Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- Google Scholar
- SHERPA ROMEO
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2021) Volume 9, Issue 1
RAVS Study: A Single Center Experience with Turbo hawk Directional Atherectomy Device to analyze it as an Emerging Modality for Treatment of Long Segment Femoro-Popliteal Occlusive Disease
Chandrashekar Anagavalli Ramswamy, Vivek Vardhan Jayaprakash*, Adharsh Kumar Maruthu Pandian, Sanjay C Desai, Rajendra Prasad Basavanthappa, Ashwini Naveen Gangadharan, Ranjith Kumar Anandasu, Nivedita Mitta and Hemanth Kumar ChoudaryReceived: 30-Dec-2020 Published: 30-Jan-2021, DOI: 10.35248/2329-6925.9.37.405
Abstract
Background: Despite advances to prevent and better manage patients with established Peripheral Arterial Disease (PAD), the incidence of PAD continues to increase and morbidity remains high, especially as the population ages. For physicians treating PAD cases, an understanding of the various treatment options, along with their benefits and limitations is crucial. Endovascular treatment with Turbo hawk atherectomy device has promising technical and clinical success rates.
Objective: To consider Turbo hawk directional atherectomy as an important and safer endovascular modality for treatment of long segment Femoro-popliteal occlusive disease.
Methods: This is a retrospective study which included 40 patients diagnosed with PAD (long segment occlusion of Femoro-popliteal arteries), who came to Ramaiah medical college hospital, Bangalore from June 2014 to June 2018 and fit into specified inclusion criteria with mean age of the patients being 61.5 years. All these patients underwent endovascular therapy with turbo hawk atherectomy device and post intervention was followed for a period of one year.
Results: Primary technical success rate was 97%. Pre-operatively mean ABI was 0.27 and post–operative mean ABI was 0.64. An average length of corrected lesion was 10.5cms. Post-operatively one patient had an episode of distal embolization, two patients had dissection and three had puncture site hematomas, all of which were managed conservatively. No vessel perforation was observed in our study. Patients were followed up at 1 month, 6 months and 12 months postoperatively. Primary vessel patency rates at 6 and 12 -months were 96% and 85%.
Conclusion: Directional atherectomy using turbo hawk device is safe, effective at 12 months for medium and long segment femoro-popliteal lesions in claudicants as well as in patients with critical limb threatening ischemia and has a primary patency rates of 85 % over 1-year period. Further, complication rates that warrants a treatment is also very low with Turbo hawk as seen with our study.
Keywords
Atherectomy; Peripheral arterial diseases; Turbohawk; Femoropopliteal; Endovascular; Directional atherectomy; Outcomes; Experience in single center
Introduction
Incidence of Peripheral Arterial Disease (PAD) in lower extremities is about 50-100 per 100,000 yearly and affects about 20% of the population older than 70 years old [1]. Despite advances in medical therapies to prevent atherosclerosis and better manage patients with established PAD, the incidence continues to increase, and associated morbidity remains high, especially as the population continues to age [1]. Critical limb ischemia (CLI) is the most severe manifestation of peripheral arterial disease (PAD) and present with ischemic rest pain, non-healing ischemic ulcerations, or gangrene. Some relief in symptoms is possible with exercise, pharmacotherapy, and cessation of smoking [2]. The risk of limb-loss is overshadowed by the risk of mortality from coexisting coronary artery and cerebrovascular atherosclerosis [2]. For physicians treating patients with PAD, an understanding of the various treatment options, along with their benefits and limitations is crucial as a greater number of patients with PAD are being encountered [2]. Over the time, surgical bypass option has been the gold standard in long segment femoropopliteal disease, with 5-year limb salvage rates of approximately 80% in patients presenting with a rest pain or non-healing ulcer. However, there has been a progressive shift from bypass surgery to endovascular treatment in recent times, especially with advent of stents, drug-coated balloons, and atherectomy.
Endovascular therapy continues to have significant limitations. Percutaneous Balloon angioplasty with or without stenting of femoro-popliteal lesions is limited by a low primary patency rate of 30% to 61% and it depends on several factors like lesion length, calcifications, bifurcated and diffuse nature of lesions [3]. Even if used, stents must be able to withstand significant biomechanical forces, if not, may lead to stent fractures, in-stent stenosis and occlusion [4]. Atherectomy on other hand offers the ability to de-bulk atherosclerotic plaque with minimal change in vessel diameter and this when done along with supplemental PTA reduces the need for subsequent stent placement [5]. Though older randomized controlled trials with Simpson Atherocath reported high technical success rates, it had similar long-term results when compared to conventional PTA [4]. This, along with the demanding technique, prevented atherectomy to become established as a routine technique. The introduction of the easy- to-use Silverhawk and Turbohawk devices (Medtronic plc, formerly Covidien/ev3, and Plymouth, MN) has reestablished the use of directional atherectomy (DA) with promising acute technical and clinical success rates and mid-term patency rates for the treatment of femoro-popliteal lesions [4]. The primary aim of this study is to consider atherectomy with Turbohawk as an important and safer endovascular modality for treatment of long segment Femoro- popliteal occlusive disease.
