Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Euro Pub
- Google Scholar
- Quality Open Access Market
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2023) Volume 9, Issue 2
Rare Post Streptococcal Glomerulonephritis Presentations include Back Pain and Constipation
Paniz Pourpashang1, Fatemeh Nili2, Masoumeh Mohkam3 and Arefeh Zahmatkesh4*2Department of Pathology, Imam Khomeini Hospital Complex, Tehran University of Medical Sciences, Tehran, Iran
Department of Pathology, Imam Khomeini Hospital Complex, Tehran University of Medical Sciences, Tehran, Iran
3Department of Pediatric Nephrology, Research Institute for Children’s Health, Shahid Beheshti University of Medical Sciences, Tehran, Iran
4Department of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Received: 24-Feb-2023, Manuscript No. JPMME-23-20005; Editor assigned: 27-Feb-2023, Pre QC No. JPMME-23-20005 (PQ); Reviewed: 13-Mar-2023, QC No. JPMME-23-20005; Revised: 20-Mar-2023, Manuscript No. JPMME-23-20005 (R); Published: 20-Mar-2023, DOI: 10.35248/2684-1320.23.9.200
Abstract
Background: Post-Streptococcal Glomerulonephritis (PSGN) is a common disease that occurs after pharyngitis or dermatitis involvement with streptococcus. The disease complications are vary including rare neurological disorder like, Posterior Reversible Encephalopathy Syndrome (PRES). Although the disease has some common symptoms like hypertension, oliguria or anuria, and neurological defects, there have been no reports of a child having severe back pain or constipation up until this point.
Cases presentation: Here, we represent a child with severe back pain and constipation that was diagnosed as PRES syndrome followed PSGN.
Conclusion: Despite several studies on PSGN, attention to different and rare associated symptoms could help practitioners with accurate diagnoses. In addition, made us investigate the disease entity.
Keywords
Post-streptococcal glomerulonephritis; Back-pain; Constipation; Posterior reversible encephalopathy syndrome.
Introduction
The most common cause of acute glomerulonephritis in children is Post-Streptococcal Glomerulonephritis (PSGN), which typically affects children between the ages of 3 and 12 years and is uncommon in children under the age of 3. Hematuria, oliguria, edema, and hypertension are the most typical symptoms of PSGN [1,2]. The severity of PSGN can vary, and patients may present with subclinical symptoms or require dialysis, and the majority of cases follow pharyngitis caused by streptococci infections [3,4]. One of the uncommon side effects of PSGN is Posterior Reversible Encephalopathy Syndrome (PRES), which typically manifests as headache, vision loss, and seizures. The etiology and clinical manifestation of PRES in children differ from those in adults, but renal diseases predominated in a large systematic review [5]. There are many different PSGN manifestations, but back pain and constipation have not yet received much attention, despite the PRES syndrome diagnosis. In this study, we described a 10-yearold boy who complained of back pain and constipation and was ultimately diagnosed with PSGN and PRES syndrome together.
Case Presentation
A 10-year-old boy was referred to our clinic complaining of severe constipation, oliguria, and edema. He had previously undergone evaluations and had a raised serum creatinine level. He also had a history of visiting a crowded area and later experiencing fever and other flu-like symptoms. The symptoms were treated with conservative treatment. In his past medical history, he had been completely healthy, had no medical or familial disorders, and had completed his series of vaccinations.
He was referred to our clinic with peri-orbital edema, congestion during a chest exam, hypertension, and anuria. His parents also reported that he had normal urination in the previous two days before a sudden onset of low-volume urination. He was given Lasix with normal saline, but he did not respond to this treatment, and laboratory tests revealed elevated creatinine levels (Table 1). Large kidneys were seen during an abdominal ultrasound study, and as a result of his high creatinine level, anuria, and lack of response to Lasix therapy, the patient underwent sessions of emergent dialysis.
