Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Publons
- International committee of medical journals editors (ICMJE)
- Geneva Foundation for Medical Education and Research
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2023) Volume 26, Issue 10
Psychopathology Analysis of 23 Cases with COVID-19 Pneumonia Accompanied by Abnormal Brain Imagine
Weidong Jin1, Xinsheng Chen2, Hongwei Ren3, Jianning Liu4 and Wang Sun1,5*2Department of Internal Medicine, Wuhan University of Science and Technology, Wuhan, China
3Department of Radiology, Wuhan University of Science and Technology, Wuhan, China
4Department of Public Health, Zhejiang Chinese Medical University, Hangzhou, China
5Department of Psychiatry, Zhejiang Chinese Medical University, Hangzhou, China
Received: 04-Sep-2023, Manuscript No. JOP-23-22862; Editor assigned: 07-Sep-2023, Pre QC No. JOP-23-22862(PQ); Reviewed: 21-Sep-2023, QC No. JOP-23-22862; Revised: 28-Sep-2023, Manuscript No. JOP-23-22862(R); Published: 05-Oct-2023, DOI: 10.35248/2378-5756.23.26.643
Abstract
COVID-19 broke out in Wuhan, China in late 2019. The persons involved maybe influenced in psychology. Abnormality of Central Never System (CNS) may promote appeared more psychological symptoms in patients with COVID-19 pneumonia. All the cases were from the hospital where the author was located and diagnosed COVID-19 pneumonia with abnormality of cranial CT (Computerized Tomography) examination and consultation of contact psychiatry. All 23 patients performance mental symptoms of consciousness disturbance, cognitive impairment, anxiety and depression, sleep disorder. The more and serious mental symptoms correlated with dangerous and severe or severe type of COVID-19 pneumonia, more physical disease. COVID-19 pneumonia patients with cranial CT abnormality always had more mental symptoms, especially with delirium and emotional disturbance.
Keywords
COVID-19; Brain CT; Psychopathology; Pneumonia
Introduction
The novel coronavirus pneumonia (Coronavirus Disease 2019- COVID-19) broke out in Wuhan, China in late 2019. Its propagation speed and severity have a significant impact on human beings.
COVID-19 is an emerging respiratory infectious disease caused by the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), which was first detected in early December 2019 in Wuhan, China. As of April 6, 2020, COVID-19 had quickly spread to the majority of countries worldwide, affected more than 1.1 million individuals, and caused nearly 63,000 deaths. Although studies have described the clinical characteristics of patients with COVID-19 [1,2]. At same times, this kind of influence will also cause a kind of serious stress and cause a variety of psychological problems [3,4]. In most cases, there are various manifestations, such as anxiety, depression, compulsion, somatization, etc., and more and more common is sleep disorder [3-6]. The reason of these psychological problems during COVID-19 was both stress and some biological reasons. Because a certain number of new crown pneumonia patients have nervous system symptoms, including three main aspects of nervous system symptoms [7,8]. Obviously, these neurological symptoms promote the appearance of psychological symptoms to some extent. The pathological mechanism of neurological symptoms may be from the CNS invasion of SARS-CoV-2, similar to SARS and MERS (Middle East Respiratory Syndrome) viruses. As with other respiratory viruses, SARS-COV-2 may enter the CNS through the hematogenous or retrograde neuronal route [7]. And the patients with novel coronavirus pneumonia were more likely to develop mental symptoms when neurological symptoms appear. It is an important neurobiological basis when the nervous system, especially the central nervous system, has organic symptoms [8]. We report mental symptoms of 23 patients with novel coronavirus pneumonia and brain CT (Computerized Tomography) abnormality and analyze their, explore the relationship between the brain imaging characteristics and mental symptoms. The aim of this study is to find the impacts of abnormality of brain imagine on the psychopathology.