Materials and Methods
Patient population
Our study included patients with peripheral arterial disease (PAD), who came to Ramaiah medical college hospital, Bangalore between periods of 4 years from June 2014 to June 2018. It is a retrospective study and included forty patients having long segment occlusion of femoro-popliteal arteries, who underwent directional atherectomy procedure. The mean age of the patients was 61.5 years (range 43 to 80 years), and there were 34 men and 6 women. The mean of pre-procedure ankle-brachial index of patients was 0.27, the length of lesions treated ranged from 7 to 20 cm, with a mean of 10.5 cms. All these patients were also followed up for a period of 1-year post intervention. Data was retrospectively collected from inpatient medical registers and OPD registers that were maintained by vascular surgery department at our hospital. Since it’s a retrospective study, no personal data that could be directly linked to a patient were used in this study and their confidentiality was strictly protected, all throughout the data collection and analysis.
Inclusion criteria
1. Stable chronic PAD patients in Rutherford clinical category 4 – 6 of chronic limb ischemia
2. Lesion Length ≤ 20 cm
3. Reference Vessel ≥ 1.5 mm and ≤ 7.0 mm
Exclusion criteria
1. In-stent restenosis
2. Aneurysmal target vessel
3. Acute occlusion/angiographically visible thrombus
4. Use of Re-entry devices (Figure 1)
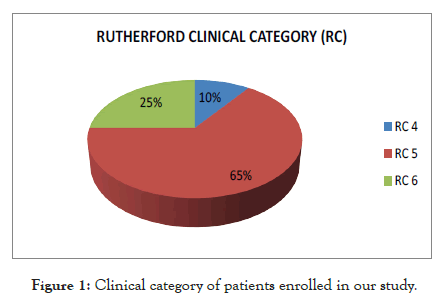
Figure 1: Clinical category of patients enrolled in our study.
Technique and description of procedure
The catheter was introduced through a sheath placed anterograde or in crossover retrograde fashion (for an ostial lesion) in the common femoral artery using modified Seldinger technique to the lesion intended for treatment. Using an external centimeter marker ruler placed before angiography, the catheter was to be positioned in the region of the intended atherectomy. In these patients, 7Fr sheath compatible catheters were used with a central 0.035 guide wire passed across the lesion and wire was exchanged with 0.014 guide wire, which was parked across the lesion. Pre-dilatation with an undersized uncoated angioplasty balloon at low pressure was done to allow successful advancement of the Directional atherectomy (DA) device, where a DA device was unable to cross. The Turbo- Hawk atherectomy device features four angled, Super Cutter blades that are designed to increase the efficiency of directional plaque excision more than its fore-runner Silver hawk and mainly intended for above the knee interventions, including severely calcified lesions in varying vessel diameters .The directional turbo-hawk atherectomy device consist of 2 major components, the peripheral catheter and the cutter driver.
Atherectomy catheter was slowly advanced over the wire while rotating the cutter blade placed first over the posterior wall and then rotating the device in the clock wise direction at 300 completing the removal of the plaque along the lateral and anterior wall of the vessel and flushing the plaque out of the nose cone once it was filled. The number of lesions passes and the use of distal embolic protection devices were left to the discretion of the surgeon. Some set of patients had proximal iliac lesion which were plastied before doing atherectomy to improve the inflow. Some patients who had focal significant residual lesion underwent PTA (Plain balloon angioplasty) / DEB (drug eluting balloon) angioplasty after atherectomy as per the surgeon’s preference. In 6 patients embolic protection devices (EPD’s) were used during the procedure, though there were no specific criteria for EPD’s usage in those cases. Stenting was reserved only for cases with severe flow limiting dissection (as bail out), however it wasn’t performed in any of study cases (Figures 2-4).
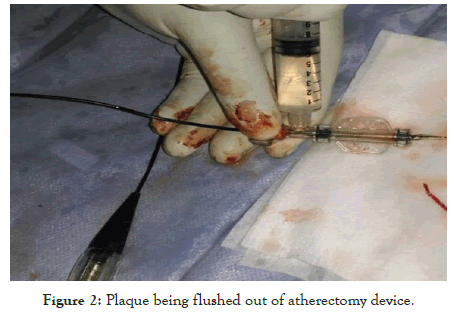
Figure 2: Plaque being flushed out of atherectomy device.
