Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2020) Volume 6, Issue 3
Patients' Perceptions of the Discharge Process
Whitney Pollio E*Received: 18-Feb-2020 Published: 12-Jun-2020, DOI: 10.35248/2573-4598.20.6.150
Abstract
Hospital readmission rates estimates range as high as 79 percent. Research aimed at decreasing readmission is almost entirely from the perspective of health care providers. Patient insights potentially aid in efforts to improve transitions of care. The study’s purpose is to examine patients’ perceptions of the discharge process. Nine African-American adult females with congestive heart failure recently discharged from the hospital were asked to recall the experience of receiving written health care information. Interviews were transcribed, coded into themes, and validated through participant follow-up. Three themes emerged: 1) consumer-friendly information and materials; 2) humanization; and 3) health care team expertise. Consumer-friendly information and materials includes readability and comprehensiveness of materials. Humanization consists of providers showing patience, patient-centred care and personal touch. Health care team expertise includes professionalism and effective communication skills. The participants’ experiences suggest that decreasing readmissions rests on humanizing communication of discharge health information and instructions to patients.
Keywords
Patient education; Patient-provider communication; Health literacy
Introduction
Quality and transition of care are being closely scrutinized as potential processes influencing the costly dilemma of hospital readmissions, also referred to as recidivism. U.S. Hospitals spent $41.3 billion between January and November 2011 on readmissions within 30 days of patient discharge [1]. The Centers for Medicare and Medicaid Services state that the national hospital readmission rate for 2012 averaged 18.4 [2]. Recidivism adds to the overall healthcare cost because some insurance companies, including Medicare, deny payment for readmissions that occur within 30 days of being discharged. Because readmissions, especially ones not reimbursed, increase the cost of healthcare, interventions focusing on decreasing recidivism are presently ongoing at both state and national levels [3]. Most payers, including Medicare, believe that better organization of post-discharge care is key to reducing readmissions [1]. Providers and government-sponsored health literacy sites recommend making the materials easier to read in order to help patients understand their medical condition and its treatment [4]. Despite efforts to assure that patients are provided educational materials at the appropriate literacy level, recidivism rates have not significantly improved.
Traditional definitions of health literacy that focus solely or predominantly on written health information are not sufficient to encompass all factors influencing a patient ’ s ability to effectively obtain and use health information. To address this issue, Sorensen, Van den Broucke, Fullam, et al [5] developed a comprehensive definition: “Health literacy is linked to literacy and entails people's knowledge, motivation and competencies to access, understand, appraise, and apply health information in order to make judgments and decisions in everyday life concerning healthcare, disease prevention and health promotion to maintain or improve quality of life during the life course.” Health literacy includes patients’ ability to read, interpret, and act on health education information.
Approximately 36 percent of Americans have insufficient health literacy skills to fully understand and utilize healthcare information. Agarwal, Shah, Stone, Ricks & Friedlander [6] found that individuals with low health literacy use preventive health services at a lower rate and have poorer understanding of personal health conditions and treatment plans than individuals with adequate health literacy. This combination can result in poor health outcomes and health status, leading to increased hospitalization and healthcare costs. Patients with low health literacy are at an increased risk for hospital readmissions [7].
Despite efforts to decrease recidivism by producing written health information at the appropriate literacy level, rates remain relatively constant. Since the key to avoiding readmission is changing or maintaining patient behavior, one direction would be to examine patient experiences of the discharge process. By asking patients about their experience with health education materials and the discharge process, there is potential to gain insights into factors and processes beyond literacy materials and comprehension. Yet, a systematic review of the literature for 2005 – 2015 using the terms health literacy and patient education revealed that 74% of the research in health literacy is from the perspective of health professionals. Efforts to gain patients insights is lacking in current literature.
To address this need, research is required to explore barriers to meeting the needs of patients by considering the discharge process with particular attention to the patient perspective. Interviewing patients after hospital discharge has the potential to answer the following questions: What perceptions do patients have of the written healthcare information they receive? What perceptions do patients have of the experience of receiving written healthcare information at discharge? Are there factors other than the discharge materials that influence how patients perceive the discharge process?
The specific population being studied, African-American adult females recently hospitalized with congestive heart failure, was chosen because patients with congestive heart failure have a high tendency to be readmitted to the hospital within 30 days of being discharged [1]. Between January and November 2011, congestive heart failure was the most common medical condition associated with recidivism for Medicare patients with 1.35 million readmissions costing $1.7 billion [1]. African- American women are disproportionately affected by cardiovascular disease, including congestive heart failure [8]. Focusing on a specific high-risk group, particularly one with clear health disparities, has the potential to be both directly useful to addressing disparities for this population, while also providing information to guide inquiry into the broader patient population. Therefore, the purpose of this study is to explore patient perceptions of the discharge process, including health education materials, in a population of African-American females discharged from an inpatient cardiac care unit.