Materials and Methods
All the cases were inpatients from the hospital where the authors were located. They were Tianyou Hospital Affiliated to Wuhan University of Science and Technology and Tongde Hospital Affiliated to Zhejiang University of traditional Chinese medicine from 1, Jan 2020 to 31, Mar 2020. All patients were certainly diagnosed novel coronavirus pneumonia by positive nucleic acid test of COVID-19 and chest CT with pneumonia, and they were all asked for psychiatric consultation because of mental problems and they also had been completed the cranial CT examination, which show abnormality. 22 patients are from Tianyou hospital and 1 patient is from Tongde hospital. The male patients was 14 cases, female was 9 cases, the age was 51 years-87 years old. COVID-19 pneumonia is classified as dangerous and severe, severe, mild, and common type. The other physical diseases also had been diagnosed by physicians. All patients had positive results of CT. See Table 1 for all patient information. This clinical study was approved by ethic committee of two hospitals.
| No | Sex | Age | Type Of COVID-19 | Brain CT | Other physical diagnosis | Mental symptoms or diagnosis |
|---|---|---|---|---|---|---|
| 1 | F | 84 | severe | 1. Bilateral basal ganglia and right radial coronal lacunar infarction, part of the softening focus, 2. Leukoencephalopathy; brain atrophy, 3. Bilateral internal carotid atherosclerosis. | 1. Type 2 diabetes mellitus; 2. Anemia; 3. Electrolyte metabolism disorder; 4. Hyperuricemia; 5. Internal carotid atherosclerosis; 6. Lacunar cerebral infarction; 7. Aortic atherosclerosis; 8. Coronary atherosclerosis; 9. Pleural effusion; 10. Pleural thickening and adhesion | 1.Dementia, 2.uncoordinated disorderly excitement |
| 2 | M | 82 | severe | 1. Lacunar infarction in bilateral basal ganglia. 2. Brain atrophy, leukoencephalopathy. | 1. Parkinson's syndrome; 2. Sequelae of cerebral infarction; 3. Mild anemia; 4. Abnormal liver function; 5. Electrolyte disorder (low sodium, low chloride, low calcium); 6. Hypoproteinemia; 7. Prostatic hyperplasia | 1.Dementia, 2.disturbance of consciousness |
| 3 | M | 87 | Dangerous and severe | 1. Lacunar infarctions and ischemic foci in pontine, bilateral basal ganglia, corona radiata and central semiovale were observed. 2. Brain atrophy, leukoencephalopathy. 3. Bilateral vertebral artery and internal carotid artery calcification. | 1. Hypertension grade 2 (extremely high risk); 2. Diabetes mellitus; 3. Alzheimer's disease; 4. Left foot soft tissue infection | 1.Alzheimer's disease, 2.disturbance of consciousness, 3.anxiety, 4.sleep disorder |
| 4 | M | 76 | severe | 1. Cerebral infarction in bilateral frontal lobe, right occipital lobe, left pons and thalamus may occur. 2. Lacunar infarction in bilateral basal ganglia. 3. Brain atrophy. | 1. Acute cerebral infarction; 2. Coronary atherosclerotic heart disease; 3. Pacemaker implantation status; 4. Pericardial effusion; 5. Pleural effusion; 6. Abnormal liver function | 1.disturbance of consciousness, 2.anxiety, 3.sleep disorde, |
| 5 | M | 79 | Dangerous and severe | 1. Lacunar infarction in bilateral basal ganglia. 2. Brain atrophy. 3. Bilateral internal carotid atherosclerosis. | 1. Type 2 diabetes; 2. Hypokalemia, 3.Alzheimer's disease; | 1. Dementia, 2.disturbance of consciousness, 3.anxiety. 4.Psychomotor excitement |