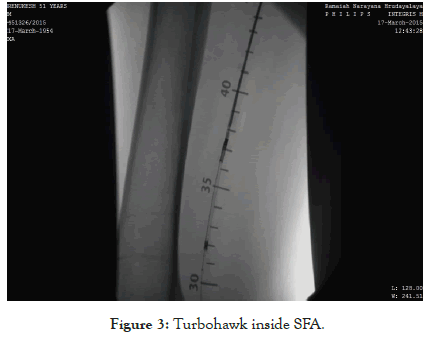
Figure 3: Turbohawk inside SFA.
Figure 4: Guide wire seen in SFA with good flow on check angiogram after atherectomy.
Medical management
Intra-operatively patient received unfractionated heparin according to patient’s body weight. All the interventions in this study were completed within 70 minutes. Activated clotting time (ACT) measurement was not measured routinely in our cases. Postoperatively patient was kept on anticoagulation till hospital stay and then discharged with dual anti-plalets (Aspirin 75 mg/ Clopidogrel 75 mg) for 3 months followed by aspirin (75/150mg) lifelong.
Patient evaluation
All patients included in the study, underwent arterial clinical examination, measurement of ankle-brachial indexes and MR/CT angiographic evaluation pre-operatively. Primary technical success of atherectomy was defined as the excision of calcified plaque in order to create a post-atherectomy residual diameter stenosis of ≤ 50% with an optimal working channel allowing performing safely conventional PTA. Post atherectomy patients were assessed with ABI and duplex ultrasound at various follow-up intervals during 1, 6 and 12-months observation period. Primary patency was defined as freedom of restenosis as confirmed by duplex ultrasound i.e., ≤ 50% diameter stenosis as confirmed by peak systolic velocity index, ratio of intra-stenotic peak systolic velocity to pre stenotic velocity without any re-intervention at the level of the target lesion during the time of follow-up visit. Repeat arteriographic evaluation was conducted in patients who had a significant decrease in ankle- brachial index; decrease in tissue perfusion or recurrence of symptoms same as that seen prior to preliminary intervention.
Results and Data Analysis
This study was conducted with 40 PAD patients fitting into above mentioned inclusion criterions between 2014 to 2018 at Ramaiah medical college and teaching hospital, Bangalore using directional turbo-hawk atherectomy device. This study included 34 males and 6 females belonging to Rutherford class C4 to C6 categories, however predominantly patients were in C5 category. Patients included were in age group between 43 and 80 years, with a mean age of 61.5 years. Important risk factors that were noted in our study include smoking and diabetes mellitus which were seen in more than half of study population. Other risk factors that occurred in lesser frequency were hypertension, coronary artery disease and hyperlipidemia. Atherectomy was done in antegrade fashion for 33 patients and in retrograde fashion for 7 patients, out of which 4 had concomitant iliac in-flow lesion who under- went iliac angioplasty and 3 had ipsilateral SFA ostial lesion. An average procedure time was 56.5 minutes. 16 patients underwent DEB angioplasty that had focal significant residual lesion after atherectomy and in 6 patients embolic protection devices were used during the procedure, though there were no specific criteria for EPD’s usage in those cases (Figures 5 and 6) (Tables 1 and 2).
Figure 5: Distribution of risk factors of patients in our study.
Figure 6: Adjunctive treatment used along with atherectomy.
Figure 7: Mean ABI pre-op and post-op in study patients.
| Procedural characteristics | |
|---|---|
| Antegrade | 34 |
| Retrograde | 6 |
| Procedure time | 66.5 mins |
| Drug eluting balloon | 16 |
| Plain balloon angioplasty | 12 |
| Concomittent proximal (iliac lesion) angioplasty | 4 |
| Mean abi pre op | 0.27 |
| Mean abi post op | 0.64 |
Table 1: Procedural characteristics.
| Target lesion length (cms) | |
|---|---|
| Average length (cms) | 11 |
| Less than 10 | 8 |
| Oct-15 | 32 |
Table 2: Baseline lesion characteristics.
Primary technical success rate was 97% in this study (39/40). Pre-operatively mean ABI was 0.27 and post-operative mean ABI was 0.64. An average length of corrected lesion was 10.5 cms (lesion lengths between 7-20 cms). Post-operatively two patients had an episode of distal embolization and three had puncture site hematomas, all of which were managed conservatively. No arterial dissection or vessel perforation was observed in our study. Patients were followed up at 1 month, 6 months and 12 months postoperatively. Using Kaplan-Meyer analysis, primary vessel patency rates at 6 and 12-months was 96% and 85 % in our study population (Figure 7 and Table 3).
| Periprocedural complication | |
|---|---|
| Distal embolisation | 2 |
| Perforation | 0 |
| Dissection | 0 |
| Puncture site complication | 3 |
Table 3: Complications encountered in our study.
