Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Euro Pub
- Google Scholar
- Quality Open Access Market
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2021) Volume 7, Issue 4
Platelet-Rich Plasma Injection in Extensor Tendon in Proximal Interphalangeal Joint for Pain and Sensitivity
Charl H. Woo1*, Christine M. Olanrewaju2, Jose J. Diaz1, Joseph E. Mouhanna3, Kathryn M. Nelson3 and Cristóbal S. Berry-Cabán42Physical Medicine and Rehabilitation Clinic, Physical Performance Service Line, Brian D. Allgood Army Community Hospital APO, AP, USA
3Pain Medicine Fellowship Program, Larkin Community Hospital South Miami, FL, USA
4Department of Clinical Investigations, Womack Army Medical Center, Fort Bragg, NC, USA
Received: 18-Aug-2021 Published: 15-Sep-2021, DOI: 10.35248/2684-1320.21.7.158
Abstract
Chronic tendon injury can cause notable impact to a patient’s physical function. Regenerative platelet rich plasma (PRP) injections have been utilized to treat a multitude of chronic musculoskeletal tendon injuries over the years, with generally positive results. To date, there have been no case reports of platelet rich plasma injections to the finger extensor tendons or collateral ligaments. Our case reviews the clinical course and outcome experienced by a 32-yearold Asian American male suffering from chronic right middle finger pain and sensitivity near the proximal interphalangeal (PIP) joint resulting from sequelae of prior laceration injury. Despite intense efforts with occupational therapy, the patient’s pain failed to resolve after two years. A single PRP injection under ultrasound guidance was trialed, and subsequent to treatment, the patient’s pain and range of motion improved, albeit by a small margin. Platelet-rich plasma injections may be considered as an adjunct to standard rehabilitation measures for finger soft tissue injury, particularly in outpatient physical medicine and rehabilitation or pain medicine clinic settings; however, more research is needed to validate results experienced by this single patient.
Keywords
Platelet-rich plasma; Extensor laceration; Pain management; Regenerative medicine; Musculoskeletal medicine
Introduction
Injections have been utilized for many years to treat patients with musculoskeletal pathology. There are numerous substances a clinician can consider injecting for musculoskeletal pain such as corticosteroid, hyaluronic acid, hypertonic dextrose injection (prolotherapy), and platelet-rich plasma (PRP) [1]. In particular, PRP is a more novel therapeutic treatment, regenerative in nature, with potential to repair tissues with poor healing capacity [2,3]. PRP is an autologous blood-derived product containing a high concentration of platelets with multiple growth factors and cytokines that promotes an inflammatory response and healing at the site of injection over a long period [2,4-6].
Various anatomic sites of soft tissue or joint injury in the body can be treated with PRP, for example the knees, trochanteric bursa, and glenohumeral joints [7]. More specifically, tendon pathologies are among many musculoskeletal conditions for which PRP can be used to stimulate regenerative healing [8]. Locations including Achilles tendon, patellar tendon, rotator cuff tendons, and elbow tendons have been common anatomic targets for PRP injection. Tendinopathy in the finger, however, has not been commonly considered for treatment using PRP. This article reports a case of a patient who suffered a traumatic laceration to the extensor tendon. Associated sequelae, including tendon thickening and scar tissue at the proximal interphalangeal joint (PIP) of the right middle finger, that was treated with PRP is also discussed.
Case Presentation
A 32-year-old Asian American male with a history of trauma to the extensor digitorum tendon adjacent to the PIP joint of the right middle finger presented to a physical medicine and rehabilitation (PM&R) clinic due to persistent pain and sensitivity upon firm pressure over the PIP joint, primarily during interactions involving handshakes. Localized pressure over the injury site also elicited a brief electrical sensation. The patient complained of difficulty during activities of daily living (ADLs) involving flexion at the PIP joint such as grabbing objects or typing on a computer.
The Primary injury had occurred approximately 22 months prior to presentation. The patient sustained a right middle finger laceration by a sharp metal object over the dorsal PIP joint (Figure 1a). Immediately after injury, the site was flushed with water and, the skin approximated with topical 2-octyl cyanoacrylate (Dermabond) by a physician. Otherwise, no further treatment was administered (Figure 1b). Initial post-injury deficits included reduced active flexion at the PIP at 34 degrees due to pain as well as pain and sensitivity to touch and deep pressure over the injury site. One month after injury, the patient underwent 2 months of occupational therapy including table-top activities with blocks and TheraPutty, scar reduction, and soft tissue mobilization. While flexion at the joint improved mildly; pain, touch and pressure sensitivity over the laceration site remained unchanged.
