Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2023) Volume 14, Issue 4
Oral Hygiene Status: The Critical Parameter in Orthodontic Patients
Jothi Yadav*Received: 13-Apr-2023, Manuscript No. JCRB-23-20994 ; Editor assigned: 17-Apr-2023, Pre QC No. JCRB-23-20994 (PQ); Reviewed: 01-May-2023, QC No. JCRB-23-20994 ; Revised: 08-May-2023, Manuscript No. JCRB-23-20994 (R); Published: 15-May-2023, DOI: 10.35248/2155-9627.23.14.466
Abstract
Aim: The aim of this study was to assess the status of oral hygiene among patients using fixed mechanotherapy appliances.
Methods and Materials: Patients undergoing orthodontic treatment had their dental hygiene status assessed using the Gingival Bleeding Index (GBI), Plaque Index (PI), and Ortho Plaque Index (OPI) at three intervals.T0 (the first day), T1 (15 days), and T2 (30 days) for a month.
Results: 10 individuals (15–30 years old) receiving orthodontic treatment at the department of orthodontics and dentofacial orthopaedics, Adesh Institute of Dental Science and Research (AIDSR), Adesh University, chosen for the study. Results showed that the mean PI significantly decreased from T0 to T1 and then from T1 to T2, the GI significantly decreased from T0 to T1 but then did not differ significantly from T1 to T2, and the OPI significantly decreased from T0 to T1 but did not differ significantly from T1 to T2. For the PI, GI, and OPI, there was no discernible difference between the genders of the patients.
Conclusion: Patients undergoing orthodontic treatment may be more susceptible to gingivitis if they don't practise good oral hygiene at home. As a result, throughout orthodontic treatment, oral hygiene guidelines and a hygiene maintenance strategy must not be neglected.
Keywords
Oral hygiene; Fixed orthodontic mechanotherapy; Gingivitis
Introduction
In the context of contemporary dental care, adult patients are increasingly seeking orthodontic therapy. Oral hygiene is substantially more challenging after fixed orthodontic appliances have been fitted. As a result, patients wearing fixed orthodontic appliances are more likely to develop dental caries and gingivitis, which can lead to gingival attachment loss [1-3]. After three months of ongoing orthodontic treatment, the stimulated salivary flow rate, pH, buffer capacity, Plaque Index (PLI) scores, and lactobacilli levels all show a statistically significant increment [4]. Following the installation of fixed appliances, differences in the Plaque Index (PI), Bleeding Index (BI), and Pocket Depth (PD) measurements were discovered; these values were significantly higher than the baseline values [5]. There has been a reported change in the subgingival microbiota towards one that promotes disease, along with a statistically significant rise in spirochetes and fusiform bacilli. A significant change in oral microbiota was found in subjects with fixed appliances during the first six months of treatment [6]. Such a finding implies that gingivitis risk was substantial during their months of therapy, and periodontitis risk could not be ruled out [7]. Manschot described a patient who, as a result of orthodontic treatment and poor dental hygiene, had substantial mucogingival alterations, such as gingival recession [8]. Although periodontal disease can be exacerbated by an increase in bacteria, orthodontic appliances typically do not promote gingival irritation. On the other hand, motivated patients can both lower plaque buildup and gingival inflammation [9]. As a result, it is crucial to promote oral hygiene advice to orthodontic patients wearing fixed appliances [10]. The purpose of this study was to evaluate the level of oral hygiene in patients receiving fixed orthodontic therapy [11].
Materials and Methods
Patients in fixed mechanotherapy in the orthodontic department at Adesh Institute of Dental Sciences and Research, Bathinda were chosen for the study. The inclusion criteria:
1. Patients who have been using full-mouth fixed orthodontic appliances for at least six months.
2. No underlying illnesses.
3. No prior use of antibiotics within the previous three months.
4. No oral prophylaxis during the month preceding the research.
Orthodontic Plaque Index (OPI)
In order to assess the patient's oral hygiene and gingiva, two measurements were used: the Gingival Bleeding Index (GBI) and the Plaque Index (PI). The most important plaque accumulation zones, which are cervical to the bracket base and mesial and distal to the bracket body, were measured using the Orthodontic Plaque Index (OPI). The index formula shown in Table 1 was used to calculate OPI.
| SCORE | CRITERIA |
|---|---|
| 0 | No buildup of plaque on the surface of tooth surrounding the base of the bracket |
| 1 | Buildup of plaque on 1 tooth surface at the base of the bracket. |
| 2 | Buildup of plaque on 2 tooth surfaces at the base of the bracket. |
| 3 | Buildup of plaque on 3 tooth surfaces at the base of the bracket. |
| 4 | Buildup of plaque on 4 tooth surfaces at the base of the bracket and gingival |
Table 1: Accumulation zones measured in Orthodontic Plaque Index (QPI).