| 6 | M | 56 | severe | 1. Lacunar infarction in right basal ganglia. 2. Brain atrophy. | 1. Sudden deafness; 2. Abnormal liver function; 3. Hypertension; 4. Type 2 diabetes mellitus; 5. Vertigo; 6. Cerebral atrophy; 7. Lacunar infarction in the right basal ganglia | 1.Anxiety, 2.sleep disorders |
| 7 | M | 82 | severe | 1. Lacunar infarction in bilateral basal ganglia. 2. Brain atrophy, 3.leukoencephalopathy | 1. Parkinson's syndrome; 2. Sequelae of cerebral infarction; 3. Mild anemia; 4. Abnormal liver function; 5. Electrolyte disorder (low sodium, low chloride, low calcium); 6. Hypoproteinemia; 7. Prostatic hyperplasia.8.Vascular demantia. | 1.Dementia, 2.depression, 3.sleep disorders |
| 8 | M | 69 | mild | 1. Hyperlipidemia; 2. Acute attack of chronic gastritis; 3. Hypertension | 1.Anxiety, 2.depression, 3.sleep disorders | |
| 9 | F | 70 | mild | 1. Lacunar infarctions and ischemic foci in bilateral basal ganglia and around lateral ventricles. 2. Brain atrophy. 3. Calcification of the right vertebral artery and bilateral internal carotid artery. 4. Bilateral ethmoid sinus and right frontal sinus were slightly inflamed. | 1. Type 2 diabetes mellitus; 2. Right hip arthroplasty; 3. Left femoral head necrosis | 1.Anxiety, 2.depression, 3.sleep disorders |
| 10 | F | 60 | mild | 1. Lacunar infarction in bilateral basal ganglia. 2. Leukoencephalopathy. 3. Mild brain atrophy. 4. Bilateral internal carotid atherosclerosis. | 1. Coronary heart disease; 2. Hypertensive cerebral infarction; 3. Hypokalemia; 4. Hepatic cyst; 5. Renal cyst; 6. Aortic atherosclerosis; 7. Carotid atherosclerosis | 1.Anxiety, 2.depression, 3.sleep disorders |
| 11 | F | 84 | severe | 1. Lacunar infarction in bilateral basal ganglia. 2. Leukoencephalopathy. 3. Mild brain atrophy. 4. Bilateral internal carotid atherosclerosis. | 1. Type 1 respiratory failure; 2. Hypertension grade 3 (extremely high risk); 3. Cardiac insufficiency; 4. Mixed dementia. | 1.Dementia, 2.disturbance of consciousness |
| 12 | M | 51 | mild | 1. Cerebral ischemia in bilateral frontal and parietal lobes. 2. Calcification in the white matter area of the posterior horn of the right lateral ventricle. 3. Left maxillary sinusitis. | 1.Anxiety, 2.depression, 3.sleep disorders | |
| 13 | F | 79 | severe | 1. Bilateral basal ganglia lacunar infarction. 2. Leukoencephalopathy3.brain atrophy. | 1. Type 2 diabetes mellitus; 2. Hypertension grade 3 (extremely high risk); 3. Hypokalemia; 4. Hypoproteinemia; 5. Lacunar cerebral infarction | disturbance of consciousness |
| 14 | F | 62 | mild | 1. Lacunar infarction in bilateral basal ganglia. 2. Mild brain atrophy. 3. Bilateral internal carotid atherosclerosis. | 1. Type 2 diabetes mellitus; 2. Hypertension | 1.State of anxiety, 2.state of depression |
| 15 | F | 69 | Dangerous and severe | 1. Lacunar infarction in bilateral basal ganglia. 2. Leukoencephalopathy; brain atrophy. 3. Bilateral internal carotid atherosclerosis. | 1. Femoral head fracture; 2. Hypertension; 3. Type 2 diabetes mellitus | 1.Disturbance of consciousness, 2.dementia, 3.sleep disorder |
| 16 | M | 64 | severe | 1. Lacunar infarction in bilateral basal ganglia. 2. Brain atrophy. 3. Bilateral internal carotid atherosclerosis. 4. Bilateral ethmoid sinus, maxillary sinus, sphenoid sinus and left frontal sinusitis。 | 1. Bacterial pneumonia; 2. Hypoxemia; 3. Hypoproteinemia; 4. Hypertension grade 2 (high risk); 5. Renal dysfunction; 6. Liver dysfunction; 7. Organic psychosis; 8. Bilateral carotid atherosclerosis | 1.Dementia, 2.anxiety, 3.psychomotor excitement, 4.sleep disorders |
