Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- Ulrich's Periodicals Directory
- Access to Global Online Research in Agriculture (AGORA)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2021) Volume 12, Issue 1
Severe Rhinocerebral Mucormycosis Case Developed after COVID-19
Fatih Sargin, Mert Akbulut, Simay Karaduman and Hülya Sungurtekin*Received: 12-Jan-2021 Published: 02-Jan-2021, DOI: 10.36648/2155-9597.21.12.386
Abstract
In this article, a case of rhinocerebral mucormycosis developing after COVID-19 infection in a diabetic patient is presented. Early diagnosis and treatment of those high morbidity conditions is vital to better outcomes.
Keywords
Covid 19; Infection; Rhinocerebral mucormycosis
Introduction
Mucormycosis is an invasive fungal infection caused by mold fungi of the genus Mucor, Rhizopus, Rhizomucor and Absidia, which are in the Mucorales order of the Zygomycetes class [1]. The most common type is Rhizopus Oryzae and approximately 60% of mucormycosis cases in humans; it is responsible for 90% of the rhinocerebral form [2]. It is frequently seen in conditions where the immune system is suppressed such as uncontrolled diabetes, hematological malignancy, immunosuppressive and corticosteroid therapy. It is rarely seen in healthy individuals [3]. The most common clinical pictures are with rhinocerebral, pulmonary and cutaneous involvement. The area of involvement can be affected by the underlying condition. While rhinocerebral involvement is observed in diabetic patients, rhinocerebral and pulmonary involvement is observed in patients who develop neutropenia due to bone marrow transplantation and leukemia. Gastrointestinal involvement is more common in patients with malnutrition. Contamination occurs through inhalation. The phagocytic cells destroy the spores of the inhaled fungus, but in immunocompromised individuals, the spores can infect the vascular endothelium by invasion [2,4]. As we know that this is the first case of a patient in the literature that developed a rhinocerebral mucormycosis with extensive cavitary lesions is here reported after coronavirus disease (COVID-19).
Case Study
56-year-old female patient with a known diagnosis of anxiety disorder, presented to the external center emergency service with the complaints of respiratory distress and fatigue. The patient was hospitalized in Covid-19 intensive care because of hypoxia, hyperglycemia, electrolyte imbalance and metabolic acidosis, positive COVID-PCR test and ground glass areas on thorax CT. Covid-19 care and treatment, including corticosteroids (methylprednisolone 80 mg/day) was applied in intensive care for 7 days, and then he was transferred to the pandemic ward.
During the follow-up of the patient, proptosis in the right eye, restricted eye movements, edema and color change in the nasal area developed. In the otolaryngologist doctor evaluation of the patient, a dry appearance in the nasal cavity was detected, and biopsy and culture sampling was performed with pre-diagnoses of mucor and vasculitis. Paranasal sinus CT revealed no pathology other than mucosal edema. In the evaluation of infectious diseases specialitis, empirical antifungal therapy was recommended with mucor diagnosis. The patient was transferred to our intensive care unit due to the deterioration in the clinical condition of the patient.
When the patient was admitted to our intensive care unit, his general condition was moderate-poor, his breathing was spontaneous, with nasal cannula under 4 lt/min oxygen, Glasgow coma scale:13, TA:118/68 mmHg, heart rate:104 per minute, SpO2:95%, Fever:37.4°C. On physical examination, a wide area of necrotic tissue was observed in the nasal, maxillo-zygomatic region of the face (Figure 1). Culture was taken from the necrotic region for fungus. Infectious diseases and plastic surgery consultation was requested. Liposomal amphotericin B was started by infectious diseases consultant. Debridement to the infection site was planned by plastic surgery. Tracheostomy was performed on the patient on third day.
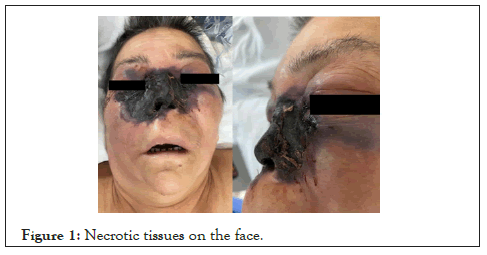
Figure 1: Necrotic tissues on the face.
Laboratory results in blood samples: hemoglobin:8.5 g/dl, white blood cell:8.0 k/uL, platelet:45 k/uL, lymphocyte:0.52 k/uL neutrophil to lymphocyte ratio:13.9, D-Dimer: 2906 ng/mL, ferritin:1076 ug/L, glucose:149 mg/dL, creatinine:1.21 mg/dL, Na:158 mmol/L, K:3.07 mmol/L, alanine amino transferases:20 IU/L, aspartate amino transferase:4 IU/L, CRP:116 mg/L, procalcitonin:3.52 ng/mL.
Infectious spread in bilateral frontal lobes, right temporal lobe, caudate nucleus and right basal ganglia were shown in the imaging technics. Abscess appearance was detected in the middle part of the pons. An appearance compatible with abscess was detected in both lateral ventricles and an appearance compatible with a 7 × 4 mm mycotic aneurysm was observed in the anterior communicating artery localization. Particular defects were observed in the nasal septum, nasal concha and both ethmoid cells. Widespread signal enhancements secondary to the infectious process involving the entire malar region extending to both sides of the neck, the retromaxillary area, both orbital structures of the infratemporal fossa, the supraorbital region including the cross-sections and the frontal region were observed (Figures 2 and 3). Multiple nodulescavitary lesions with a cystic-necrotic character and a diameter of 2 cm were detected in the upper lobes of both lungs included in the sections.
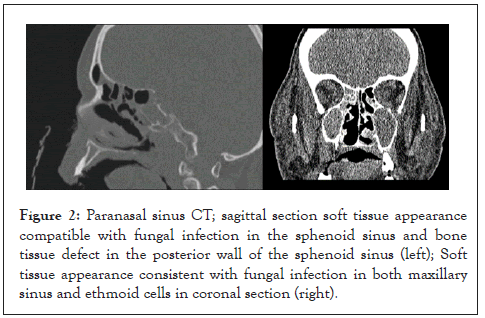
Figure 2: Paranasal sinus CT; sagittal section soft tissue appearance compatible with fungal infection in the sphenoid sinus and bone tissue defect in the posterior wall of the sphenoid sinus (left); Soft tissue appearance consistent with fungal infection in both maxillary sinus and ethmoid cells in coronal section (right).
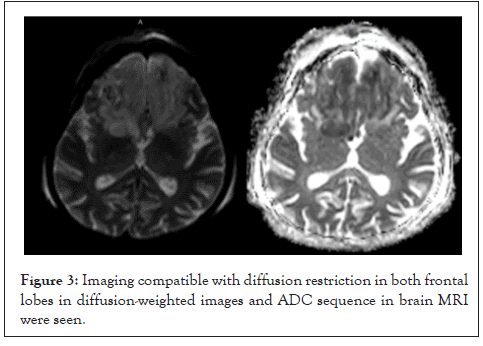
Figure 3: Imaging compatible with diffusion restriction in both frontal lobes in diffusion-weighted images and ADC sequence in brain MRI were seen.
After imaging, plastic surgery was consulted again in terms of operation and debridement, but it was stated that the patient have invasive fungal infection was not suitable for debridement due to the risk of fungal sepsis. Mucor was detected in the fungal culture taken from the lesion area and Acinetobacter baumani growth was detected in the blood culture.
Colimicin treatment was started in consultation with infectious diseases. The treatment of the patient was continued with intravenous antifungal. In the following days, the patient developed hypotension (MAP<65 mmHg) and vasopressor treatment was initiated with the diagnosis of septic shock, antibiotherapy was extended with the recommendation of infectious diseases, and the dose of liposomal amphotericin B was increased. The patient died on the 10th day of hospitalization.
Discussion
Mucormycosis is an angioinvasive mycosis thanks to fungi of the Mucorales. Counting on the clinical presentation it's classified as rhinocerebral, pulmonary, cutaneous, gastrointestinal, disseminated or other, which incorporates uncommon rareforms, like endocarditis, osteomyelitis, peritonitis, renal, etc. The foremost important conditions that predispose to mucormycosis, include Diabetes Mellitus (DM), with or without ketoacidosis, Hematological Malignancies (HM), other malignancies, transplantation, prolonged neutropenia, corticosteroids, hemochromatosis, trauma, neonatal prematurity, illicit intravenous drug use and malnourishment [5]. Recent report from India that included four hundred sixty five patients. It had been shown that rhino-orbital mucormycosis was the foremost common (315/465, 67.7%) presentation followed by pulmonary (62/465, 13.3%), cutaneous (49/465, 10.5%), et al. The predisposing factors included DM (342/465, 73.5%), malignancy (42/465, 9.0%), transplant (36/465, 7.7%), et al., [6].
Diabetes mellitus is that the leading underlying disease in patients with mucormycosis globally [7]. Diabetes has been shown as a risk factor for mucormycosis in 73.5% of cases in India 6. There are reports of mucormycosis related to short courses of corticosteroids [8]. In the ECMM European study 46% of the patients had received corticosteroids within the month before diagnosis of mucormycosis and 44% had received other immunosuppressive agents [9].
In our patient, the unstable high sugar level observed during the presentation brings to mind the possibility of a long-term diabetes that has not been diagnosed before and suggests that it may be the underlying cause of mucor infection. Giving steroid therapy to the patient can also be seen as another underlying cause for the development of mucor infection.