Gingival Index (GI)
All four surfaces of the teeth were checked to determine whether probing induced bleeding in order to determine the Gingival Bleeding Index (GI) (Table 2).
| SCORE | CRITERIA |
|---|---|
| 0 | Normal gingiva. |
| 1 | Mild inflammation-slight colour change, a small amount of edoema, but no bleeding when probing. |
| 2 | Moderate inflammation-redness, edema and glazing, bleeding on probing. |
| 3 | Severe inflammation with edoema, ulceration, and a propensity for spontaneous bleeding. |
Table 2: To determine the Gingival Bleeding Index (GI).
Plaque Index (PI)
For orthodontic patients, the Plaque Index (PI) was assessed on the bracket sides of one representative tooth from six sextants: the first molars on the upper right, upper centre, upper left, lower right, lower centre, and lower left. Using Loe and Silness' PI score, each tooth was split into four zones based on where it was located around the brackets: Mesial (M), Distal (D), Gingival (G), and Incisal (I). The second premolar served as the sextant in circumstances where the first molar was banded or absent. On the nonbracket side, the Loe and Silness PI were applied (Table 3).
| SCORE | CRITERIA |
|---|---|
| 0 | No plaque |
| 1 | Thin plaque coating near the gingival margin, only visible with probe scraping. |
| 2 | Moderate plaque coating along the gingival margin, interdental spaces free, but plaque is visible to the naked eye. |
| 3 | Abundant plaque coating along the gingival margin, interdental spaces filled with plaque. |
Table 3: To determine the patients Plaque Index (PI).
Data Analysis
The Statistical Package for the Social Sciences (SPSS 10; SPSS Inc., Chicago, IL, USA) was used to run statistical analyses after data was entered into the computer using the FoxPro programme (FoxPro 7.0; Sybase Inc., Dublin, CA, USA). Using a one-way analysis of variance (ANOVA), differences at the 5% significance level (p0.05) were determined.
Results
Mean Age of male and female study participants was found to be comparable (Table 4).
| Sex | N | Mean | Std. Deviation | |
|---|---|---|---|---|
| Age | Males | 4 | 19.25 | 4.425 |
| Females | 6 | 20.00 | 2.898 |
Table 4: Descriptive of age of the study participants.
The Friedman test was used to compare the Mean Plaque Index at T0, T1, and T2 within groups. The mean PI score at T0, T1, and T2 differed in a manner that was statistically significant. Wilcoxon test was used to perform a post hoc pairwise comparison. It was discovered that from T0 to T1 and subsequently from T1 to T2, the mean PI dramatically dropped (Table 5).
| GINGIVAL INDEX | |||||
|---|---|---|---|---|---|
| N | Minimum | Maximum | Mean | Std. Deviation | |
| T0 | 10 | 0.80 | 2.00 | 1.5320 | 0.39454 |
| T1 | 10 | 0.50 | 1.50 | 1.0820 | 0.39355 |
| T2 | 10 | 0.3 | 1.0 | 0.570 | 0.1767 |
| P value | <0.001, S | ||||
| Post hoc Pairwise comparison | T0>T1>T2 | ||||
Table 5: Intragroup comparison of mean plaque index at T0, T1 and T2.
The Friedman test was used to compare the Mean Gingival Index at T0, T1, and T2 within each group. A statistically significant difference was found in the mean GI score at T0, T1 and T2. Post hoc pairwise comparison was done using Wilcoxon test. The mean GI was discovered to have greatly lowered from T0 to T1, however there was no discernible change in GI between T1 and T2 (Table 6).
| GINGIVAL INDEX | |||||
|---|---|---|---|---|---|
| N | Minimum | Maximum | Mean | Std. Deviation | |
| T0 | 10 | 0.60 | 1.50 | 1.0060 | 0.30826 |
| T1 | 10 | 0.5 | 0.6 | 0.540 | 0.0516 |
| T2 | 10 | 0.16 | 0.60 | 0.3760 | 0.13818 |
| P value | <0.001, S | ||||
| Post hoc Pairwise comparison | T0>T1, T2 | ||||
Table 6: Intragroup comparison of mean gingival index at T0, T1 and T2.