| 17 | F | 66 | severe | 1. Cerebral ischemic changes should be considered, combined with MRI examination. 2. Brain atrophy. 3. Bilateral internal carotid atherosclerosis. | 1. Cervical spondylosis; 2. Mixed hyperlipidemia; 3. Sleep disorder; 4. Moderate risk group of hypertension; 5. Bilateral internal carotid atherosclerosis | 1.Dementia, 2.anxiety, 3.depression, 4.sleep disorders |
| 18 | M | 61 | mild | 1. Cerebral ischemic changes | Left ethmoid sinusitis | Sleep Disoders |
| 19 | M | 82 | Dangerous and severe | 1. Large area cerebral infarction in right basal ganglia and frontal parietal lobe, lacunar infarction in pontine and bilateral basal ganglia radiation coronal area, 2. White matter disease, brain atrophy. 3. The wall calcification of bilateral internal carotid artery. | Cerebral infarction | coma |
| 20 | M | 61 | Dangerous and severe | 1. Lacunar infarction in bilateral basal ganglia. 2. Small calcification under the right frontal lobe cranial plate. | 1. Acute exacerbation of chronic obstructive pulmonary disease; 2. Aortic atherosclerosis; 3. Pleural hypertrophy; 4. Lacunar infarction | 1.Disturbance of consciousness, 2.psychomotor excitement, 3.anxiety, 4.sleep disorder |
| 21 | M | 69 | severe | 1. Lacunar infarction in bilateral basal ganglia. 2. The right lateral ventricle was slightly enlarged, | 1. Acute coronary syndrome; 2. Benign prostatic hyperplasia; 3. Cervical spondylosis | 1.Disturbance of consciousness, 2.psychomotor excitement, 3.anxiety, 4.sleep disorder |
| 22 | F | 70 | severe | Leukoencephalopathy Brain atrophy | 1. Parkinson's syndrome; 2. Sequelae of cerebral infarction; 3. Mild anemia; 4Vascular demantia. 5. Electrolyte disorder (low sodium, low chloride, low calcium); 6.Abnormal liver function | 1.Disturbance of consciousnes, 2.Psychomotor excitemen, |
| 23 | M | 57 | mild | Lacunar infarction in bilateral basal ganglia. | 1. Migraine; 2. Uremia | Anxiety, sleep disorders |
Table 1: Primary clinical data of 23 patients
Results
Mental symptoms of patients
The most common are sleep disorders, anxiety and depression, and the most serious is the disturbance of consciousness, including coma and delirium. The most difficult to manage is psychomotor excitement, which brings great difficulties to treatment and management. There are other cognitive disorders. A few had compulsive symptoms and psychotic manifestations. 11 cases was company with disturbance of consciousness. 9 cases had cognitive disorders, 2 cases of which had been diagnosed as Alzheimer’s disease, and 1 of which had been diagnosed as vascular dementia and 1 of which had been diagnosed as mixed dementia before hospitalization. Most patients had sleep disorders, anxiety and depression.
Brain CT results
All patients had positive results. Three results are common. One is senile change, brain atrophy, including ventricular enlargement, widened sulcus, and leukoaraization. The second is cerebral ischemia, including infarct and softening focus, which occurs in the basal ganglia and around the ventricles. The most patients had both brain atrophy and cerebral ischemia. The atypical brains imagine show in Figures 1-3.