Discussion
We report on the long-term results of patients with long segment femoro-popliteal lesions treated with the Turbohawk directional percutaneous atherectomy catheter system (Medtronics). Though retrospective in nature, this is one of first of its kind single center study reporting outcomes with Turbohawk atherectomy device. During last 10 years, there has been a paradigm shift away from open surgery toward endovascular therapy. Around the world, the rate of endovascular lower extremity interventions has quadrupled for critical limb threatening ischemia and doubled for claudicants [5]. This has been accompanied by a reduction in the rate of major amputations and length of hospital stay, despite an increase in the burden of patient comorbidities. PAD results from any disease-causing stenosis or occlusion of the lower limb arteries with atherosclerotic disease being the most common etiology [6] risk factors for atherosclerosis includes race, male gender, increasing age, smoking, diabetes mellitus, hypertension, dyslipidemia, hypercoagulable states, hyper-homocysteinemia, systemic inflammatory conditions and chronic renal insufficiency. Particular emphasis should be given on smoking cessation and aggressive glycemic control in diabetic patients, since both represent the most dominant risk factors for PAD [7]. Smoking cessation among patients with symptomatic PAD does not improve walking capacity but may reduce the severity of claudication, reduce risk of developing critical limb ischemia and also improves outcomes after a vascular intervention [8-11].In our series it was seen that the all the patients belonged to more than 40 years with mean age being 61.5 years. Risk factors like smoking (28 cases), diabetes mellitus (24 cases), Hypertension (15 cases) were seen predominantly, however no case of renal insufficiency were taken into the study group.
Traditionally, atherosclerotic disease affecting the femoral artery is best treated surgically with a bypass operation or endarterectomy with patch angioplasty [12]. Recently, technological advances favored a significant evolution of percutaneous revascularization therapies which can be offered as treatment options, which are less invasive than traditional surgery. The optimal endovascular therapy is not well established and includes several options like angioplasty, stenting, drug-coated balloons and atherectomy. But, as the femoro popliteal vessel lies over the hip joint in chronically occluded segments, and can involve the region of the adductor canal, there can be issues related to vessel like suboptimal stent placement, stent flexion, elongation or torsion during routine daily activities, stent fractures and restenosis or stent thrombosis. These can be associated with acute limb-threatening ischemia, as circulation to both the superficial femoral artery (SFA) and the profunda femoris can be compromised simultaneously [13,14].
Promise of atherectomy is to overcome the limitations and complications of traditional angioplasty such as dissection, elastic recoil, and disruption of the internal elastic lamina, resulting in overwhelming neo-intimal hyperplasia and smooth muscle cell proliferation [15]. Endovascular stenting in the SFA is generally indicated only in the presence of a flow-limiting dissection or severe elastic recoil after balloon angioplasty [16]. Considering the still unresolved issue of stent fractures after SFA and popliteal artery stenting, any technology that improves the acute technical result of angioplasty avoiding stenting should be beneficial. Atherectomy procedure reduces barotraumas i.e., vessel wall injury from irregular tears, splits, and stretches that are caused by balloon angioplasty which often demands stent placement [17-19].
Atherectomy is performed to debulk the atherosclerotic plaque from diseased vessel. Usually it is combined with low-pressure balloon angioplasty with the aim of minimizing plaque shift while avoiding stent placement. Different atherectomy devices are designed to cut, shave, sand, or vaporize atherosclerotic or calcified plaques and each have slightly different indications depending upon the lesion characteristics [5]. Four different methods of atherectomy have been utilized for treatment of femoropopliteal or small-vessel infra-popliteal disease, which are plaque excision (directional) atherectomy, rotational atherectomy / aspiration, laser athero- ablation, and orbital atherectomy. Directional atherectomy devices make use of carbide rotating cutter disks that resect and remove the atherosclerotic plaque [5].
Earlier version Simpson Athero-Cath, did not become established for treatment of femoropopliteal lesions in the early 1990s because of its complex operation and poorer results compared to balloon angioplasty [20-29]; however, the system presented here (Turbohawk) is simple to operate that could lead to a rebirth of directional atherectomy. Atherectomy alone in the majority of our cases was technically successful, but additional balloon dilation in about 60% of our cases served to visually improve the angiographic appearance of the recanalized artery. From a technical standpoint, this newer catheter could be easily controlled in both antegrade and crossover approaches, despite wire guidance of the monorail system over only a short distance [3]. The SilverHawk and TurboHawk plaque excision systems are the only two U.S. Food and Drug Administration (FDA)-approved directional atherectomy devices that are being used today, with the next version HawkOne system recently being FDA cleared for usage. The Turbo Hawk atherectomy device comes in various sizes to enable atherectomy in vessels ranging from a diameter of 1.5 mm to 7 mm. Our study included patients with femoro-popliteal lesions from a length of 7 up to 20cms with a mean length of 10.5cms [5].