Intragroup comparison of Mean OPI at T0, T1 and T2 was done using Friedman test. The mean OPI score at T0, T1 and T2 showed a statistically significant difference. Post hoc pairwise comparison was done using Wilcoxon test. The average OPI was observed to have drastically dropped from T0 to T1, however from T1 to T2, there was no discernible difference in OPI (Table 7).
| ORTHO PLAQUE INDEX | |||||
|---|---|---|---|---|---|
| N | Minimum | Maximum | Mean | Std. Deviation | |
| T0 | 10 | 2 | 3 | 2.7 | 0.483 |
| T1 | 10 | 1 | 2 | 1.6 | 0.516 |
| T2 | 10 | 1 | 2 | 1.2 | 0.422 |
| P value | <0.001 | ||||
| Post hoc Pairwise comparison | T0>T1>T2 | ||||
Table 7: Intragroup comparison of mean OPI at T0, T1 and T2.
Discussion
Patients having orthodontic treatment with fixed appliances are more likely to experience gingival inflammation because oral hygiene is more difficult. Dental plaque is mostly to blame for gingivitis. Plaque buildup around fixed orthodontic appliances is encouraged by the patient's inability to properly clean his or her teeth, which might eventually cause gingival inflammation [12-15]. Salivary bacterial counts generally rise after orthodontic appliance insertion, especially Lactobacillus. Similar to this, six months after appliance insertion, rises of two to three folds in clinical indexes and motile organism counts have also been noted [2], along with an early increase in anaerobes and Prevotella intermedia and a decline in facultative anaerobes [16]. Similar to the microbiota found in periodontally diseased locations, the subgingival microflora has changed to a periopathogenic community [3,17]. Irregular tooth alignment may make it harder to control plaque [18]. While other studies have not, some studies have found a connection between crowding and periodontal disease. Nonetheless, effective plaque control is the most important factor in maintaining good oral hygiene [19,20]. The purpose of this study was to assess oral hygiene among orthodontic patients at Adesh Institute of Dental Sciences and Research. Despite the fact that more than half of the patients brush their teeth twice a day, their oral hygiene was poor. In general, PI and OPI were reduced after oral prophylaxis, with mean values of 1.5-0.5 and 2.7-1.2, respectively. This result is in line with earlier studies that revealed an increase in visible plaque on tooth surfaces after the use of braces [19-21]. Both an increase in plaque-retentive areas and the patient's incapacity to practise good oral hygiene are to blame for this. However, increasing the frequency of brushing does not guarantee clean teeth. As a result, tooth brushing frequency alone cannot be used to assess the quality of oral hygiene [22] (Figure 1).
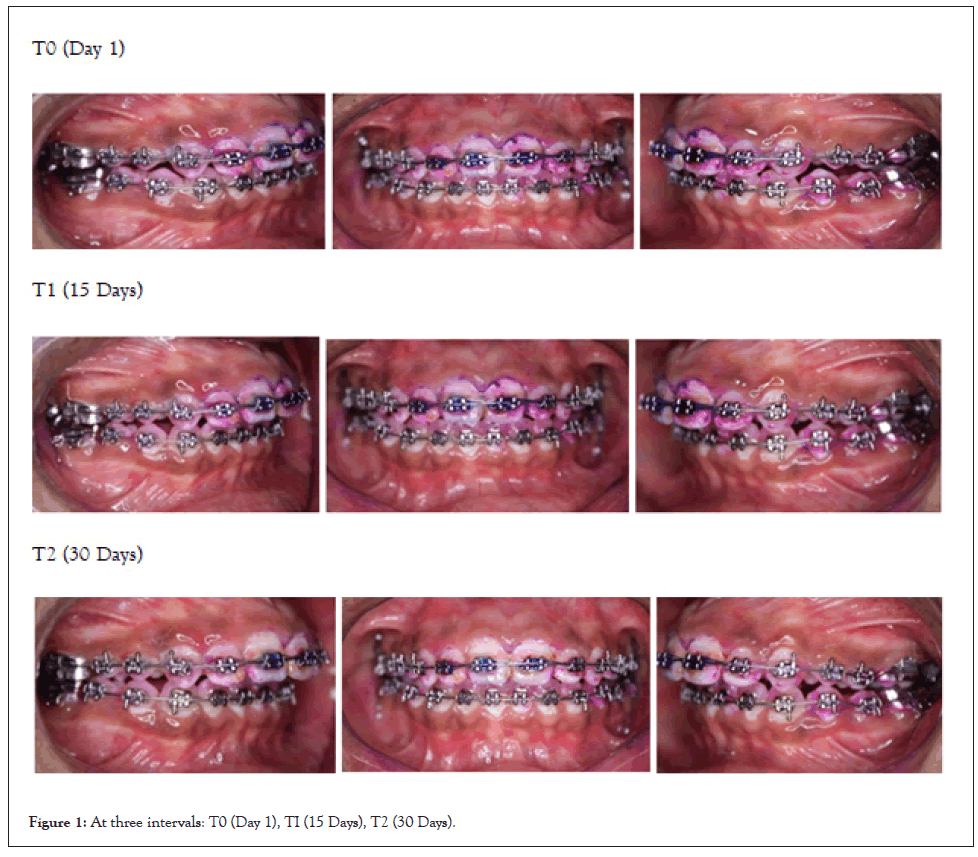
Figure 1: At three intervals: T0 (Day 1), TI (15 Days), T2 (30 Days).