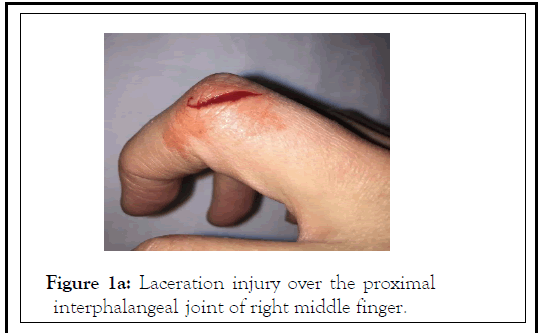
Figure 1a: Laceration injury over the proximal interphalangeal joint of right middle finger.
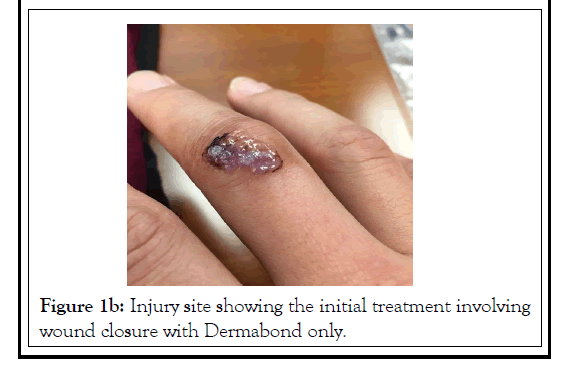
Figure 1b:Injury site showing the initial treatment involving wound closure with Dermabond only.
Due to persistent symptoms, advanced imaging was ordered. Magnetic resonance imaging (MRI) revealed a partially lacerated extensor tendon at the neck of the proximal phalanx of the middle finger with scar tissue formation (Figures 2a and 2b). There was an interruption of occupational therapy for over a year due to work-related relocation. The patient once resumed occupational therapy included table-top activities with TheraPutty and hand web, instrument assisted soft tissue mobilization, Fluidotherapy, and blood flow restriction therapy. Therapy continued to improve the reduced flexion at the PIP joint to 61 degrees before experiencing pain; however, the pain and sensitivity to deep palpation to the injury site never improved.
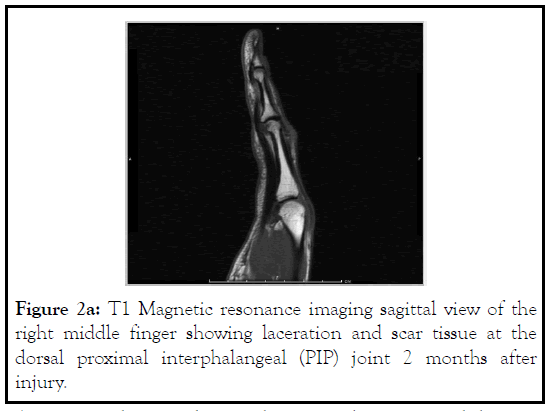
Figure 2a: T1 Magnetic resonance imaging sagittal view of the right middle finger showing laceration and scar tissue at the dorsal proximal interphalangeal (PIP) joint 2 months after injury.
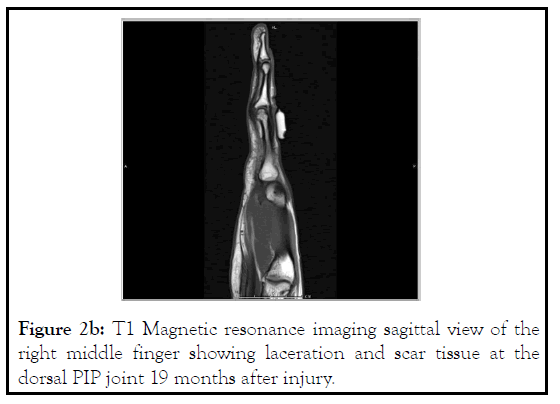
Figure 2b: T1 Magnetic resonance imaging sagittal view of the right middle finger showing laceration and scar tissue at the dorsal PIP joint 19 months after injury.
Approximately 14 weeks into the resumed occupational therapy, a follow-up MRI of the right hand was performed that showed thickening of the extensor tendon over the middle finger PIP joint (Figure 2b). Despite multiple months of occupational therapy, the patient continued to feel pain and sensitivity to pressure at the PIP joint as well as sensation of fullness at the joint upon flexion. Due to suboptimal improvement, PRP was considered as the next treatment plan to help improve the laceration-induced tendinopathy and associated symptoms of pain, sensitivity, and ROM abnormalities.