SilverHawk plaque excision atherectomy system is a forward- cutting, directional atherectomy device that consists of a rotating blade inside a tubular housing with a collection area. TurboHawk system is similar to the SilverHawk in other designing except with a different number of inner blades, allowing for a larger luminal gain. While SilverHawk has one inner blade, TurboHawk has four contoured blades which favors use in highly calcified lesions and also achieves more plaque removal per pass [5]. Unlike prior atherectomy devices, Turbohawk catheter enables treatment of a large range of vessel diameters with predictable and consistent cuts which allows capture of voluminous amounts of plaque (up to 750 mg) in a single peripheral specimen [30]. Stents were not used in our atherectomy patients when compared to other studies of laser and cryoplasty procedures, in which stent placement rates were 45% and 8.8%, respectively [31,32].
In the study by Ramaiah et al., stent placement after atherectomy was performed in 6.3% of lesions, and their Target limb Revascularization (TLR) rate ranged between 9% (in nondiabetic patients) and 11% (in diabetic patients) at 12 months [30]. In our study the use of reentry devices was an exclusion criterion and most of the occlusions were crossed intraluminal, potentially resulting in a reduced likelihood of multiple dissection planes, which usually requires bail-out stent placement, potentially explaining the low overall bail-out stent rate in the present study. Biskup et al. also reported no cases of provisional stent placement with atherectomy, which was similar to our study that is supporting historic observations and indicating that atherectomy reduces recoil and dissection. The mechanism of reduced dissection and recoil is unclear, but we think that it may be related to improvement of vessel compliance in the atherectomy by reducing plaque burden [33]. This directional atherectomy procedure significantly decrease the need for stenting facilitating future endovascular or open surgical revascularization in these hostile arterial segments such as flexion points [34].
Yet another intriguing concept is ‘‘lesion preparation’’ and the ‘‘leaving nothing behind’’ approaches , where atherectomy is employed for plaque removal and modification prior to drug-coated balloon (DCB) angioplasty so as to improve the acute luminal gain, remove/remodel the calcium barrier, aids in drug diffusion and decrease the need for stenting [34]. Low-pressure balloon angioplasty can limit vessel wall barotraumas and further limit inflammatory response (neointimal hyperplasia) of the arterial wall. However, this intruiging concept of combined atherectomy (with Turbohawk) and DCB treatment needs to be better determined by well-designed randomized controlled trials (RCT), as solid data demonstrating its superiority over standard endovascular treatment are insufficient at present [35,36]. In our study it was seen that 16 cases had Drug eluting balloon and 12 cases had plain ballon angioplasty concomitantly after atherectomy procedure. Adjunctive PTA significantly reduced stent use compared with PTA alone. In addition, optimal balloon inflation in these cases was achieved at lower pressures than with primary PTA, which may have been related to increased compliance of the pretreated lesion with atherectomy as seen in other such studies [37].
In 2011 February, NICE had published guidelines on percutaneous atherectomy of femoro-popliteal lesions with plaque excision devices, suggesting that even more auditing and research in the form of well-conducted trials should take place because of the inadequate evidence at present on the efficacy and safety of this procedure [38]. The Determination of Effectiveness of Silver-Hawk Peripheral Plaque Excision for the Treatment of Infra-inguinal Vessels or Lower Extremities (DEFINITIVE LE) study is the largest so far to evaluate directional atherectomy, with enrollment of about 800 patients worldwide with both claudication and/or Critical limb ischemia across 50 sites in the U.S. and Europe. The success rate was reported at 89%, with post-atherectomy bail-out stenting rate of 3.2%. Rates of distal embolization, dissection, and perforation in this study were 3.8%, 2.3%, and 5.3% respectively. Primary patency rate at 12 months in claudicants was 78%, whereas the rate of freedom from major unexpected amputation of the target limb at 12 months in CLI group was 95% [5]. Reported median procedure time (time from arterial access to catheter removal) of 65.0 min (45.0 to 92.0 min) using SilverHawk catheter, whereas in our study with turbohawk device the average procedure time was 56.5 minutes [39].
On the other hand, using directional atherectomy (Silverhawk catheter with diameter of 2.7 mm), Authors has reported a primary technical success rate of 92% and primary patency rate of 55% at 3 years follow-up in femoro popliteal lesions. Similar to our experience, Minko Had also reported a low incidence of distal embolization without distal protection device and it was described that silver Hawk allowed avoiding distal embolization of calcified lesions by performing a frequent clearance of the nose cone [40]. Author has reported a 90% patency rate after 1 year in patients with heavily calcified femoropopliteal stenosis (which is defined as fluoroscopic calcification on both sides of vessel wall >1 cm in length) using Turbohawk catheter with DEB and it was seen in their study that the bailout stent rate was 6.5%, the 1-year duplex- derived primary patency rate was 90%, and the freedom from MAEs was 87% [41]. In our study the technical success rate was 97% and perioperatively patients mean ABI improved from 0.27 to 0.64. The primary patencies in our study at end of 6 months and 1 year were 96% and 85% respectively.