Methods
Participants of this study consisted of nine African-American adult females with a diagnosis of congestive heart failure. None of the nine participants were newly diagnosed, so all previously received information regarding their diagnosis. Participants were recruited from the same inpatient cardiac care unit and received similar written discharge information. Potential participants were approached prior to discharge and given an informed consent form to read and ask questions. All participants were English speaking with no identified cognitive deficits. Demographic information, such as age, socioeconomic status, marital status, degree of education and literacy level were not collected. Permission for all study procedures was received from the Institutional Review Board.
Participants were interviewed 48 hours to 10 days post hospital discharge. The open-ended interview protocol was guided using the following open-ended prompts: 1) Tell me about when you received your instructions at discharge. 2) Did you feel like that situation was handled to your satisfaction? 3) Was the information useful to your situation? and 4) Did the information you were given meet your needs?
The interviewer audio recorded the interviews, transcribed them and verified for accuracy using follow-up telephone interviews. Interviews lasted approximately 45 minutes each. One interview was conducted by telephone and the other eight were in person.
Analysis of the qualitative data gathered from these interviews used an open coding strategy. The interviewer reviewed all the interview data, identifying similarities among interviewees in experiences and examples provided. Initial coding included the development of as many thematic categories as possible. Additional themes were developed as needed as additional interviews were conducted. Conceptually similar concepts were grouped together to form seven themes. These themes were organized into three categories in order to address the research questions. Definitions of the themes were further developed as statements from participants were added. Phrases taken from the transcripts were added to the subthemes in order to demonstrate common themes among participants. Finally, the findings were member checked by telephone conversation with each one of the interviewees to validate the results of the analysis.
Results
As a result of this review process, 7 initial themes with brief descriptions were generated. In some cases, the name of the theme was provided by the interviewee, and in others the name of the theme emerged during the analytic process based on key similarities in descriptions across at least two interviews. The three categories with their 7 subthemes are described in Figure 1.
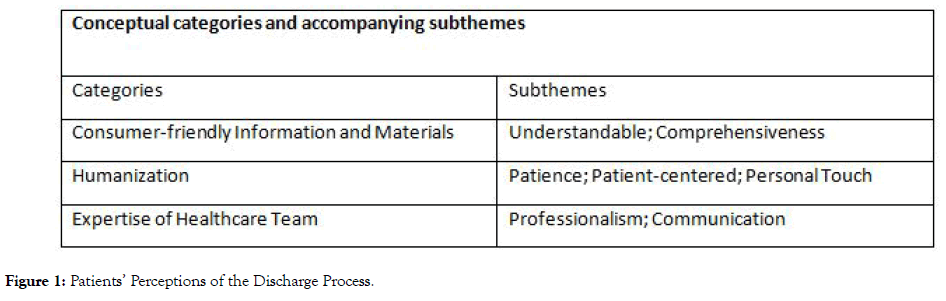
Figure 1: Patients’ Perceptions of the Discharge Process.
1. Consumer-friendly Information and Materials: This category included examples of participants reporting that the information and materials that they were given were easy to use and/or understand. The participants conveyed that the materials were readable and helpful. They also reported that the staff supplied them with comprehensive information for them to better understand their diagnosis and allow them to be better prepared for self-care.
Understandable: This subtheme referred to instances of participants conveying that the materials were able to be understood; intelligible. Participants reported that the written materials were easily understood and straightforward. None of the participants reported not being able to read the information that they were given.
Comprehensiveness: This subtheme included experiences where participants felt that the healthcare team had access to information that covered all elements or aspects of their care. Participants reported that the healthcare team shared information with them that they needed to be able to understand their condition and to better take care of themselves. Participants felt that the information that was shared with them covered all their healthcare needs.
2. Humanization: This category included three subthemes pertaining to the humanization of the participants. All the participants reported that they were treated more as humans rather than just another patient or number. They communicated that they were treated as individuals with specific needs. Participants presented examples where the healthcare team members went above and beyond what they considered as the normal standard of care. The content of the subthemes in this category was almost entirely positive in nature and were the majority of the content of all the interviews.
Patience: This subtheme included experiences where the participants felt that the healthcare team members gave them all the time and attention that they requested or needed. Participants noted that the nurses never rushed them and were willing to take all the time necessary to meet the needs of the participants. Participants could ask questions and the healthcare team took the needed amount of time to make sure that they were answered, explained and understood.