| Test | Result (first and follow-ups) | Test | Result (first and follow-ups) | Test | Result (first and follow-ups) |
|---|---|---|---|---|---|
| BUN (mg/dL) | 63-72-23-7.9 | U/A | C3 (75-135) | 35 | |
| Cr (mg/dL) | 4.6-5.7-0.95-0.79 | SG | 1026-1025 | C4 (9-36) | 17 |
| Calcium(mg/dL) | 8.7-8.4 | PH | 5-May | CH50 (51-150) | 89 |
| Phosphorus(mg/dL) | 6.8-8.9-4.6 | WBC(mg/dL) | Many-5 | ||
| Sodium (mEq/L) | 136-140 | RBC(mg/dL) | Many-25 | P-ANCA | Normal |
| Potassium(mEq/L) | 4.7-4 | Blood | positive | C-ANCA | Normal |
| Uric acid (mg/dL) | 12-5.7 | U/C | negative | Anti-ds-DNA | Normal |
| ASO titre (normal<200) | 800 | ||||
| Abbreviations: BUN: Blood Urea Nitrogen; Cr: Creatinin; WBC: White Blood Count; RBC: Red Blood Count; U/A: Urine Analysis; U/C: Urine Culture; ASO: Antistreptolysin | |||||
Table 1: Laboratory findings.
On the second day of hospitalization, the patient started experiencing severe low back pain, which persisted throughout dialysis. Considering the laboratory results and the requirement for daily dialysis, a kidney biopsy was performed with the intention of confirming PSGN; however, the biopsy report revealed PSGN without crescentic features (Figure 1). On the third day of his hospital stay, the patient experienced a seizure that was controlled with phenytoin and carbamazepine. As a result, Magnetic Resonance Imaging (MRI) without contrast was carried out, and the results revealed PRES, He also received rasburicase for hyperuricemia, adjusted doses of ciprofloxacin, meropenem, and cefazoline, as well as five doses of methyl prednisolone for the treatment of PSGN (Figure 2). Following the methylprednisolone prescription, the patient's symptoms improved noticeably, and PSGN therapy was used to treat the patient's back pain and constipation.
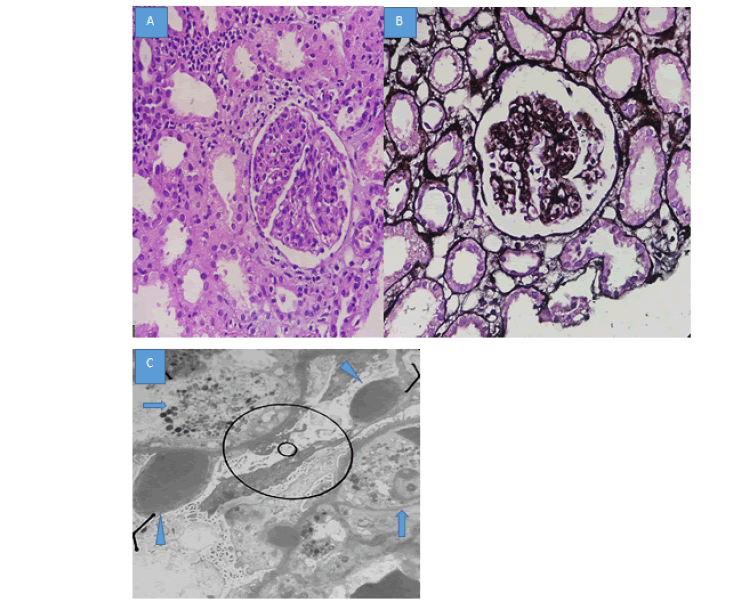
Figure 1: A) Hematoxylin and Eosin sections show dense infiltration of polymorph nuclear leukocytes within the glomeruli. B) Jone’s stain shows mesangial matrix expansion and normal thickness of GBM (400X). C) Electron microscopy study reveals numerous sub epithelial humps (arrows) and intra capillary PMNs (arrowheads).