Patient’s adherence to oral home care can be improved through encouragement, education, and motivation as well as ongoing reinforcement. Particularly orthodontic patients need to learn how to maintain good oral hygiene, and their brushing habits need to be regularly observed. A high grade of oral health behaviour can be attained and maintained after a period of rigorous individual oral hygiene education [23]. It is evident from an evaluation of the brushing techniques utilised that patients need encouragement and training to employ the proper technique. Previously, patients undergoing orthodontic treatment were advised to use the so-called "scrubbing method," but the modified Bass technique proved more effective [24]. Many patients neglect the gingival third of the tooth by placing the toothbrush too far coronally, which can result in increased plaque buildup and the onset of gingivitis. As a result, all patients should be given instructions on how to properly clean both the residual coronal surfaces as well as the tooth structure cervical to an orthodontic appliance. Some patients might find it challenging to maintain everyday oral hygiene while wearing orthodontic appliance. Therefore, those who have orthodontic gear should brush their teeth with an electric toothbrush. Indeed came to the conclusion that using an electric toothbrush may be advantageous for people with poor oral hygiene, particularly because dental plaque can be eliminated rapidly and easily. In comparison to manual toothbrushes, electric toothbrushes with rotational brushes are substantially more successful at eliminating supragingival plaque from bracketed teeth. In fact, it was found that variations in plaque-removing efficiency were particularly dependable on the proximal surfaces of teeth [25]. The majority of patients (68%) who had orthodontic treatment did not see a dental hygienist, according to the study's findings. It has been demonstrated that patients with fixed orthodontic appliances respond well to professional prophylaxis [26]. As a result, oral hygiene education and reinforcement are necessary during orthodontic treatment. Reminding some patients to brush their teeth's cervical regions beneath brackets is also necessary. In addition to decreasing the frequency and severity of iatrogenic tissue damage, greater oral hygiene knowledge will also lengthen the long-term advantages of orthodontic treatment [27]. The mean GBI value was reduced from 1.0 to 0.3, which is regarded as a reasonable value. The results of this study revealed that the relationship between the three indices and gender was not significant for the PI and OPI, but significant for the GBI (p=0.05) [28].
Conclusion
The results of this study show that people wearing orthodontic appliances have trouble keeping up decent oral hygiene. Therefore, the key to attaining the best outcomes in oral hygiene continues to be motivating and educating these patients to maintain their oral health as well as suggesting oral home care aids to increase compliance. Patients need to be aware of what to expect from their treatment and what they are responsible for. They must comprehend that they are involved in their orthodontic care as partners and that they have the chance to maintain and then improve their oral health. However, no oral hygiene campaign will be successful unless orthodontists take ownership of inspiring their patients and team. Patients typically respond favourably and are open to self-improvement when an orthodontist delivers oral hygiene recommendations with real interest and respect. Therefore, any hygiene issues or limitations discovered during orthodontic treatment must not be ignored and must be addressed right away.
Clinical significance: Inadequate oral home care among orthodontic patients may increase their risk of gingivitis during orthodontic treatment. It is therefore critical that proper oral hygiene be maintained throughout orthodontic treatment.
References
- Zachrisson SI, Zachrisson BU. Gingival condition associated with orthodontic treatment. Angle Orthod. 1972;42(1):26-34.
[Crossref] [Google Scholar] [pubmed]
- Leggott PJ, Boyd RL, Quinn RS, Eakle WS, Chambers DW. Gingival disease patterns during fixed orthodontic therapy-adolescents vs. adults. J Dent Res. 1984;1(63):309).
- Huser MC, Baehni PC, Lang R. Effects of orthodontic bands on microbiologic and clinical parameters. Am J Orthod Dentofacial Orthop. 1990;97(3):213-218.
[Crossref] [Google Scholar] [pubmed]
- Zachrisson Bu, Alnaes l. Periodontal condition in orthodontically treated and untreated individuals I. Loss of attachment, gingival pocket depth and clinical crown height. Angle Orthod. 1973;43(4):402-11.