Patient-centered: This subtheme referred to the concept that healthcare and health information is customized and reflects patient needs, values and choices. Knowledge and information are freely shared between and among patients, care partners, physicians and other caregivers. Many participants remarked that they felt that their care and information was tailored to them and their specific needs. The nurses were accepting and tolerant of the participants ’ preferences. Eight of the nine participants shared experiences of feeling that the healthcare team showed a patient-centered approach to their care. This subtheme involves experiences of nurses asking or allowing the participants to make decisions according to their needs and preferences. It also includes examples of patient care and healthcare instructions meeting the individual participant ’ s needs and instances where participants felt that their care had been customized to meet their needs.
Personal Touch: This subtheme included experiences where the participants felt like they received special treatment outside of the normal standard of care. All the participants conveyed that healthcare team members went out of their way to do special tasks just for them. There were examples of the healthcare team going above and beyond to meet both medical needs and personal needs. The participants felt that these experiences facilitated a personal connection with members of the healthcare team.
3. Expertise of Healthcare Team: This category referred to instances where the healthcare team demonstrated both a breadth and depth of knowledge that covered all the participants ’ healthcare needs. It also referred to how the healthcare team presented themselves to the participants. Participants communicated that the healthcare team demonstrated a degree of knowledge that they had not experienced at other institutions. They also reported that the staff was competent in communicating their healthcare instructions.
Professionalism: This subtheme referred to instances where the participants felt that a member of the healthcare team demonstrated the demeanor and/or the competence of someone with the knowledge and skill of a professional. Participants reported that members of the healthcare team had the qualities and characteristics of a professional. These characteristics of professionalism were supported both by the actions of the healthcare team and by the quality of information that they shared with the participants.
Communication: This subtheme referred to participants experiencing that members of the healthcare team were successful in communicating both general healthcare information as well as information specific to their individual needs. Participants felt that the staff supplied them with all the information that they needed to be able to care for themselves after leaving the hospital. Participants also stated that the healthcare team was proficient in explaining the information that was given to them in written form.
The seven subthemes were overwhelmingly supported by participant quotes as shown in Table 1. The subthemes Understandable, Comprehensiveness, and Personal Touch were supported by quotes from 100% of the participants. Patience and Patient-centered were supported by 89% of participant quotes. Seventy eight percent of participants supplied quotes supporting Professionalism and Communication.
Table 1: Subthemes Supported by Participant Quotes.
| Participant Number | Understandable | Comprehensiveness | Patience | Patient-centered | Personal Touch | Professionalism | Communication |
|---|---|---|---|---|---|---|---|
| 1 | X | X | X | X | |||
| 2 | X | X | X | X | X | X | |
| 3 | X | X | X | X | X | X | X |
| 4 | X | X | X | X | X | X | |
| 5 | X | X | X | X | X | X | X |
| 6 | X | X | X | X | X | X | X |
| 7 | X | X | X | X | X | X | |
| 8 | X | X | X | X | X | X | X |
| 9 | X | X | X | X | X | X | X |
In this study, all the participants reported having an overall positive experience during the discharge process. All the participants contributed quotes that supported the category of expertise of healthcare team. Also, five of the participants supplied quotes to support all seven subthemes. During the interviews, they communicated that the healthcare team members exhibited both personable and professional behavior. Five out of the seven subthemes are about the behavior and competence portrayed by the healthcare team. Participants valued the behavior and competency of the healthcare team members as well as the relationship they formed between themselves and the healthcare team members. All the participants reported that the healthcare team treated them like individuals. Eight of the participants communicated that the healthcare team portrayed both patience and patient-centered care. All nine of the participants experienced a personal touch from the healthcare team. The category of humanization was found to be significant in all participants. Most participants also reported that the healthcare team was professional, knowledgeable and had excellent communication skills.
Discussion
The experiences of the participants interviewed for this study suggested that the most optimal approach to successful communication of discharge health information and instructions to patients were to humanize the patient using patience, personal touch and patient-centered care. The findings of this study suggest that if healthcare professionals are competent and treat patients as individuals, patients are more likely to report having a favorable perception of the discharge process. Participants conveyed that successful communication of both general healthcare information, as well as information specific to their individual needs, was influenced by the knowledge and expertise of the healthcare professional. If healthcare professionals are competent and treat patients as individuals, patients are more likely to report having a favorable perception of the discharge process.
Humanization was influential in patients’ perceptions of the discharge process. Although not previously seen as important to the health literacy discussion, participants from this study reported that nurses who took extra time with them or went out of their way to help them made them feel like individuals. This feeling of having a personal relationship fostered trust in the participants. Trusting in the healthcare team persuaded the participants to be more accepting of information and instruction from the healthcare team.