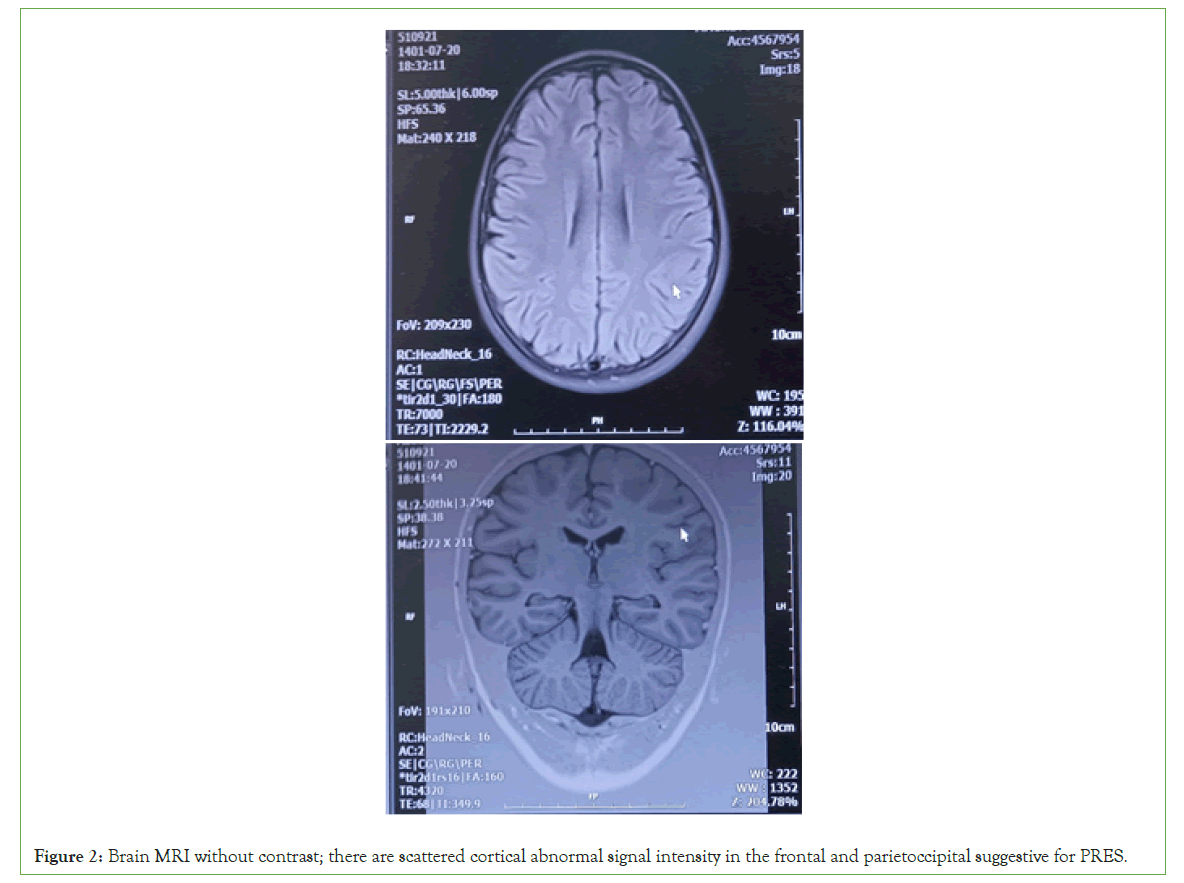
Figure 2: Brain MRI without contrast; there are scattered cortical abnormal signal intensity in the frontal and parietoccipital suggestive for PRES.
The patient was given a clean bill of health and was referred for follow-up exams. At the most recent checkup, his kidney size and creatinine level were both within normal ranges.
Results and Discussion
These Post-Streptococcal Glomerulonephritis (PSGN) is known as rapid deterioration of kidney functions because of an inflammatory process that included type III hypersensitivity reaction after streptococcal infection. This condition is primarily caused by a beta-hemolytic streptococcus known as nephrogenic streptococci, which affect the glomeruli of the kidneys and small blood vessels. PSGN typically appears in children 1-2 weeks after a sore throat [4,6]. In our case, a 10-year-old boy had edema, hypertension, and other typical PSGN presentations after experiencing flu-like symptom. The most frequent side effect of PSGN is hypertension, which has a presentation rate of about 64%. After receiving full treatment, hypertension may recur in 3% to 6% of PSGN patients [7,8]. Children with PSGN involvement may exhibit abnormal neurological symptoms like generalized seizures because of severe hypertension, which affects about 30 to 35 percent of children with PSGN [4,9]. Additionally, hypertension can result from PRES, a term for hypertensive encephalopathy that was first used in 1996 and PRES causes seizures in patients [10]. One widely accepted PRES mechanism theory links the rise in blood pressure to a hypertensive emergency that causes a breakdown in cerebral autoregulation [11]. despite the fact that the child in our case had one seizure, which was stopped by carbamazepine, it is crucial for pediatricians to be aware of the seizure occurrence in kids with PSGN because it can negatively affect neurological function. In general, PRES with PSGN usually has a favorable prognosis.