The PIP joint of the right middle finger was examined under ultrasound, which showed thickened extensor tendon in the area. Cortical irregularity was also visualized over the dorsolateral PIP joint (Figure 3a). Using the Arthrex Autologous Conditioned Plasma (ACP®) double-syringe system, 10 cc of blood was drawn from the patient. The ACP® double-syringe was spun in a Hettich Rotofix 32 A centrifuge at the rate of 2000 revolutions per minute for 5 minutes. Once centrifugation was completed, the separated plasma layer was removed from the double-syringe for PRP use. Using a 27-gauge needle, a digital nerve block was performed with 1.5 cc of 1% lidocaine on the medial and lateral aspect of the finger in the interdigital web space. Once anesthesia was confirmed, a 1.5” 27-gauge needle was inserted in a lateral-to-medial plane approach and was used to inject 0.5 cc of PRP at the site while simultaneously peppering the area with the needle tip (Figure 3b). Gentle tenotomy was performed at the area of extensor tendon thickening during the injection. At the completion of the procedure, the needle was withdrawn. There were no apparent complications.
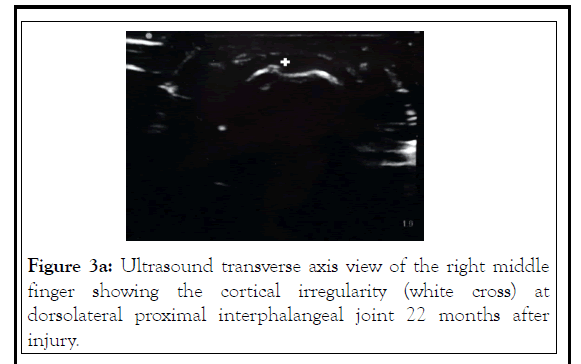
Figure 3a: Ultrasound transverse axis view of the right middle finger showing the cortical irregularity (white cross) at dorsolateral proximal interphalangeal joint 22 months after injury.
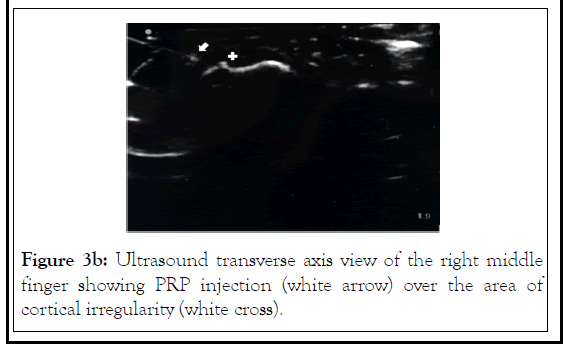
Figure 3b: Ultrasound transverse axis view of the right middle finger showing PRP injection (white arrow) over the area of cortical irregularity (white cross).
At a 1-month follow-up evaluation the patient reported minimal improvement in pain, sensitivity or ROM. Later, after approximately 4 months of concurrent occupational therapy, the injury site was re-evaluated.
At that appointment, the patient experienced minor improvement with desensitization in severity as well as the frequency of shooting pain and sensitivity upon deep palpation such as a firm handshake or accidental colliding at the injury site with an object. Prior to the procedure, the patient experienced electrical sensation and pain between 8 and 9 (on a scale of 10) upon every episode of colliding or firm pressure over the injury site. After the procedure, the frequency of shooting pain and sensitivity upon colliding or firm pressure over the injury site occurred approximately 8 out of 10 times, while the pain was rated at 6 to 7 (on a scale of 10). The patient had less difficulty in situations encountering pressure at the injured joint and while performing ADLs involving finger flexion at the joint. However, no particular improvement was seen with associated sensation of fullness upon full flexion at the PIP joint. No further follow-up occurred due to the patient’s relocation.
Discussion
Platelet-rich plasma was first described by Kingsley in 1954 for thrombocyte concentrate to treat severe thrombopenia [9]. Many more clinicians later helped establish the term for the plasma containing a higher platelet count than that of peripheral blood as a treatment method for thrombocytopenia [10,11]. However, it was not until the 1970s when PRP was more widely experimented in the medical field with Matras incorporating into fibrin adhesive for reimplantation trials onto the skin in a rat [12].
