Indexed In
- Open J Gate
- Cosmos IF
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
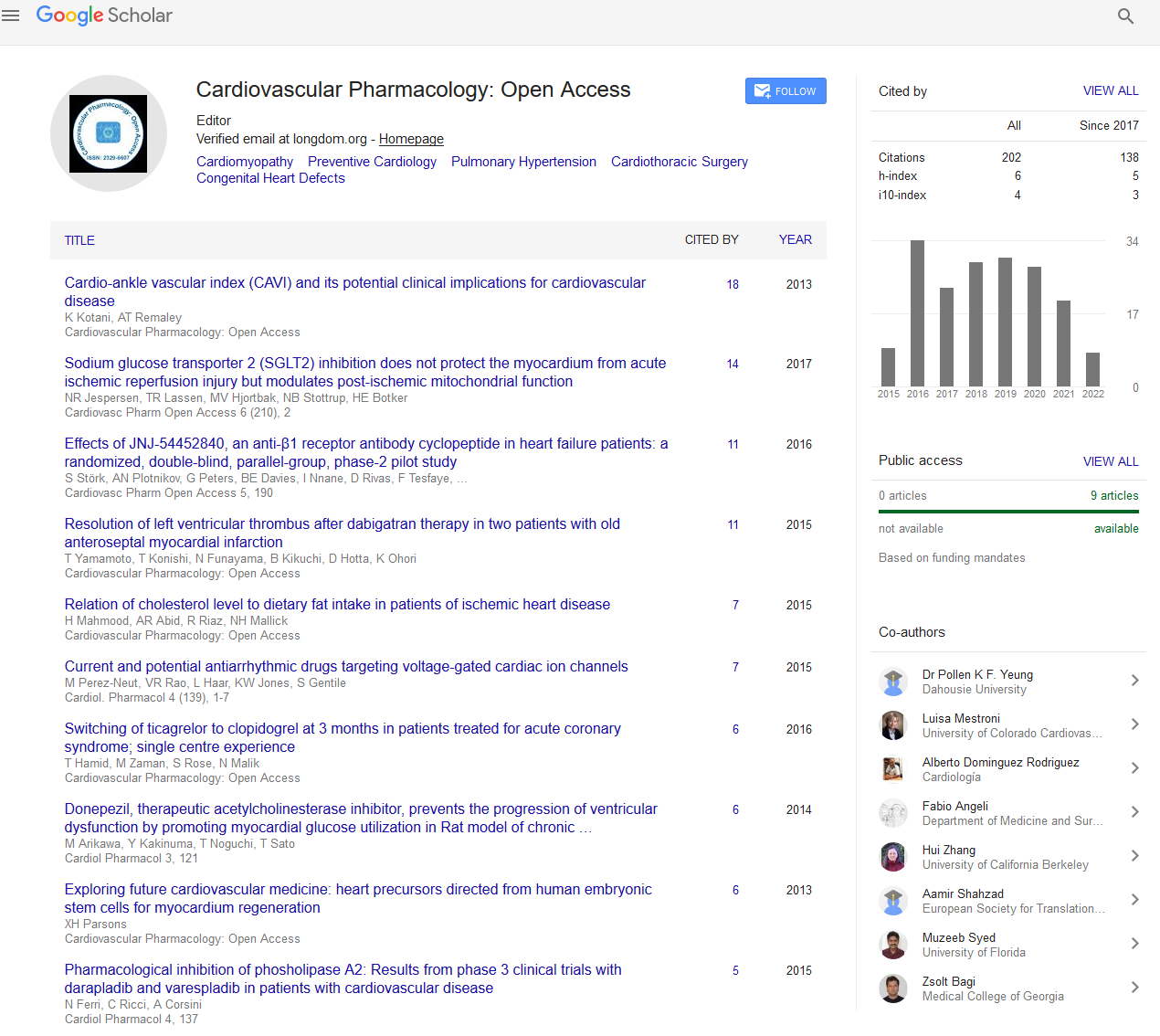
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Commentary - (2022) Volume 11, Issue 5
Recent Advancements in the Cardiovascular Drug Delivery System
Xudong Deng*Received: 05-May-2022, Manuscript No. CPO-22-17035; Editor assigned: 09-May-2022, Pre QC No. CPO-22-17035 (PQ); Reviewed: 23-May-2022, QC No. CPO-22-17035; Revised: 30-May-2022, Manuscript No. CPO-22-17035 (R); Published: 06-Jun-2022, DOI: 10.35248/2329-6607.22.11.286
Description
Cardiovascular disease (also known as heart disease) refers to a group of illnesses that affect the heart and blood vessels (arteries, veins, and capillaries). Angina pectoris is a cardiac disorder characterized by chest discomfort caused by a lack of oxygen to the heart. There are several causes of cardiovascular disease, but the most frequent are atherosclerosis and/or hypertension. Furthermore, as people become older, a variety of physiological and morphological changes affect cardiovascular function, increasing the risk of cardiovascular disease in later years, even in healthy, symptom-free people. Cardiovascular disease is a major cause of mortality globally. In many wealthy nations, cardiovascular death rates have decreased since the 1970s [1].
