Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- Google Scholar
- SHERPA ROMEO
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2019) Volume 7, Issue 3
Percutaneous Transluminal Stenting of Infra-Renal Abdominal Aorta Penetrating Atherosclerotic Ulcer
Sara Mokhtari1,2*, Abdellah Rezziki1,2, Adnane Benzirar1,2 and Omar El Mahi1,22Department of Vascular Surgery, University Hospital Center Mohammed VI, Oujda, Morocco
Received: 16-Aug-2019 Published: 03-Oct-2019
Abstract
Predominantly found in the descending thoracic aorta, Penetrating Atherosclerotic Ulcer (PAU) is uncommon in the infra-renal abdominal aorta. It is defined as atherosclerotic lesions with ulceration of the aortic intima and media, and rupture of the internal elastic lamina. PAU is considered as a rare serious clinical entity that may induce aortic dissection, aortic rupture, and secular aortic aneurysm typically occurs in elderly hypertensive patients with severe systemic atherosclerosis disease. The treatment of PAU remains a subject of considerable controversy. With the development of percutaneous techniques of stent placement, stenting has emerged as a new option in the treatment of abdominal aorta PAU. We report a 68 years old man with PAU being diagnosed with symptoms of intermittent claudication of both lower limbs; that underwent intraluminal stenting. The technical success rate was 100%. We obtained excellent short and medium term clinical success without finding any complications related. Although open surgical repair is an effective therapeutic option, endovascular treatment of abdominal aortic PAU is a safe attractive alternative to surgery therapy that should be considered as the treatment of choice. Keywords: Claudication penetrating atherosclerotic ulcer; Angioplasty; Palmaz stent; Abdominal aorta
Keywords
Claudication-penetrating atherosclerotic ulcer; Angioplasty; Palmaz stent; Abdominal aorta
Introduction
Penetrating atherosclerotic ulcer is defined as atherosclerotic lesions with ulceration of the aortic intima and media, and rupture of the internal elastic lamina. It is characterized by its uncommon localization in the infra-renal abdominal aorta and its rare clinical entity that may induce to serious complications.
The emergence of endovascular therapy has made percutaneous transluminal angioplasty a safe attractive alternative to surgery for the therapeutic management of PAU. Through this publication, we would like to report our youthful experience with the balloon expandable Palmaz stent employed for the treatment of infrarenal abdominal aorta PAU.
Case Report
A 68 years old man, with the vascular factors following: Gender, age, obesity, cigarette smoking, diabetes mellitus, high blood pressure, ischemic stroke and ischemic heart disease operated by venous bypass; was referred for bilateral lower limb claudication stage II b. The physical examination revealed femoral pulses weakly palpable while the distal pulses were not palpables.
A Doppler ultrasound was performed, completed by an angio Computed Tomography (CT) confirmed the diagnosis of PAU of the infra-renal abdominal aorta taking the aspect of a localized dissection with an intimal flap spread over 36 mm of length.
An arteriography was performed by retrograde direct puncture of the right Common Femoral Artery (CFA) after being dissected and controlled. The arteriography; that was carried out using a sheath 7 French (F), a 0.035 guide wire type angioflex and a straight catheter 4F; showed a stenosis of the infra-renal abdominal aorta just before bifurcation. The stenotic lesion was classified as an eccentric ulcerated plaque extended over a length of approximately 40 mm. Pre-procedurally, a bolus of 2500 UI heparin was given. After clamping and arteriotomy of CFA, a Palmaz stent mounted on 22 mm balloon-catheter; was placed across the stenosis and inflated. As post-stenting findings, the ulcerated plaque was stabilized.
Post-procedurally, a curative subcutaneous heparin for 48 hours and a unique dose of 300 mg of clopidogrel maintained by a daily dose of 75 mg and aspirin 75 mg/day were set. The postoperative results were simple. Clinically, the femoral and distal pulses were perceived. The patient was subsequently discharged under medical treatment and consultation appointment.
Three months later, the follow-up has been noticed by a significant improvement of the walking area. An angio-CT of control has been performed and revealing no complications (Figures 1-4).