The complications with atherectomy procedures includes arterial dissection, arterial perforation, arterial rupture, arterial spasm, arterio-venous (AV) fistula, bleeding complications, embolism and/ or arterial thrombosis, emergency arterial bypass surgery, puncture site complications, restenosis of the atherectomised segment, complete occlusion of the peripheral artery and other vascular complications which may warrant a surgical repair [42]. In our study significant complications noted were distal embolization (2 cases) and puncture site complications (3 cases), however no dissection or perforations were noted. Distal embolization remains a concern with usage of atherectomy devices, given that these devices require retrieval of removed plaque, and the use of distal protection devices may be needed in these patients, particularly with heavily calcified lesions [5]. Usually more than 2 mm is taken as threshold for ‘‘clinical significance’’ of this macro debris, but it is still unclear whether debris of this size has real clinical consequences. The distal tibial vessels are typically 2.0-2.5 mm in diameter, and it is expected that debris >2mm will cause distal tibial vessel compromise, particularly in a diseased runoff vessel or in patients with a single patent tibial vessel [43]. Generally, it can be accepted that in order to minimize the risk of thrombosis, patient has to be anticoagulated adequately during the procedure and adequate measures have to be taken with regard to safety and the use of the device.
Embolic Protection Devices (EPD) has been used successfully in various circumstances and is found to be effective in capturing larger debris. Preventing Lower Extremity Distal Embolization Using Embolic Filter Protection – PROTECT study, included 40 patients with 56 lesions being treated with angioplasty/stenting or atherectomy and 1 filter was employed per patient. Clinically significant macro debris that is given as >2 mm in diameter was found in 27.6% of the angioplasty/stenting patients and 90.9% of the atherectomy patients [43,44]. In Our study EPD’s were not used based upon any specific criteria rather randomly assigned for usage in 6 patients. EPD’s also have their own problems and main amongst them is the device retrieval where problems might be encountered. However, it should be remembered that filter use in the periphery is yet an off-label application, and future research is needed to validate their cost effectiveness, overall clinical benefits and safety [43].
In future, an even more interesting treatment combination would be atheroma debulking by usage of percutaneous atherectomy followed by bioabsorbable drug-eluting stent deployment. Using this approach, all possible advantages of endovascular technological advancements like transcatheter plaque excision, ideal lesion preparation to allow placement of a bioresorbable scaffold, maximal luminal gain without any elastic recoil, prolonged drug delivery for inhibition of neointimal hyperplasia and also no permanent metal implantation will be combined in order to achieve optimal treatment effect for PAD patients. Further technological developments that will minimize the risk of distal embolization, reduce device profile, fasten the procedural time are to be evaluated with large volume randomized controlled trials to establish percutaneous directional atherectomy as the first-line endovascular PAD treatment option with superior patency outcomes [45].
Conclusions
Directional atherectomy using turbo hawk device is safe & effective at 12 months for medium and long segment femoro-popliteal lesions in claudicants & CLI patients, with primary patency rates of 85 % over 1-year period. Further, complication rates that warrants a treatment is also very low with Turbohawk as seen with our study. Also to note is the use of Drug eluting balloons to decrease the chances of restenosis may increase patency in complex atherectomies. Although long term patency is still unknown, turbo hawk atherectomy device has been shown in our study to be an effective device for treatment of long segment femoral popliteal disease and to overcome the limitations of balloon angioplasty and stent placement. A follow-up large randomized control studies are needed to confirm the observations of our study including an increased number of patients, a focus on calcified lesions, and these patients should also be followed up for a longer period of time. Moreover, the outcomes of this study cannot be extrapolated to the impact of other atherectomy or DCB technologies, or in other lesion locations.
REFERENCES
- R Gandini, G Pratesi, S Merolla, Scaggiante J, Chegai F. A single center experience with Phoenix Atherectomy System in patients with moderate-heavily calcified femoro popliteal lesions. Cardiovasc Revasc Med. 2020;21(5):676-681.
- Mahmud E, Cavendish JJ, Salami A. Current treatment of peripheral arterial disease: role of percutaneous interventional therapies. Journal of the American College of Cardiology. 2007;50(6):473-490.
- Zeller T, Rastan A, Schwarzwälder U, Frank U, Bürgelin K, Amantea P, et al. Percutaneous Peripheral Atherectomy of Femoropopliteal Stenoses Using a New-Generation Device: Six-Month Results from a Single-Center Experience. J Endovasc Ther. 2004;11:676-685.
- Zeller T, Rastan A, Sixt S, Schwarzwälder U, Schwarz T, Frank U, et al. Long-Term Results After Directional Atherectomy of Femoro-Popliteal Lesions. J Am Coll Cardiol. 2006;48(8):1573-1578.