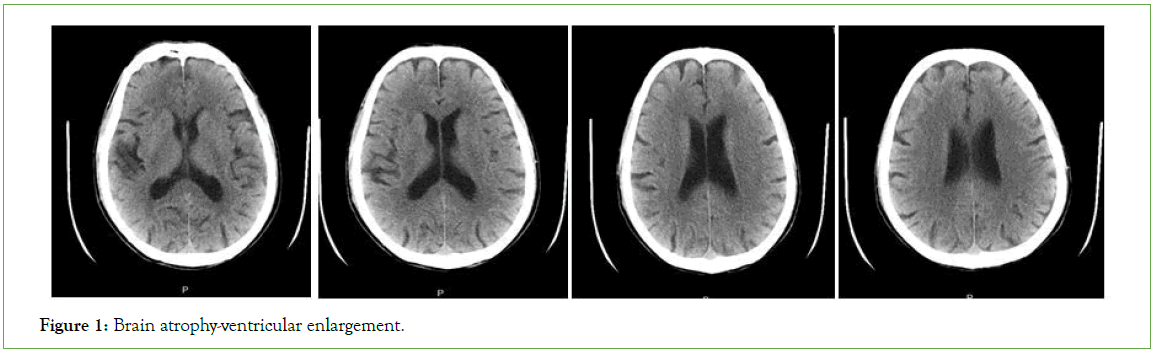
Figure 1: Brain atrophy-ventricular enlargement.
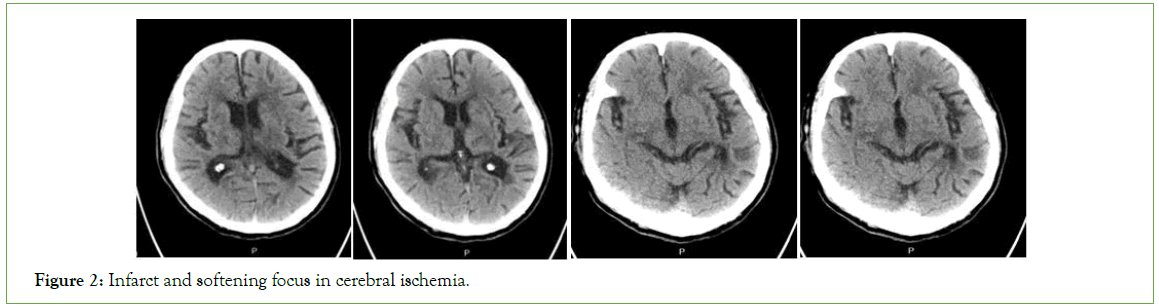
Figure 2: Infarct and softening focus in cerebral ischemia.
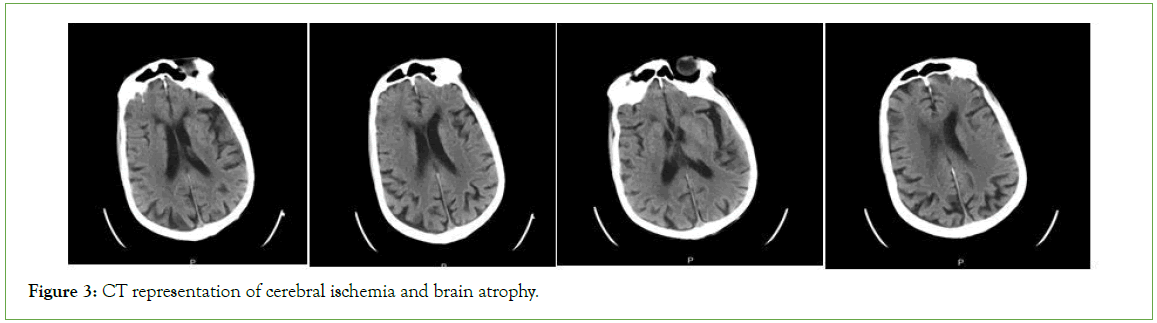
Figure 3: CT representation of cerebral ischemia and brain atrophy.
COVID-19 pneumonia, psychiatric symptoms and brain imaging
(1) The influence of COVID-19 pneumonia on mental symptoms: Most of the patients with consciousness disturbance were critically ill, which type always was dangerous and heavy, almost all patients had sleep disorders, anxiety and depression, and some patients had delirium with psychomotor excitement.