Over the years PRP been interchangeably called rich growth factors, platelet concentrate, and platelet-rich fibrin matrix [13]. It is an autologous plasma preparation with concentrated platelets containing cytokines and growth factors that contribute to enhanced repairment and regeneration [14,15]. Platelets play a vital role in wound healing with their ability to repair the vasculature and nearby tissues after injury. The process starts as the collagen from the injured tissue encounters the plateletcarrying vascularity that activates its platelets [16]. Cytokines, along with other mediators, are secreted upon activation and become intensified with the synthesis of growth factors and cytokines over time [17]. With such growth factors contributing to wound healing, PRP can effectively improve tissue repair [18].
During the 1970s, PRP was widely used in a variety of fields such as urology, maxillofacial surgery, gynecology, and plastic surgery. It gained popularity as a treatment option for musculoskeletal pathologies when multiple professional athletes started receiving PRP for sports injuries [19,20]. The popularity of PRP continued to grow in the general population as it helped improve tendon and ligament pathology as they cause marked morbidity and can create a profound impact on work, recreational activities, and overall quality of life [21].
There have been many clinical trials and publications investigating the efficacy of PRP in tendon-related disorders in various anatomical areas. Filardo et al conducted a literature review of PRP use in tendinopathies in select areas including patellar tendon, Achilles tendon, lateral elbow tendon, and rotator cuff that concluded a beneficial effect in patellar tendon compared to other available modalities such as simple wholeblood injections [8]. A systematic review and meta-analysis of thirty-seven articles comprising 1031 participants by Chen et al evaluated the efficacy of PRP injections to reduce pain in various tendon pathologies including rotator cuff, lateral epicondylitis, and anterior cruciate ligament (ACL). The study revealed that PRP might reduce pain associated with lateral epicondylitis and rotator cuff pathology [21]. However, as of this moment, no publications have been found specific to reduction in pain and sensitivity to a tendon injury in the hand with PRP.
The importance of this case brings awareness to consideration of PRP for tendon pathologies in small joints such as fingers. An injury to joints in the hand, whether distal interphalangeal, proximal interphalangeal, or metacarpal phalangeal, can create an impairment in various severity in leisure activities, occupation, as well as activities of daily living. The cost of healthcare and the length of rehabilitative treatment before being able to return to normal duty and lifestyle can also be a major factor causing stress to patients with hand injuries. A study conducted by Gustafsson et al revealed many stress factors for patients in the early stage of acute traumatic hand injury. Impairment in functioning, ADL’s, leisure activity, and pain were among the stressors pertinent to those with such hand injuries [22].
As seen in our patient, the tendinopathy from laceration was causing difficulty in multiple settings such as greeting others with handshakes or simply performing ADLs requiring full flexion at the PIP joint. After suboptimal improvement with therapies, PRP injection was performed to cause wound healing with an objective to relieve the associated symptoms more effectively. Although the sensation of fullness at the PIP joint upon finger flexion showed no relevant improvement, other pertinent symptoms such as pain and sensitivity to pressure over the injury site ultimately showed some improvement at the 5-month follow-up post PRP to the injured extensor tendon in the right middle PIP joint.
This case, however, had confounding factors that required the patient to continue to receive occupational therapy concurrently to maximize the benefit in symptomatic improvement. While the PRP injection did provide some benefit, it is not clear of how much benefit the patient received from the injection alone due to his concurrent occupational therapy to the hand. There was also no follow-up after the 5-month evaluation due to the patient’s relocation, making it impossible to evaluate the improvement over a longer time.
Conclusion
The advancement in medicine has allowed physicians to provide a variety of treatment options to patients who suffer from musculoskeletal injuries. PRP is an autologous blood preparation with concentrated platelets injected to create augmented healing. It has been used to treat injuries to tendons and ligaments. More common pathologies, such as rotator cuff, lateral epicondylitis, and ACL injury, have shown good response to PRP in pain reduction. Injury to a tendon in a small hand joint such as the PIP joint can also receive benefit from PRP in symptomatic improvement such as ROM abnormalities, pain and sensitivity at the injury site. Although it is important to maximize benefit by providing a multidisciplinary approach including injection and therapy to reduce symptoms, an opportunity to evaluate the efficacy of PRP for a tendon injury in a small hand joint over a long period without other concurrent interventions during healing and recovery should be considered.
Disclosures
Human subjects
Consent was obtained from the participant in this study.
Financial relationships
All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
REFERENCES
- Hulsopple C. Musculoskeletal therapies: musculoskeletal injection therapy. FP Essent. 2018; 470:21-26.