According to prior studies, clinical findings fully resolve if it is quickly diagnosed and treated [5].
Although reports on the association between back pain and PSGN on children are limited, some studies reported back pain presentation with different glomerulonephritis diagnosis in adult after infections. Study by Kadapia, et al. reported back pain in a 39-year-old man with post infectious glomerulonephritis, who well responded to corticosteroid therapy [12]. Another study showed Minimal Change Nephrotic Syndrome (MCNS) after B type influenza in a 50-years-man with progressive back pain, which spontaneous remission accrued without corticosteroid therapy [13]. However, in our study back pain resolved after corticosteroid administrations, because of less information, more case reports and studies need to investigate the treatment. In addition, no study was reported constipation in PSGN. Although constipation is highly frequent among patients with chronic kidney disease and uremic toxin could affect intestinal motility, there is no reported on constipation in PSGN [14]. Therefor more studies needed.
The predictors of poor long-term prognosis of PSGN include the presence of nephrotic syndrome, crescent formation on biopsy findings, and renal insufficiency at onset [15]. Wong, et al. evaluated 27 PSGN patients who required renal biopsies due to acute severe glomerulonephritis, anuric renal failure, and nephrotic nephritic syndrome. They found that 12 patients required acute dialysis and that 11 patients had crescents that were higher than 50% on the biopsies, and that patients with crescentic glomerulonephritis had a greater need for acute dialysis [3]. Kidney damage may persist years after PSGN because of secondary inflammation after infection due to the nephron’s damages [16]. However, our patient was anuric, after daily dialysis, pathology specimen didn’t reported cresentric and his symptoms start regretting.
In most cases, PSGN is a self-limiting condition, so supportive treatment for managing the effects of overload like edema and hypertension should be carried out. Only symptomatic treatment is advised [15]. Antihypertensive medications in cases with uncontrolled blood pressure, the use of calcium channel blockers, Angiotensin-Converting Enzyme Inhibitors (ACEI), Angiotensin Receptor Blockers (ARBs) are recommended. There is no evidence to support the use of immunosuppressive medications in PSGN patients, but they may be helpful in those with progressive renal failure [17]. Immunosuppressive and antihypertensive medications were used to control the disease in our patient, and with these medications, all patient manifestations were resolved. In fact, after receiving methylprednisolone, all patient manifestations regressed.
Conclusion
In conclusion, PSGN is a self-limiting disease that can manifest as hypertension, neurological disorders. However, we can explain these manifestations due to PRES, back pain and constipation were not previously reported in studies with this syndrome. Pediatricians and physicians should be aware of these manifestations in PSGN. If there is any doubt about PSGN and the patient exhibits either of these symptoms, PSGN treatment should be initiated. If the constipation or back pain persists, doctors should be evaluated.
Authors Contributions
Conceptualization: PP; Validation: MM and FN; Investigation: PP; Resource: PP; Data correction: MM and FN; Writing original draft preparation: PP; Writing review and editing: AZ; Visualization: PP and MM; Supervision: MM and Project administration: AZ
Ethics Approval and Consent to Participate
Informed consent was obtained from the patient and parents of the patient prior to being included in the study.
Consent for Publication
Written consent for publication was taken from the patient and her parents.
Availability of Data and Materials
Not applicable.
Competing Interests
The authors declare that they have no conflict of interest.
Funding
The authors received no specific funding for this research.
Acknowledgements
We thank the patient and her family for their contribution to this study.
References
- Kari JA, Bamagai A, Jalalah SM. Severe acute post-streptococcal glomerulonephritis in an infant. Saudi J Kidney Dis Transpl. 2013;24(3):546-548.
[Crossref] [Google Scholar] [Pub Med]
- Demircioglu Kılıc B, Akbalık Kara M, Buyukcelik M, Balat A. Pediatric post‐streptococcal glomerulonephritis: Clinical and laboratory data. Pediatr Int. 2018;60(7):645-650.