(2) The relationship between brain image and mental symptoms: The patients with severe mental symptoms usually occur in the old age and have more physical diseases, especially both brain atrophy and cerebral infarction. (3) The some patients had cognitive impairment, which mainly related the brain CT abnormality that may further aggravate in case of COVID-19 pneumonia. (4) The most patients had anxiety and depression related to both stress and biology impacts of COVID-19 pneumonia see Table 2.
| N | Male | Female | Age | Average number of physical disease | Average number of CNS disease1 | Average number of diagnosis by brain CT | Type of COVID-19 pneumonia | |
|---|---|---|---|---|---|---|---|---|
| Disturbance of consciousness | 11 | 7 | 4 | 76.2 | 4.2 | 4.2 | 3 | S2:6 DS3:5 |
| Impairment of cognition | 9 | 5 | 4 | 77.1 | 5.7 | 4.1 | 3.1 | S2:6 DS3:3 |
Note: 1. Number of CNS disease=Number of diagnosis by Brain CT+Clinical CNS disease
2. S=Severe
3. DS=Dangerous and Severe
Table 2: Information of patients with disturbance of consciousness and impairment of cognition
Discussion
In a new study, of 214 patients included 88 (41.1%) had severe infection and 126 (58.9%) had non-severe infection. Of these, 78 (36.4%) had various neurologic manifestations that involved CNS, PNS, and skeletal muscles [7], and 40% patients with COVID-19 pneumonia had various psychological manifestations that involved depression, anxiety, insomnia, suicide [9,10]. These result showed that COVID-19 pneumonia influenced both physical and psychological aspects.
Disturbance of consciousness is not only a symptom of central nervous system, but also a mental symptom, but more often, it is considered to be a more serious clinical manifestation. It strongly suggests that the central nervous system has been compromised. In our 23 case reports, nearly half of the cases (11/23) had disturbance of consciousness. Most of these patients had severe infection, were older and had a variety of physical diseases. These conclusions were similar to those of previous studies, but there is something special about the cases we report, which is that the patients have already suffered from central nervous system injury that is brain atrophy, cerebral infarction or both, as seen by head CT scan [7]. Therefore, this is also an important factor for these patients to have disturbance of consciousness.
Moreover, nervous system manifestations were significantly more common in severe infections compared with non-severe infections [7]. They included acute cerebrovascular disease, patients with ischemic stroke or with cerebral hemorrhage or with ischemic, impaired consciousness and skeletal muscle injury. In the severe group, some patient had a seizure characterized by a sudden onset of limb twitching, foaming in the mouth, and loss of consciousness, especially in acute stage of COVID-19 [7,8,11]. But we just report disturbance of consciousness, and also report the disorder of cognition, which also suggest more serious clinical manifestation.
The delirium was one kind of consciousness disturbance. The study showed that 28% patients with severe COVID-19 presented confusion during the acute illness [11]. When data for patients with COVID-19 were examined (including preprint data), there was evidence for delirium (confusion in 26 (65%) of 40 intensive care unit patients and agitation in 40 (69%) of 58 intensive care unit patients in one study, and altered consciousness in 17 (21%) of 82 patients who subsequently died in another study) [11]. When patients presented delirium, they always had disturbance of behavior with agitation, which also was import reason of consultation liaison psychiatry.
As to disturbance of consciousness, the patents with impaired cognition and severe infections, were higher older, had more physical disease, more impaired CNS that be seen by brain CT. The study found 34.1% patients with severe infection of COVID-19 had impaired memory during acute stage and 18.9% in the post-illness stage [11]. Generally, the impaired cognition was related to exited brain atrophy and cerebral ischemic. But we also do not know that neurologic manifestations are caused by the virus directly or by the pulmonary disease or other organ damage indirectly [8].
It was certain that impairment of CNS induce impaired cognition. In the patients reported, some patients had been diagnosed as Alzhemer’s disease, mixed dementia which was disease characterized by disorder of cognition. And some patients had been diagnosed as Parkinson’s disease which was disease possibly induced disorder of cognition. But what cannot be ruled out is that COVID-19 pneumonia can cause cognitive impairment in these elderly patients in a special way, and moreover these patients already have the damage that can be seen by head CT.