Participants reported that the expertise of the healthcare team members was a key factor in how they perceived the care and information that they received. The knowledge of the staff and their ability to communicate effectively influenced the willingness of the participants to accept the instructions they were given along with the overall impression they had of the entire discharge experience. Participants shared that the healthcare team was proficient at communicating information that they needed to manage their condition and provide selfcare.
Effective communication skills and spending time with patients during the discharge process may positively influence patients’ willingness to accept and ability to understand health education information. Participants felt that the quality of care and health information they received were far superior to what they had received during past experiences. Therefore, knowledge base and behavior of healthcare team members are influential in patients’ perceptions of the delivery of health education materials.
Although one reason for choosing African-American females as the sample was the potential for insights into this population, race never emerged as an issue in any of the interviews. Although it is possible that the questions asked did not lend themselves to discussions of race or disparities, it is also a possibility that in situations where discharge is perceived as positive in nature, race is not of relevance to the experience. It may be more likely that race is perceived of importance when the discharge experience is negative in nature. Obviously, the nature of race in the discharge process requires further inquiry.
Health literacy professionals argue that improved health literacy will lead to greater patient involvement, which, in turn, should lead to better patient outcomes [9]. Patients are most often given health information in written form; therefore, the focus of health literacy initiatives has been on creating written information at the appropriate literacy level. This study found that in addition to the written materials, the patient-provider relationship, including communication and information sharing, is a significant factor in determining patient perceptions of the discharge process. When discussing care and treatment in focus groups, patients identified poor communication between doctor and patient as a barrier to care [10]. In a study about patient preferences of sources of health information, patientprovider relationship and health literacy affect a patient’s ability to understand and use health information [11].
Strengths and Limitations
The high proportion of participants endorsing each theme argues for the validity of the findings. However, because qualitative inquiry is not strictly generalizable, the findings are only representative of the study population and the single medical condition.
Conclusion
The implementation of humanization of patients combined with a professional and competent healthcare team fosters a personal connection for the patient. Even though all participants reported that the health education materials were understandable and comprehensive, having a personal connection with the healthcare team promoted trust and willingness to accept instruction and information in the participants. This personal connection between patients and healthcare team members allows for information sharing which aids the healthcare team in understanding and meeting the needs of the patients. Allowing the patients to have input into the content of discharge information and having the information disseminated by a knowledgeable and competent healthcare team produces quality, a usable, patient-centred healthcare education material which leads to better patient outcomes. The perception patients have of the discharge process needs to be explored in other patient populations and other settings. Compiling data from additional studies has the potential of developing interventions to improve patient outcomes and reduce cost of healthcare.
REFERENCES
- Hines AL, Barrett ML, Jiang HJ, Steiner CA. Conditions with the largest number of adult hospital readmissions by payer, 2011. Agency for Healthcare Research and Quality. HCUP Statistical Brief number.
- Gerhardt G, Yemane A, Hickman P, Oelschlaeger A, Rollins E, Brennan N. Data shows reduction in Medicare hospital readmission rates during 2012. Medicare Medicaid Res Rev. 2013; 3:1-12.
- Elixhauser A, Steiner C. Readmissions to U.S. hospitals by diagnosis, 2010. Agency for Healthcare Research and Quality. HCUP Statistical Brief number: 153, 2013.
- Mueller SK, Giannelli K, Boxer R, Schnipper JL. Readability of patient discharge instructions with and without the use of electronically available disease-specific templates. J Am Med Inform Assoc. 2015;22:857-863.
- Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012;12.
- Agarwal N, Shah K, Ston, J, Ricks CB, Friedlander RM. Educational resources “over the head” of neurosurgical patients: the economic impact of inadequate health literacy. World Neurosurg. 2015;84:1223-1226
- Mitchell S, Sadikova E, Jack B, Paasche-Orlow MK. Health literacy and 30-day postdischarge hospital utilization. J Health Commun. 2012;17:325-338
- Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics-2013 update: a report from the American Heart Association. Circulation. 2013;127:e6-e245.
- Johnson A. Health literacy, does it make a difference? Aust J Adv Nurs. 2014;31:39-45.
- North CS, Devereaux R, Pollio DE, Hong BA, Jain MK, et al. Patient perspectives on hepatitis C and its treatment. Eur J Gastroenterol Hepatol. 2014;26:74-81.
- Longo DR, Schubert SL, Wright BA, LeMaster J, Williams CD, Clore JN. Health information seeking, receipt, and use in diabetes self-management. Ann Fam Med. 2010;8:334-340.
Citation: Pollio EW (2020) Patientsâ?? Perceptions of the Discharge Process. J Pat Care 6:150. doi: 10.35248/ 2573-4598.20.6.150
Copyright: © 2020 Pollio EW. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