[Crossref] [Google Scholar] [pubmed]
- Chang HS, Walsh LJ, Freer TJ. The effect of orthodontic treatment on salivary flow, ph, buffer capacity, and levels of mutans streptococci and lacto bacilli. Aust Orthod J. 1999;15(4):229-234.
[Google Scholar] [pubmed]
- Paolantonio M, Pedrazzoli V, di Murro C, di Placido G, Picciani C, Catamo G, et al. Clinical significance of Actinobacillus actinomycetemcomitans in young individuals during orthodontic treatment. J Clin Periodontol. 1997;24(9):610-17.
[Crossref] [Google Scholar] [pubmed]
- Petti S, Barbato E. Effect of orthodontic therapy with fixed and removable appliances on oral microbiota: a six-month longitudinal study. New Microbiol. 1997;20(1):55-62.
- Manschot A. Orthodontics and inadequate oral hygiene compliance as a combined cause of localized gingival recession: a case report. Quintessence Int. 1991;22(11):572.
- Parker HB. Our common enemy. J Am Soc Prev Dent. 1971; 1(2):14-7.
- Axelsson P. Needs-related plaque control measures based on risk prediction. Inproceedings of the European workshop on mechanical plaque control. Chicago, IL: Quintessence. 1998.
- Zhao H, Xie Y, Meng H. Effect of fixed appliance on periodontal status of patients with malocclusion. Chinese J Stomatol. 2000;35(4):286-288. [Crossref]
- O'LEARY TJ. The plaque control record. J periodontol.1972;43:38.
[Crossref] [Google Scholar] [pubmed]
- Ainamo J, Bay I. Problems and proposals for recording gingivitis and plaque. Int Dent J. 1975;25(4):229-235.
[Google Scholar] [pubmed]
- Heintze SD, Jost-Brinkmann PG, Finke C, Miethke RR. Ortho-plaque Index. In: Oral health for the orthodontic patient. Chicago: Quintessence.1999.
- Loe H, Theilade E, Jensen SB. Experimental gingivitis in man. J Periodontol. 1965; 36: 177-187
- Bloom RH, Brown LR. A study of the effects of orthodontic appliances on the oral microbial flora. Oral Surg Oral Med Oral Pathol. 1964;17(5):658-67.
- Diamanti‐Kipioti A, Gusberti FA, Lang NP. Clinical and microbiological effects of fixed orthodontic appliances. J Clin Periodontol. 1987; 14(6):326-33.
- Listgarten MA, Helldén L. Relative distribution of bacteria at clinically healthy and periodontally diseased sites in humans. J Clin Periodontol. 1978; 5(2):115-32.
- Buckley L. The relationship between malocclusion and periodontal disease. J Periodontol. 1972;43(7):415-7.
- Geiger AM, Wasserman BH, Turgeon LR. Relationship of occlusion and periodontal disease. Relationship of crowding and spacing to periodontal destruction and gingival inflammation. J Periodontol. 1974; 45(1):43-9.
- Lundstrom F, Hamp SE, Nyman S. Systematic plaque control in children undergoing long-term orthodontic treatment. Eur J Orthod. 1979; 2(1):27-39.
- Hamp SE, Lundstrom F, Nyman S. Periodontal conditions in adolescents subjected to multiband orthodontic treatment with controlled oral hygiene. Eur J Orthod. 1982; 4(2):77-86.
- Wites M, Panuszka J, Dyras M. Evaluation of oral and orthodontic appliance hygiene in orthodontically treated patients. Przegl Lek. 2003; 60(6):126-128.
- Waerhaug J. The interdental brush and its place in operative and crown and bridge dentistry. J Oral Rehabil. 1976; 3(2):107-13.
- Bjorn H, Lindhe J. On the mechanics of tooth brushing. Odontol Revy. 1966; 17(1):9-16.
- Trombeli L, Scabbia A, Griselli A, Zangari F, Calura G. Clinical evaluation of plaque removal by counterrotational electric toothbrush in orthodontic patients. Quintessence Int. 1995; 26(3):199-202.
- Alstad S, Zachrisson BU. Longitudinal study of periodontal condition associated with orthodontic treatment in adolescents. Am J Orthod. 1979; 76(3):277-86.
- Carlsson J, Egelberg J. Effect of diet on early plaque formation in man. Odontol Revy. 1965; 16:112-25.
Citation: Yadav J (2023) Oral Hygiene Status: The Critical Parameter in Orthodontic Patients. J Clin Res Bioeth.14:466.
Copyright: © 2023 Yadav J. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