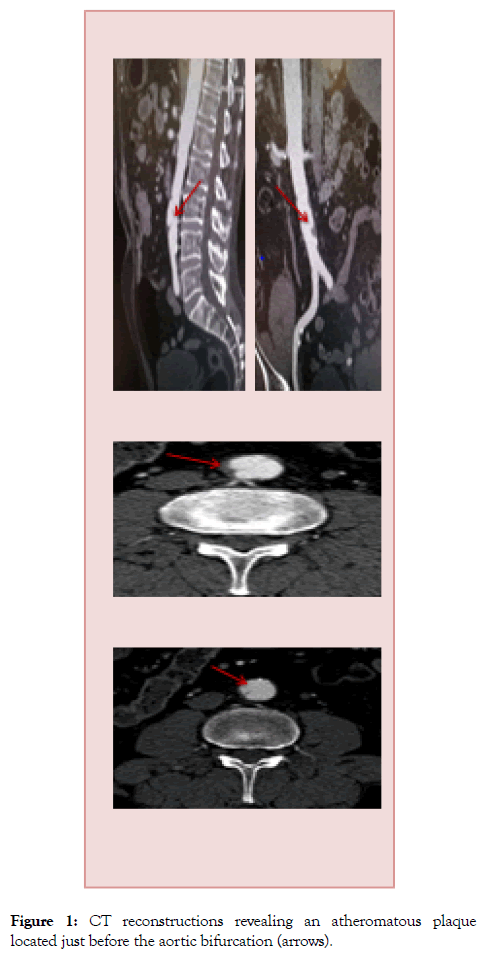
Figure 1: CT reconstructions revealing an atheromatous plaque located just before the aortic bifurcation (arrows).
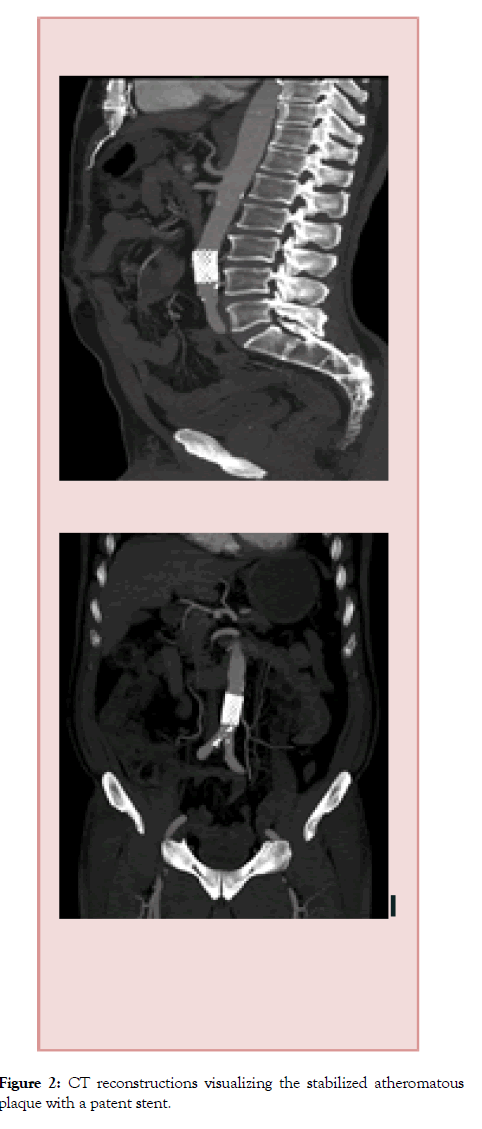
Figure 2: CT reconstructions visualizing the stabilized atheromatous plaque with a patent stent.
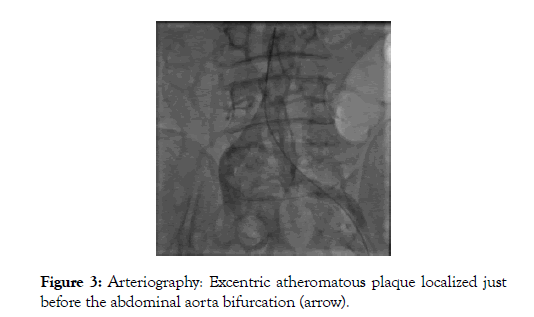
Figure 3: Arteriography: Excentric atheromatous plaque localized just before the abdominal aorta bifurcation (arrow).
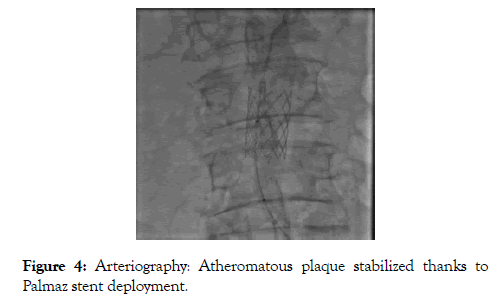
Figure 4: Arteriography: Atheromatous plaque stabilized thanks to Palmaz stent deployment.
Discussion
The PAU is an anatomopathological entity recently individualized. It fits into the framework of aortic syndromes acute, its prevalence is between 2.3% and 7.6% [1].