- Konstantinos Charitakis, Dmitriy N Feldman. Atherectomy for Lower Extremity Intervention: Why, When, and Which Device? J Am Coll Cardiol. 2015.
- Rothwell PM, Coull AJ, Silver LE, Fairhead JF, Giles MF. Population-based study of event-rate, incidence, case fatality, and mortality for all acute vascular events in all arterial territories (Oxford Vascular Study). Lancet. 2005;366(9499):1773-1783.
- Aboyans V, Criqui MH, Denenberg JO, Knoke JD, Ridker PM, Fronek A. Risk factors for progression of peripheral arterial disease in large and small vessels. Circulation. 2006;113(22):2623-2629.
- Thompson PD, Zimet R, Forbes WP, Zhang P. Meta-analysis of results from eight randomized, placebo-controlled trials on the effect of cilostazol on patients with intermittent claudication. Am J Cardiol. 2002;90:1314-1319.
- Hankey GJ, Norman PE, Eikelboom JW. Medical treatment of peripheral arterial disease. JAMA 2006; 295:547-553.
- The CAPRIE Steering Committee. A randomised, blinded trial of clopidogrel versus aspirin in patients at risk of ischemic events (CAPRIE). Lancet. 1996;348:1329-1339.
- Hackam DG, Tan MK, Lin PJ, Mehta PG, Jaffer S, Kates M, et al. Supporting a call to action for peripheral artery disease: insights from two prospective clinical registries. J Vasc Surg. 2006;44:776-781.
- Nelson P, Powell R, Schermerhorn M, Fillinger MF, Zwolak RM, Walsh DB, et al. Early results of external iliac artery stenting combined with common femoral artery endarterectomy. J Vasc Surg. 2002;35:1107-1113.
- Mahmud E, Keramati S, Salami A, Palakodeti V, Tsimikas S. Expanded applications of rotational atherectomy in contemporary coronary and peripheral interventional practice. J Invasive Cardiol. 2005;17:207-210.
- Silva JA, White CJ, Quintana H, Collins TJ, Jenkins JS, Ramee SR. Percutaneous revascularization of the common femoral artery for limb ischemia. Catheter Cardiovasc Interv. 2004;62:230-233.
- Romano M, Amato B, Markabaoui K, Tamburrini O, Salvatore M. Follow-up of patients with previous vascular interventions: role of multidetector row computed tomographic angiography of the abdominal aorta and lower extremities. J Cardiovasc Surg. 2004;45(1):89-91.
- Cejna M, Thurnher S, Illiasch H, Horvath W, Waldenberger P, Hornik K, et al. PTA versus Palmaz stent placement in femoropopliteal artery obstructions: a multicenter prospective randomized study. J Vasc Interv Radiol. 2001;12: 23-31.
- Schlager O, Dick P, Sabeti S, Amighi J, Mlekusch W, Minar E, et al. Long-segment SFA stenting—the dark sides: in-stent restenosis, clinical deterioration, and stent fractures. J Endovasc Therapy. 2005;12:676-684.
- Scheinert D, Scheinert S, Sax J, Piorkowski C, Bräunlich S, Ulrich M, et al. Prevalence and clinical impact of stent fractures after femoropopliteal stenting. J Am College Cardiology 2005;45:312-315.
- Allie DE, Hebert CJ, Walker GCM. Nitinol stent fractures in the SFA. Endovasc Today. 2004;3:22-34.
- Graor RA, Whitlow PL. Transluminal atherectomy for occlusive peripheral vascular disease. J Am Coll Cardiol. 1990;15:1551-1558.
- Ahn SS, Concepcion B. Current status of atherectomy for peripheral arterial occlusive disease. World J Surg. 1996;20:635-643.
- Ahn SS. Status of peripheral atherectomy. Surg Clin North Am. 1992;72:869-878.
- Vroegindeweij D, Kemper FJ, Tielbeek AV, Buth J, Landman G. Recurrence of stenoses following balloon angioplasty and Simpson atherectomy of the femoro-popliteal segment. A randomised comparative 1-year follow-up study using colour flow duplex. Eur J Vasc Surg. 1992;6:164-171.
- Walker J, Chalmers N, Gillespie IN. A new use of the Simpson percutaneous atherectomy catheter: resection of retained valve cusps of an in-situ vein graft. Cardiovasc Intervent Radiol. 1995;18:50-52.
- Seth A, Mathur A, Chandra P. Revascularization of a thrombosed, previously stented aorto-renal graft using combined directional atherectomy and AngioJet thrombectomy. Catheter Cardiovasc Interv. 1999;46:85-88.
- Castaneda F, Moradian G, Hunter D. Percutaneous intravascular biopsy using a Simpson atherectomy catheter: technical note. Cardiovasc Intervent Radiol. 1990;12:342-343.
