-43.
- Hassan MN, Zinelis S, Hersberger-Zurfluh M, Eliades T. Creep, hardness, and elastic modulus of lingual fixed retainers adhesives. Materials (Basel). 2019;12:646.
- Bishara SE, Gordan VV, VonWald L, Jakobsen JR. Shear bond strength of composite, glass ionomer, and acidic primer adhesive systems. Am J Orthod Dentofacial Orthop. 1999;115:24-28.
- Artun J, Bergland S. Clinical trials with crystal growth conditioning as an alternative to acid-etch enamel pretreatment. Am J Orthod. 1984;85:333-340.
- Pickett KL, Sadowsky PL, Jacobson A, Lacefield W. Orthodontic in vivo bond strength: comparison with in vitro results. Angle Orthod. 2001;71:141-148.
- Murray SD, Hobson RS. Comparison of in vivo and in vitro shear bond strength. Am J Orthod Dentofacial Orthop. 2003;123:2-9.
- Hobson RS, Ledvinka J, Meechan JG. The effect of moisture and blood contamination on bond strength of a new orthodontic bonding material. Am J Orthod Dentofacial Orthop. 2001;120:54-57.
- Vilchis RJ, Hotta Y, Yamamoto K. Examination of six orthodontic adhesives with electron microscopy, hardness tester and energy dispersive X-ray microanalyzer. Angle Orthod. 2008;78:655-661.
- Sinha PK, Nanda RS, Duncanson MG, Hosier MJ. In vitro evaluation of matrix-bound fluoride-releasing orthodontic bonding adhesives. Am J Orthod Dentofacial Orthop. 1997;111:276-282.
- Vinagre AR, Messias AL, Gomes MA, Costa AL, João CR. Effect of time on shear bond strength of four orthodontic adhesive systems. Rev Port Estomatol Med Dent Cir Maxilofac. 2014;55:142-151.
- Greenlaw R, Way DC, Galil KA. An in vitro evaluation of a visible light-cured resin as an alternative to conventional resin bonding systems. Am J Orthod Dentofacial Orthop. 1989;96:214-220.
- Toledano M, Osorio R, Osorio E, Romeo A, de la Higuera B, Garcia GF. Bond strength of orthodontic brackets using different light and self-curing cements. Angle Orthod. 2003;73:56-63.
- Chang WG, Lim BS, Yoon TH, Lee YK, Kim CW. Effects of salicylic-lactic acid conditioner on the shear bond strength of brackets and enamel surfaces. J Oral Rehabil. 2005;32:287-295.
- Joseph VP, Rossouw PE. The shear bond strengths of stainless steel orthodontic brackets bonded to teeth with orthodontic composite resin and various fissure sealants. Am J Orthod Dentofacial Orthop. 1990;98:66-71.
- Yapel MJ, Quick DC. Experimental traumatic debonding of orthodontic brackets. Angle Orthod. 1994;64:131-136.
- Habibi M, Nik TH, Hooshmand T. Comparison of debonding characteristics of metal and ceramic orthodontic brackets to enamel: an in-vitro study. Am J Orthod Dentofacial Orthop. 2007;132:675-679.
- Faria JEM, Guiraldo RD, Berger SB, Correr AB, Correr SL, Contreras EF, et al. In-vivo evaluation of the surface roughness and morphology of enamel after bracket removal and polishing by different techniques. Am J Orthod Dentofacial Orthop. 2015;147:324-329.
Citation: Shams S, Abela S, Andiappan M, Hajiheshmati A, Bister D (2020) Shear Bond Strengths of 3 Commonly Used Orthodontic Adhesives. Dentistry 10: 568. doi: 10.35248/2161-1122.20.10.568
Copyright: © 2020 Shams S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : Nil