[Crossref] [Google Scholar] [Pub Med]
- Wong W, Morris MC, Zwi J. Outcome of severe acute post-streptococcal glomerulonephritis in New Zealand children. Pediatr Nephrol. 2009;24:1021-1026.
[Crossref] [Google Scholar] [Pub Med]
- Eison TM, Ault BH, Jones DP, Chesney RW, Wyatt RJ. Post-streptococcal acute glomerulonephritis in children: Clinical features and pathogenesis. Pediatr Nephrol. 2011;26:165-180.
[Crossref] [Google Scholar] [Pub Med]
- Shi Y, Ren S, Shu L, Li Q. Posterior reversible encephalopathy syndrome secondary to acute post-streptococcal glomerulonephritis in a child: A case report from the Tibetan plateau. BMC Neurol. 2022;22(1):1-7.
[Crossref] [Google Scholar] [Pub Med]
- Rawla P, Padala SA, Ludhwani D. Poststreptococcal Glomerulonephritis. 2019.
- Ong LT. Management and outcomes of acute post-streptococcal glomerulonephritis in children. World J Nephro. 2022;11(5):139-145.
[Crossref] [Google Scholar] [Pub Med]
- White AV, Hoy WE, McCredie DA. Childhood post‐streptococcal glomerulonephritis as a risk factor for chronic renal disease in later life. Med J Aust. 2001;174(10):492-496.
[Crossref] [Google Scholar] [Pub Med]
- Wong W, Lennon DR, Crone S, Neutze JM, Reed PW. Prospective population-based study on the burden of disease from post-streptococcal glomerulonephritis of hospitalized children in New Zealand: Epidemiology, clinical features and complications. J Paediatr Child Health. 2013;49(10):850-855.
[Crossref] [Google Scholar] [Pub Med]
- Hinchey J, Chaves C, Appignani B, Breen J, Pao L, Wang A, et al. A reversible posterior leukoencephalopathy syndrome. N Engl J Med. 1996;334(8):494-500.
[Crossref] [Google Scholar] [Pub Med]
- Mandal D, Khanal D, Phuyal R, Bhatta A. Posterior reversible encephalopathy syndrome in a patient with post streptococcal glomerulonephritis: A case report. JNMA J Nepal Med Assoc. 2020;58(232):1072-1074.
[Crossref] [Google Scholar] [Pub Med]
- Kapadia AS, Panda M, Fogo AB. Postinfectious glomerulonephritis: Is there a role for steroids? Indian J Nephrol. 2011;21(2):116-119.
[Crossref] [Google Scholar] [Pub Med]
- Haruki A, Ishikawa E, Katayama K, Ito T, Hiramoto T, Fujimoto M, et al. Spontaneous remission of adult-onset minimal change nephrotic syndrome associated with influenza B infection: A case report. BMC Nephrol. 2018;19(1):1-5.
[Crossref] [Google Scholar] [Pub Med]
- Ikee R, Yano K, Tsuru T. Constipation in chronic kidney disease: It is time to reconsider. Ren Replace Ther. 2019;5(1):1.
- van de Voorde 3rd RG. Acute poststreptococcal glomerulonephritis: The most common acute glomerulonephritis. Pediatr Rev. 2015;36(1):3-12.
[Crossref] [Google Scholar] [Pub Med]
- Pinto SW, Mastroianni-Kirsztajn G, Sesso R. Ten-year follow-up of patients with epidemic post infectious glomerulonephritis. PLoS One. 2015;10(5):e0125313.
[Crossref] [Google Scholar] [Pub Med]
- Yang TJ, Shah H, Olagunju A, Novak M, Difilippo W. Role of steroids in post-streptococcal glomerulonephritis without crescents on renal biopsy. Cureus. 2018;10(8):e3150.
[Crossref] [Google Scholar] [Pub Med]
Citation: Pourpashang P, Nili F, Mohkam M, Zahmatkesh A (2023) Rare Post streptococcal Glomerulonephritis Presentations include Back Pain and Constipation. J Pain Manage Med. 9:200.
Copyright: © 2023 Pourpashang P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