- Fotouhi A, Maleki A, Dolati S, Aghebati-Maleki A, Aghebati-Maleki L. Platelet rich plasma, stromal vascular fraction and autologous conditioned serum in treatment of knee osteoarthritis. Biomed Pharmacother. 2018; 104:652-660.
- Martínez-Martínez A, Ruiz-Santiago F, García-Espinosa J. Platelet-rich plasma: myth or reality? Radiologia. 2018; 60(6):465-475.
- Bos-Mikich A, de Oliveira R, Frantz N. Platelet-rich plasma therapy and reproductivemedicine. J Assist Reprod Genet. 2018;35(5):753-756.
- Zhu Y, Yuan M, Meng H, et al. Basic science and clinical application of platelet-rich plasma for cartilage defects and osteoarthritis: a review. Osteoarthr Cartil. 2013; 21(11):1627-1637.
- Sun Y, Feng Y, Zhang C, Chen S, Cheng X. The regenerative effect of platelet-rich plasma on healing in large osteochondral defects. Int Orthop. 2010;34(4):589-597.
- Wittich CM, Ficalora RD, Mason TG, Beckman TJ. Musculoskeletal injection. Mayo Clin Proc. 2009;84(9):831-837.
- Filardo G, Di Matteo B, Kon E, Merli G, Marcacci M. Platelet-rich plasma in tendon-related disorders: results and indications. Knee Surg Sports Traumatol Arthrosc. 2018;26(7):1984-
- 1999.
- Kingsley C. Blood coagulation: evidence of an antagonist to factor VI in platelet-rich human plasma. Nature. 1954;173(4407):723-724.
- Andia I. Platelet-rich plasma biology. In: Ascensao Alves RF, Grimalt Santacana R, eds. Clinical Indications and Treatment Protocols with Platelet-rich Plasma in Dermatology. Barcelona: Ediciones Mayo, S.A.; 2016:3-15.
- Andia I, Abate M. Platelet-rich plasma: underlying biology and clinical correlates. Regen Med. 2013;8(5): 645-658.
- Matras H. Die Wirkungen verschiedener Fibrinpräparate auf Kontinuitätstrennungen der Rattenhaut [Effect of various fibrin preparations on reimplantations in the rat skin]. Osterr Z Stomatol. 1970;67(9):338-359.
- Alves R, Grimalt R. A review of platelet-rich plasma: history, biology, mechanism of action, and classification. Skin Appendage Disord. 2018;4(1):18-24.
- Dhillon RS, Schwarz EM, Maloney MD. Platelet-rich plasma therapy-future or trend? Arthritis Res Ther. 2012;14(4):1-10.
- Marwah M, Godse K, Patil S, Nadkarni N. Is there sufficient research data to use platelet-rich plasma in dermatology? Int J Trichology. 2014;6(1):35-36.
- Amable PR, Carias RBV, Teixeira MVT, Pacheco IDC, Farias Corrêa do Amaral RJ, GranjeiroJM, et al. Platelet-rich plasma preparation for regenerative medicine: optimization and quantification of cytokines and growth factors. Stem Cell Res Ther. 2013;4(3):67.
- Senzel L, Gnatenko DV, Bahou WF. The platelet proteome. Curr Opin Hematol. 2009;16(5):329-333.
- Xu J, Gou L, Zhang P, Li H, Qiu S. Platelet‐rich plasma and regenerative dentistry. Aust Dent J. 2020;65(2):131-142.
- Andia I, Rubio-Azpeitia E, Martin J, Abate M. Current concepts and translational uses of platelet rich plasma biotechnology. In: Ekinci D, ed. Biotechnology. Rijeka, Croatia: InTech; 2015:1-31.
- Lynch M, Bashir S. Applications of platelet-rich plasma in dermatology: a critical appraisal of the literature. J Dermatolog Treat. 2016;27(3):285-289.
- Chen X, Jones IA, Park C, Vangsness Jr CT. The efficacy of platelet-rich plasma on tendon and ligament healing: a systematic review and meta-analysis with bias assessment. Am J Sports Med. 2018;46(8):2020-2032.
- Gustafsson M, Persson LO, Amilon A. A qualitative study of stress factors in the early stage of acute traumatic hand injury. J Adv Nurs. 2000;32(6):1333-1340.
Citation: Woo CH, Olanrewaju CM, Diaz JJ, Mouhanna JE, Nelson KM,Berry-Cabán CS (2021) Platelet-Rich Plasma Injection in Extensor Tendon in Proximal Interphalangeal Joint for Pain and Sensitivity. J Pain Manage Med. 7:158.
Copyright: © 2021 Woo CH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