- Kumakura H, Yokoi Y, Kusaba H, Koga N, Higashiue S, Ichikawa S, et al. Atherectomy in patients with arteriosclerosis obliterans: angiographic follow-up study of 186 lesions in 146 patients. Nippon Igaku Hoshasen Gakkai Zasshi. 1996;56:638-643.
- Kuffer G, Hansen R, Spengel FA. Simpson’s atherectomy in embolizing leg artery stenoses. Rofo. 1991;155:235-241.
- Lugmayr H, Deutsch M, Pachinger O. Simpson atherectomy-long-term results and indications. Vasa Suppl. 1991;33:44-46.
- Ramaiah V, Gammon R, Kiesz S, Cardenas J, Runyon JP, Fail P, et al. Midterm Outcomes from the TALON Registry: Treating Peripherals with Silver Hawk: Outcomes Collection. J Endo Vasc Therapy. 2006;13:592-602.
- Laird JR, Zeller T, Gray BH, Scheinert D, Vranic M, Reiser C, et al. Limb salvage following laser-assisted angioplasty for critical limb ischemia: results of the LACI multicenter trial. J Endovasc Ther. 2006; 13:1-11.
- Laird J, Jaff MR, Biamino G, McNamara T, Scheinert D, Zetterlund P, et al. Cryoplasty for the treatment of femoropopliteal arterial disease: results of a prospective, multicenter registry. J Vasc Interv Radiol. 2005;16:1067-1073.
- Biskup NI, Ihnat DM, Leon LR, Gruessner AC, Mills JL. Infrainguinal atherectomy: a retrospective review of a single-center experience. Ann Vasc Surg. 2008;22:776-782.
- Katsanos K, Spiliopoulos S, Karnabatidis D, Reppas L. Debulking Atherectomy in the Peripheral Arteries: Is There a Role and what is the Evidence? Cardiovasc Intervent Radiol. 2017;40:964-977.
- Shammas NW. An overview of optimal endovascular strategy in treating the femoropopliteal artery: mechanical, biological, and procedural factors. Int J Angiol. 2013;22(1):1-8.
- Mittleider D, Russell E. Peripheral atherectomy: applications and techniques. Tech Vasc Interv Radiol. 2016;19(2):123-135.
- Shammas NW, Coiner D, Shammas GA, Dippel EJ, Christensen L. Percutaneous Lower-extremity Arterial Interventions with Primary Balloon Angioplasty Versus Silver Hawk Atherectomy and Adjunctive Balloon Angioplasty: Randomized Trial. J Vasc Interv Radiol. 2011;22:1223-1228.
- P Abdulhannan, DA Russell, S Homer-Vanniasinkam. Peripheral arterial disease: a literature review. Br Med Bull. 2012;104(1):21-39.
- Zeller T, Sixt S, Schwarzwälder U. Two-year results after directional atherectomy of infrapopliteal arteries with the SilverHawk device. J Endovasc Ther 2007;14:232-240.
- Gandini R, Merolla S, Chegai F. Foot embolization during limb salvage procedures in critical limb ischemia patients successfully managed with mechanical thromboaspiration: a technical note. J Endovasc Ther. 2015;22:558-563.
- Shammas NW, Lam R, Mustapha J. Comparison of orbital atherectomy plus balloon angioplasty vs. balloon angioplasty alone in patients with critical limb ischemia: results of the CALCIUM 360 randomized pilot trial. J Endovas Ther. 2012;19:480-488.
- Franzone A, Ferrone M, Carotenuto G. The role of atherectomy in the treatment of lower extremity peripheral artery disease. BMC Surgery. 2012;12:S13.
- Shammas NW, Dippel EJ, Coiner D, Shammas GA, Jerin M. Preventing Lower Extremity Distal Embolization Using Embolic Filter Protection: Results of the PROTECT Registry. J Endovasc Ther. 2008;15:270-276.
- Wholey M. The role of embolic protection in peripheral arterial atherectomy. Tech Vasc Interv Radiol. 2011;14(2):65-74.
- Katsanos K, Spiliopoulos S, Karnabatidis D, Reppas L. Debulking Atherectomy in the Peripheral Arteries: Is There a Role and what is the Evidence? Cardiovasc Intervent Radiol. 2017;40:964-977.
Citation: Vardhan VJP, Ramswamy CA, Pandian AKM, Desai SC, Basavanthappa RP, Gangadharan AN, et al. (2021) Ravs Study: A Single Center Experience with Turbo hawk Directional Atherectomy Device to Analyze it as an Emerging Modality for Treatment of Long Segment Femoro-Popliteal Occlusive Disease. J Vasc Med Surg. 9:405.
Copyright: © 2021 Vivek Vardhan JP, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