Symptoms that are less severe than consciousness and cognitive impairment are negative emotional symptoms. Prevalence of depression and anxiety symptoms were diagnosed in 35.9% and 38.5% of the patients, respectively [9]. The most of patients we reported had the depression and anxiety. Coronavirus Disease 2019 (COVID-19) has affected everyone around the world while often disrupting medical practices in non-COVID-19 cases and specifically in prenatal care. The systematic review revealed that during the acute illness, common symptoms among patients admitted to hospital for SARS or MERS included confusion (36 (27.9%; 95% CI 20.5%-36% cover) of 129 patients), depressed mood (42 (32.6%; 24.7%-40.9%) of 129), anxiety (46 (35.7%; 27.6%-44.2%) of 129), impaired memory (44 (34.1%; 26.2%-42.5) of 129), and insomnia (54 (41.9%; 22.5%-50.5) of 129) [11]. These results showed that the patients with COVID-19 experienced more negative affection, such as depression, anxiety. Our reports also showed most patients experienced depression and anxiety.
There was a finding showed a high rate of depression and anxiety in COVID-19 patients [9]. The prevalence of depression was 35.9%: 20.5% for mild depression, 12.8% for moderate depression, and 2.6% for severe depression. Almost four out of 10 (38.5%) patients were diagnosed with anxiety: 20.5% with mild anxiety, 12.8% with moderate anxiety, and 2.6% with severe anxiety. Nearly quarters (24.3%) of the patients were diagnosed as having both depression and anxiety. Multivariate linear regression found having family members diagnosed with COVID-19 and family members who died from COVID-19 were independent predictors of both higher depression severity index and anxiety score. Being female was also independently associated with depression severity index in COVID-19 patients. It was very pity that we did not analyze the risk with depression and anxiety. But ratio of our patients with depression and anxiety was more than 40%. It may also relate to their special findings by head CT.
The patients with brain atrophy and cerebral ischemia always presented emotional regulation disturbance. There was a study revealed brain structural abnormalities in emotional regulation and sensory processing regions of anxious depression, which may suggested distinct neurobiological mechanisms of this (Major Depressive Disorder) MDD specifier and could help explain different clinical manifestations in anxious depression from pure depression [12]. But psychological distress of COVID-19 may had importer role, as these findings of previous studies showing that public health emergencies can cause mental-health problems, such as the Wenchuan and Lushan earthquakes, the 2014 Ebola outbreak, and Severe Acute Respiratory Syndrome (SARS) [13-16].
Sleep disorder was very common psychological symptom without specificity. About 29.2% (95% CI, 28.8%-29.6%) general populations had insomnia. The people with occupational exposure risks and residents in Hubei province had increased odds of symptoms of insomnia (adjusted ORs, 1.60 (95% CI, 1.45-1.77). The confirmed patients with COVID-19 had more increased odds of symptoms of insomnia (adjusted ORs, 3.06 (95% CI, 1.73- 5.43) the systematic review 42% patients had insomnia in acute illness, 100% patients had sleep disorder in the post-illness stage [11,17]. The patients we reported almost had sleep disorder, for patients, besides the impact of psychological factors, there may be more important biological factors, especially those with severe pneumonia, which induced insomnia, anxiety and depression [18,19].
COVID-19 may impact both CNS and psychology. Despite the occurrence of symptoms-such as Shortness of Breath (SOB)-associated with severe manifestations of COVID-19, only the severities of smell and taste loss were associated with depressed mood and anxiety. These results may raise the novel possibility of emotional disturbance as a CNS manifestation of COVID-19 given trans-olfactory tract penetration of the Central Nervous System (CNS) by coronaviruses [20].
Conclusion
Unfortunately, our report does not have such data. There is no evaluation and test of olfactory and taste sense, no correlation analysis with negative emotion and no correlation analysis between this and CT results of head, which is insufficient. COVID-19 Pneumonia patients with cranial CT abnormality were easier to had mental symptoms, which include severe symptoms of consciousness disturbance, cognitive impairment, and common symptom of anxiety and depression, sleep disorder. The special attention should been to it. The consultation liaison psychiatry will play import role.