Patients with a PAU are characterized by the importance of associated pathologies: arterial hypertension, heart disease, diabetes and chronic renal failure [2-5]. Our patient presents all these diseases except kidney failure. It is important to sign that this particular context has an impact on therapeutic management and prognosis.
PAU and others pathologies of aortic abdominal have similar clinical manifestations, they must be distinguished radiologically. At present, CT is considered the reference imaging tool since it allows a rapid and straight forward evaluation of the aortic cavity and wall. Yucel et al. [6] demonstrated that magnetic imaging is superior to CT for diagnosis of abdominal aortic diseases in differentiating acute intramural hematoma from atherosclerotic plaque and chronic intraluminal thrombus. MR imaging has the additional advantage of allowing multiplanar imaging without use of contrast material. In our study, the lesion was diagnosed by means of an angio-CT of abdominal aorta and lower limbs.
Previously, surgery was the only available treatment. Most authors suggested that surgical intervention with grafting of the affected area is the treatment of choice because of possible malignant involvement [2,3]. Although it is successful in relieving symptoms, a significant morbidity and mortality was noticed. That’s why it is indicated, particularly, in situations of persistent or recurrent pain, hemodynamic instability, and a rapidly expanding aortic diameter. On the other hand, some authors believe that immediate surgical treatment is not always required because the disease may have a benign course [7,8]. Harris et al. [8] had noticed that few patients, from their study, developed aortic dissection or aortic rupture during the followup. These authors emphasized that most patients with PAU are at high risk for surgical intervention because of their advanced age and poor general health. In recent years, stent grafts have been introduced, and treatment experiences with them for PAU have been reported [9,10].
Conclusion
Surgery has been a traditional treatment option for atherosclerotic diseases of the abdominal aorta with welldocumented long-term results. The emergence of endovascular therapy has made percutaneous transluminal angioplasty a seductive alternative in the treatment of abdominal aorta infrarenal PAU.
REFERENCES
- Eggebrecht H, Herold U, Schmermund A, Lind AY, Kuhnt O, Martini S, et al. Endovascular stent-graft treatment of penetrating aortic ulcer: results over a median follow up of 27 months. Am Heart J. 2006;151(2):530-536.
- Stanson AW, Kazmier FJ, Hollier LH, Edwards WD, Pairolero PC, Sheedy PF, et al. Penetrating atherosclerotic ulcers of the thoracic aorta: natural history and clinicopathologic correlations. Ann Vasc Surg. 1986;1(1):15-23.
- Cook JP, Kazmier FJ, Orszulak TA. The penetrating aortic ulcer: pathologic manifestations, diagnosis and management. Mayo Clin Proc. 1998;63(7):718-725.
- Vilacosta I, San Roman JA, Aragoncillo P, Ferreiros J, Mendez R, Graupner C, et al. Penetrating atherosclerotic aortic ulcer: documentation by transesophageal echocardiography. J Am Coll Cardiol. 1998;32(1):83-89.
- Coady MA, Rizzo JA, Hammond GL, Pierce JG, Kopf GS, Elefteriades JA. Penetrating ulcer of the thoracic aorta: what is it? How do we recognize it? How do we manage it? J Vasc Surg. 1998;27(6):1006-1016.
- Yucel EK, Steinberg FL, Egglin TK, Geller SC, Waltman AC, Athanasoulis CA. Penetrating aortic ulcers: diagnosis with MR imaging. Radiology. 1990;177(3):779-781.
- Kazerooni EA, Bree RL, Williams DM. Penetrating atherosclerotic ulcers of the descending thoracic aorta: evaluation with CT and distinction from aortic dissection. Radiology. 1992;183(3):759-765.
- Harris JA, Bis KG, Glover JL, Bendick PJ, Shetty A, Brown OW. Penetrating atherosclerotic ulcers of the aorta. J Vasc Surg 1994;19(1):90-99.
- Tsuji Y, Tanaka Y, Kitagawa A, Hino Y, Taniguchi T, Sugimoto K, et al. Endovascular stent-graft repair for penetrating atherosclerotic ulcer in the infrarenal abdominal aorta. J Vasc Surg. 2003;38(2):383-388.
- Piffaretti G, Tozzi M, Lomazzi C, Rivolta N, Caronno R, Castelli P. Endovascular repair of abdominal infrarenal penetrating aortic ulcers: a prospective observational study. IntJ Surg. 2007;5(3):172-175.
Citation: Mokhtari S, Rezziki A, Benzirar A, El Mahi O (2019) Percutaneous Transluminal Stenting of Infra-Renal Abdominal Aorta Penetrating Atherosclerotic Ulcer. J Vasc Med Surg 7:3. doi: 10.35248/2329-6925.19.7.384.
Copyright: © 2019 Mokhtari S et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited

