Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
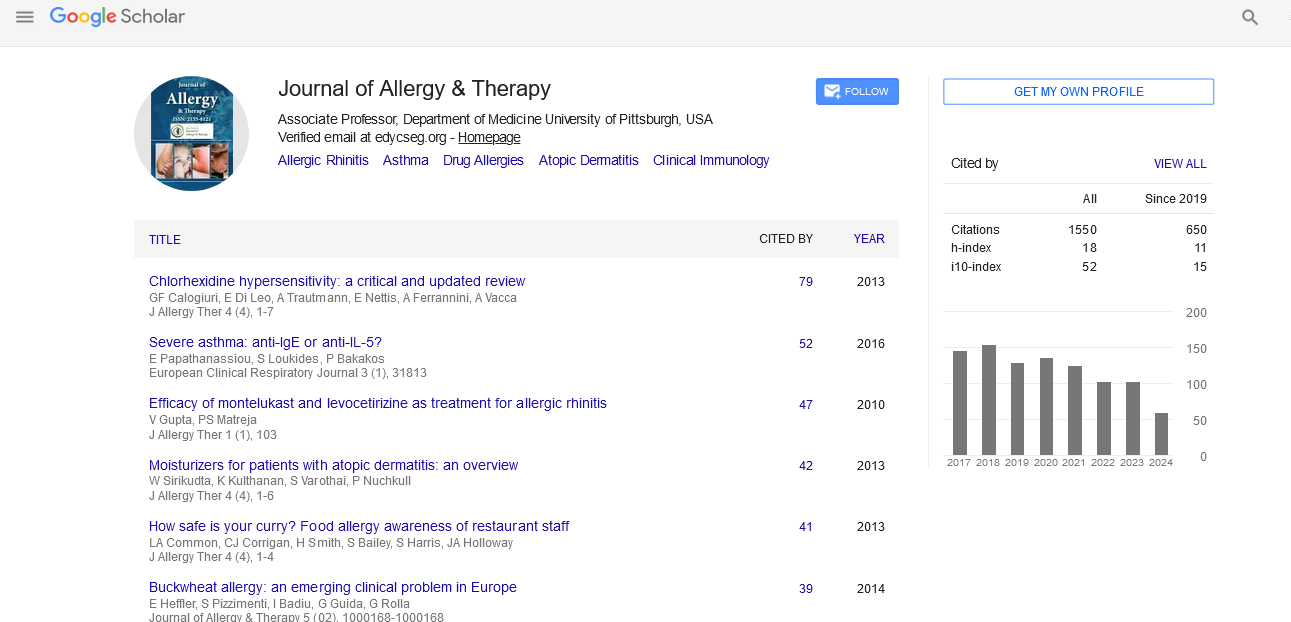
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Opinion Article - (2022) Volume 13, Issue 9
Pollen Sensitization on Patients with Respiratory Allergic Diseases
Santosh Pokhrel*Received: 01-Sep-2022, Manuscript No. JAT-22-18293; Editor assigned: 05-Sep-2022, Pre QC No. JAT-22-18293 (PQ); Reviewed: 19-Sep-2022, QC No. JAT-22-18293; Revised: 27-Sep-2022, Manuscript No. JAT-22-18293 (R); Published: 05-Oct-2022, DOI: 10.35248/2155-6121.22.13.305
Description
Due to their negative effects on quality of life, including social interaction, school attendance, and job performance, allergic airway diseases, such as Bronchial Asthma (BA) and Allergic Rhinoconjunctivitis (AR), are significant health and economic burdens. Allergy-related airway illnesses can arise for a variety of reasons, including genetic and environmental influences. Pollen is a significant environmental element that can lead to respiratory allergies. A distinctive feature of pollinosis is a country-specific, recurrent pattern of symptoms that occur during the pollen season. The symptoms of respiratory allergies are present year-round in patients who are sensitive to both seasonal (such as pollen) and perennial allergens (such as House Dust Mites (HDM), cockroaches, and moulds) and are exacerbated during the pollen season. The pollen season and the flowering season are related, but air pollution and climate change are the primary factors affecting pollen allergenicity. Pollution increases the amount of pollen allergenic proteins, particularly in metropolitan regions, and modifies these proteins into more allergenic components that cause allergies in susceptible people. On the other hand, the timing, length, geographic range, and dispersion of the pollen season are all impacted by climate change [1].
Most pollen allergies come from grasses, weeds, and trees. 40% of pollen sensitivity is brought on by grass pollen because of its prolific production and widespread dissemination. Numerous studies conducted in the United States revealed that grass pollen was primarily to blame for summer visits, whereas tree pollen was the cause of 25,000-50,000 hospital admissions for asthma throughout the spring. Weeds, on the other hand, are more common in the fall. The primary weeds that produce weed pollen on a global scale are parietaria, ragweed, mugwort, sunflower, and Russian thistle. Oral allergy syndrome develops in people who have previously been sensitive to aeroallergens and plant-derived allergens. Oral Allergy Syndrome (OAS), an acute hypersensitivity reaction, causes itching of the lips, tongue, and throat when raw fruits or vegetables come into contact with the oral mucosa [2].
In 2%-10% of instances, OAS may be accompanied by more serious symptoms including angioedema or anaphylaxis. Profiling, pathogenesis-related protein 10, and lipid transfer proteins are the key allergenic factors in OAS. Skin Prick Tests (SPT) and/or the detection of serum IgE in entire allergen extracts have historically been used to support patient anamnesis in the diagnosis of allergic disorders. Both approaches are effective at identifying reactivity to allergen extracts, but they are unable to pinpoint the precise components that cause sickness. The creation of Component-Resolved Diagnosis (CRD), sometimes referred to as molecular diagnostic, has made it possible to pinpoint the specific molecular allergen components that are the cause of sensitization. Since the introduction of allergen-specific immunotherapy, this trait, which allows discriminating between symptoms related to cross-reactivity and those evoking allergens, has been especially important. SPT is the preferred technique in many otorhinolaryngology departments due to its lower cost, despite the fact that CRD has become more widely accepted as standard practice in many allergy units. This raises the danger of utilizing SPT, patients receiving insufficient immunotherapies for their respiratory allergies [3].
The use of immunotherapy in those individuals has been driven by the correlation between sensitization to particular allergens and the emergence of respiratory disorders like asthma and rhinitis. In reality, the only causative treatment for allergic rhinitis that can lessen symptoms and the requirement for medication treatments at this time is allergen-specific immunotherapy. However, these treatments are frequently predicated on SPT diagnoses in ordinary clinical practice, presuming sensitivity to major allergens. The kind of respiratory allergy or the intensity of the symptoms did not significantly correlate with sensitization profiles revealed by SPT in our population. Contrarily, CRD permitted linking sensitizations to Der p, Der f, and Lep d with asthma (with or without concurrent rhinitis), as well as linking sensitizations to Der p and Lep d with asthma [4].
According to the multivariate analysis, which supports this dust mite allergens was significantly influenced by the type of disease, whereas group 2 (Der p 2 and Der f 2) house dust mite allergens were significantly influenced by the severity of the disease. Sensitization to Lep d 2 was also significantly influenced by both the type and severity of the disease. There have been similar associations between different pollens and the type of respiratory ailment described. To our knowledge, however, this is the first study demonstrating a connection between the type/ severity of a disease and household dust mite allergens [5].
The importance of using CRD to evaluate the sensitization profile of patients with respiratory allergies is strengthened by consistent findings that specific antigens are associated with clinical characteristics of the disease, despite the fact that the evidence for these particular relationships is still inconclusive.
Conclusion
The ability of CRD to depict more accurate sensitization profiles and identify candidates to symptom-triggering antigens suggests that routine use of CRD in this setting may provide remarkable benefits for the management of patients with respiratory allergy, finding, sensitization to group 1 (Der p 1 and Der f 1) houseeven though the relationship between symptoms and particular antigens is still poorly understood.
REFERENCES
- Simpson EL, Bieber T, Guttman-Yassky E, Beck LA, Blauvelt A, Cork MJ, et al. Two phase 3 trials of dupilumab versus placebo in atopic dermatitis. N Engl J Med 2016;375(24):2335-2348.
[Crossref] [Google Scholar] [Pubmed]
- Beck LA, Thaçi D, Deleuran M, Blauvelt A, Bissonnette R, de Bruin-Weller M, et al. Dupilumab provides favorable safety and sustained efficacy for up to 3 years in an open-label study of adults with moderate-to-severe atopic dermatitis. N Engl J Med. 2020;21(4):567-577.
[Crossref] [Google Scholar] [Pubmed]
- de Bruin‐Weller M, Thaçi D, Smith CH, Reich K, Cork MJ, Radin A, et al. Dupilumab with concomitant topical corticosteroid treatment in adults with atopic dermatitis with an inadequate response or intolerance to ciclosporin A or when this treatment is medically inadvisable: A placebo‐controlled, randomized phase III clinical trial (LIBERTY AD CAFÉ). Br J Dermatol. 2018;178(5):1083-1101.
- Simpson EL, Bieber T, Guttman-Yassky E, Beck LA, Blauvelt A, Cork MJ et al. Two phase 3 trials of dupilumab versus placebo in atopic dermatitis. N Engl J Med. 2016;375(24):2335-2348.
[Crossref] [Google Scholar] [Pubmed]
- Thaci D, Simpson EL, Beck LA, Bieber T, Blauvelt A, Papp K, et al. Efficacy and safety of dupilumab in adults with moderate-to-severe atopic dermatitis inadequately controlled by topical treatments: A randomised, placebo-controlled, dose-ranging phase 2b trial. Lancet. 2016;387(10013):40-52.
[Crossref] [Google Scholar] [Pubmed]
Citation: Pokhrel S (2022) Pollen Sensitization on Patients with Respiratory Allergic Diseases. J Allergy Ther. 13:305.
Copyright: © 2022 Pokhrel S. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.