References
- World Health Organization. Coronavirus disease 2019 (COVID-19) situation report-76. 2020.
- Pan A, Liu L, Wang C, Guo H, Hao X, Wang Q, et al. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. Jama. 2020;323(19):1915-1923.
- Shanafelt T, Ripp J, Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. Jama. 2020;323(21):2133-2134.
- Reger MA, Stanley IH, Joiner TE. Suicide mortality and coronavirus disease 2019-a perfect storm?. JAMA Psychiat. 2020;77(11):1093-1094.
- Li W, Yang Y, Liu ZH, Zhao YJ, Zhang Q, Zhang L, et al. Progression of mental health services during the COVID-19 outbreak in China. Int J Biol Sci. 2020;16(10):1732.
- Xiang YT, Jin Y, Cheung T. Joint international collaboration to combat mental health challenges during the coronavirus disease 2019 pandemic. JAMA Psychiat. 2020;77(10):989-990.
- Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77(6):683-690.
- Pleasure SJ, Green AJ, Josephson SA. The spectrum of neurologic disease in the severe acute respiratory syndrome coronavirus 2 pandemic infection: Neurologists move to the frontlines. JAMA Neurol. 2020;77(6):679-680.
- Nie XD, Wang Q, Wang MN, Zhao S, Liu L, Zhu YL, et al. Anxiety and depression and its correlates in patients with coronavirus disease 2019 in Wuhan. In J Psychiatry Clin Pract. 2021;25(2):109-114.
- Reger MA, Stanley IH, Joiner TE. Suicide mortality and coronavirus disease 2019—a perfect storm?. JAMA Psychiat. 2020;77(11):1093-1094.
- Rogers JP, Chesney E, Oliver D, Pollak TA, McGuire P, Fusar-Poli P, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiat. 2020;7(7):611-627.
- Peng W, Jia Z, Huang X, Lui S, Kuang W, Sweeney JA, et al. Brain structural abnormalities in emotional regulation and sensory processing regions associated with anxious depression. Prog Neuropsychopharmacol Biol Psychiatry. 2019;94:109676.
- Xie Z, Xu J, Wu Z. Mental health problems among survivors in hard-hit areas of the 5.12 Wenchuan and 4.20 Lushan earthquakes. J Ment Health. 2017;26(1):43-49.
- Ji D, Ji YJ, Duan XZ, Li WG, Sun ZQ, Song XA, et al. Prevalence of psychological symptoms among Ebola survivors and healthcare workers during the 2014-2015 Ebola outbreak in Sierra Leone: a cross-sectional study. Oncotarget. 2017;8(8):12784.
- Shultz JM, Baingana F, Neria Y. The 2014 Ebola outbreak and mental health: current status and recommended response. Jama. 2015;313(6):567-568.
- Mak IW, Chu CM, Pan PC, Yiu MG, Chan VL. Long-term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry. 2009;31(4):318-3126.
- Shi L, Lu ZA, Que JY, Huang XL, Liu L, Ran MS, et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw Open. 2020;3(7):e2014053.
- Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5):1729.
- Yohannes AM. COPD patients in a COVID-19 society: depression and anxiety. Expert Rev Respir Med. 2021;15(1):5-7.
- Speth MM, Singer-Cornelius T, Oberle M, Gengler I, Brockmeier SJ, Sedaghat AR. Mood, anxiety and olfactory dysfunction in COVID-19: Evidence of central nervous system involvement?. Laryngoscope. 2020;130(11):2520-2525.
Citation: Jin W, Chen X, Ren H, Liu J, Sun W (2023) Psychopathology Analysis of 23 Cases with COVID-19 Pneumonia Accompanied by Abnormal Brain Imagine. J Psychia. 26:643.
Copyright: © 2023 Jin W, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