Lymphopenia is a common finding in patients infected with SARSCOV2 and may predispose to mucor infection with additional suppression of the immune system. This susceptibility has been documented especially by mucor infections observed in AIDS patients with lymphopenia [10,11]. This information suggests that lymphopenia associated with COVID-19 may also be a primary risk factor for mucor infection. However, in order to determine that COVID-19-associated lymphopenia is a single risk factor for mucor infection, it should be supported by other cases without additional risk factors.
We presented a case of a patient whose known comorbidity was diabetes for developing mucormycosis after COVID-19. He was hospitalised following the diagnosis of COVID-19 and managed with broad-spectrum antibiotics and corticosteroids (which are risk factors for fungal disease) similar to the literature [8]. It is known that COVID-19 may be associated with immune dysregulation and has been shown that patients with COVID-19 might be at risk of developing invasive fungal infections, such as candidiasis infection and invasive aspergillosis [12].
Conclusion
In conclusion, COVID-19 is considered an explanation for severe immunosuppression which may increase the danger to develop opportunistic infections. Early detection of symptoms for mucor like cheek swelling, blackening etc got to be reported immediately. Furthermore, if a CT scan finds a mucormycosis fungus, then there's a gold standard treatment and also removing dead tissue through surgery. Clinical suspicion and prompt treatment are fundamental to realize the cure of the disease. However, there are no reports of mucormycosis associated with COVID-19. Our patient was diagnosed with rhinoserebral mucormycosis after COVID-19, we don’t know whether the cause of death was invasive mucormycosis. More studies are necessary to determine if these two pathologies are related.
REFERENCES
- Eucker J, Sezer O, Graf B, Possinger K. Mucormycoses. Mycoses. 2001;44(7):253-260.
- Sugar AM. In: Mandell GL, Bennett JE, Dolin R(eds) Mandell, Douglas, and Bennett’s principles and practice of infectious diseases (5th edn), Churchill Livingstone, New York, USA, 2000.
- Bottone EJ, Weitzman I HB. Rhizopus rhizopodiformis: emerging etiological agent of mucormycosis. J Clin Microbiol. 1979;9(4):530-537.
- Shi BY, Lan L, Guo H Tan Y-F. Concomitant diabetic ketoacidosis and rhinocerebral mucormycosis: Report of a case. Chin Med J. 2004;117(7):1113-1115.
- Skiada A, Pavleas I, Drogari-Apiranthitou M. Epidemiology and diagnosis of mucormycosis: An Update. J Fungi. 2020;6(4):265.
- Patel A, Kaur H, Xess I, Michael JS, Savio J, Rudramurthy S, et al. A multicentre observational study on the epidemiology, risk factors, management and outcomes of mucormycosis in India. Clin Microbiol Infect. 2020;26(7):944.e9-944.e15.
- Jeong W, Keighley C, Wolfe R, Lee WL, Slavin MA, Kong DCM, et al. The epidemiology and clinical manifestations of mucormycosis: a systematic review and meta-analysis of case reports. Clin Microbiol Infect. 2019;25(1):26-34.
- Hoang K, Abdo T, Reinersman JM, Lu R, Higuita NIA. A case of invasive pulmonary mucormycosis resulting from short courses of corticosteroids in a well-controlled diabetic patient. Med Mycol Case Rep. 2020;29(1):22-24.
- Skiada A, Pagano L, Groll A, Zimmerli S, Dupont B, Lagrou K, et al. Zygomycosis in Europe: Analysis of 230 cases accrued by the registry of the European Confederation of Medical Mycology (ECMM) Working Group on Zygomycosis between 2005 and 2007. Clin Microbiol Infect. 2011;17(12):1859-1867.
- Sanchez MR, Ponge-Wilson I, Moy JA, Rosenthal S. Zygomycosis and HIV infection. J Am Acad Dermatol. 1994;1994(30):904-908.
- Klatt EC, Nichols L, Noguchi TT. Evolving trends revealed by autopsies of patients with the acquired immunodeficiency syndrome: 565 Autopsies in adults with the acquired immunodeficiency syndrome, Los Angeles, Calif, 1992-1993. Arch Pathol Lab Med. 1994;118(9):884-890.
- Koehler P, Cornely OA, Böttiger BW, Dusse F, Eichenauer DA, Fuchs F, et al. COVID-19 associated pulmonary aspergillosis. Mycoses. 2020;63(6):528–534.
Citation: Sargin F, Akbulut M, Karaduman S, Sungurtekin H (2021) Severe Rhinocerebral Mucormycosis Case Developed After COVID 19. J Bacteriol Parasitol. 12: 386.
Copyright: © 2021 Sargin F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