Heart failure is a prominent cause of morbidity and death globally, despite advances in pharmacological and therapeutic therapy. To treat Heart Failure (HF), several innovative and sophisticated treatment techniques have been investigated, including cell transplantation, gene delivery or therapy, and cytokines or other small chemicals. Recent research into the molecules that govern cardiac activities has revealed that they are critical molecules in the treatment of heart failure. Furthermore, a paracrine mechanism hypothesis, which is related to the positive effects of cell treatment, encourages us to look for new target molecules for pharmacological approach. The term "gene transfer treatment" refers to the transport of genetic elements into cells in order to achieve therapeutic results. Gene therapy for the cardiovascular system has recently made significant progress, and clinical research on numerous novel therapeutic target genes has begun, with some promising findings already attained. Drug delivery vehicles include polymeric micelles, liposomes, dendrimers, lipoprotein-based drug carriers, nanoparticle drug carriers, and others. Biocompatible, non-toxic, non-immunogenic, and biodegradable drug delivery vehicles should evade identification by the host's defensive mechanisms [2].
Liposomes- Liposomes are made up mostly of phospholipids with a few extra molecules thrown in for good measure. Liposomes range in size from a few micrometres to several tens of micrometers. Unilamellar liposomes are smaller liposomes with diverse targeting ligands attached to their surface, allowing for surface attachment and accumulation in diseased regions for disease therapy. Liposomes are non-hemolytic, non-toxic, nonimmunogenic, biocompatible, and biodegradable, and might be tailored to avoid clearance processes including chemical or enzymatic inactivation, renal clearance, and so on. Depending on the nature of the medicine, ligand-coated nanocarriers can store their payload in the hydrophobic shell or the hydrophilic interior section.
Polymeric Nanoparticles- Drug carriers made of biodegradable polymeric nanoconstructs have been studied extensively. Copolymers made up of two or more blocks with differing hydrophobicities fall under this category of nanocarrier. These copolymers commonly form micellar structures in aquatic conditions, with a hydrophilic shell and a hydrophobic core. Water-insoluble pharmaceuticals can be housed inside the hydrophobic core, while the hydrophilic corona can be changed for the attachment of water-soluble medications or targeting moieties. Encapsulated medications are released at a regulated pace that is time or environment dependent. The duration of nanoparticles' residency in the body and the features of their microenvironment influence the release kinetics of nanoparticlebound medicines [3].
Dendrimers- Dendrimers are the tiniest nanocarriers, with numerous end groups that allow for a great degree of link targeting or active agent targeting. They represent polymer chains that branch at regular splitting intervals, allowing for a rapid increase in the number of end groups as molecular mass increases. Dendrimers are generally quite uniform in size, and their molecular weights can exceed 1,000 kD. They prefer a sphere-shaped geometry due to their very branching nature. Dendrimers have a low inherent viscosity and a high surface-tovolume ratio in comparison to linear polymers of the same molecular weight.
Artificially developing particularly designed nanostructure systems for DNA computing is the key to DNA nanotechnology's success. Artificial nucleic acid nanodevices might be utilized to target medicine delivery depending on environmental sensing. These approaches treat DNA as a chemical molecule rather than the biological bearer of genetic DNA information that it is. It has been established that nucleic acid logic circuits may be employed as the heart of a system that helps release the medicine solely in response to a stimulus such as a certain mRNA [4].
Silica nanoparticles can be employed in both passive and active methods to transport drugs to the heart. Galagudza and colleagues developed adenosine-loaded silica nanoparticles for passive adenosine administration to ischemic-reperfused heart tissue. As previously stated, adenosine is a cardioprotective drug, and it was incorporated into the NPs via adsorption on their surface. In vitro and in vivo, the NPs had a mean diameter of 6–13 nm and had no harmful effects. However, because they are captured by the liver, their long-term toxicity is unknown. In rats with ischemic-reperfusion damaged hearts, intravenous injection of adenosine-silica NPs resulted in increased accumulation in the infarcted region. In compared to free adenosine treatment, adenosine bound to NPs restored blood pressure and significantly decreased infarct size. It should be stressed that the DDS should be given shortly after ischemia or at the start of reperfusion to optimize its therapeutic benefits [5].
REFERENCES
- Heidenreich P. Heart failure prevention and team-based interventions. Heart Fail Clin. 2015;11(3):349-58.
[Crossref] [Google Scholar] [PubMed]
- Singh B, Garg T, Goyal AK, Rath G. Recent advancements in the cardiovascular drug carriers. Artif Cells Nanomed Biotechnol. 2016;44(1):216-25.
- Ding BS, Dziubla T, Shuvaev VV, Muro S, Muzykantov VR. Advanced drug delivery systems that target the vascular endothelium. Mol Interv. 2006;6(2):98.
[Crossref] [Google Scholar] [PubMed]
- Timmis A, Townsend N, Gale C, Grobbee R, Maniadakis N, Flather M, et al. European society of cardiology: cardiovascular disease statistics 2017. Eur Heart J. 2018;4(1):1-3.
[Crossref] [Google Scholar] [PubMed]
- Bobo D, Robinson KJ, Islam J, Thurecht KJ, Corrie SR. Nanoparticle-based medicines: a review of FDA-approved materials and clinical trials to date. Pharm Res. 2016;33(10):2373-87.
[Crossref] [Google Scholar] [PubMed]
Citation: Deng X (2022) Recent Advancements in the Cardiovascular Drug Delivery System. Cardiovasc Pharm. 11:286.
Copyright: © 2022 Deng X. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.