Indexed In
- Open J Gate
- Genamics JournalSeek
- ResearchBible
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
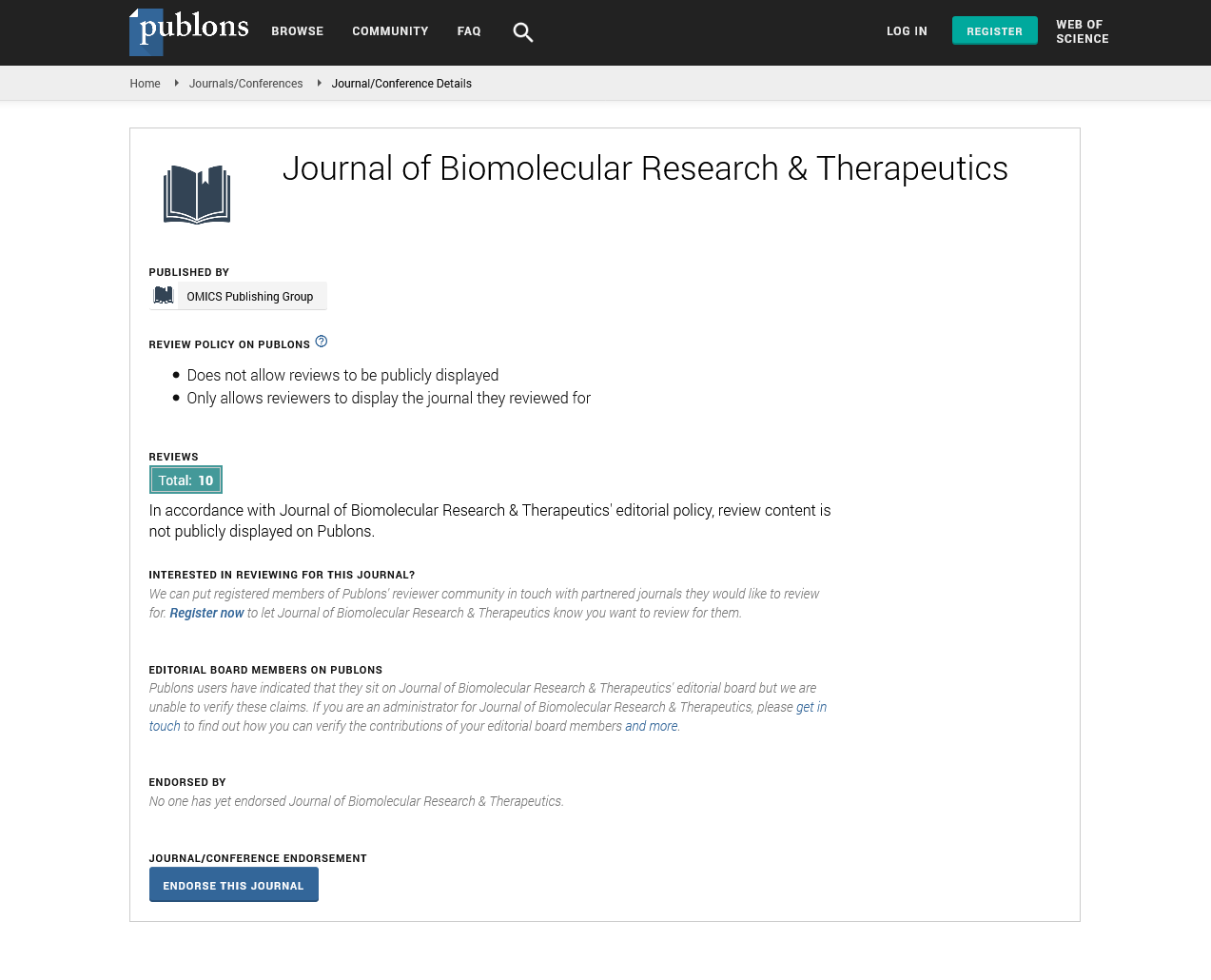
- Publons
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Perspective - (2025) Volume 14, Issue 2
Nanoparticle-Based Drug Delivery in Therapeutic Development
James Wilson*Received: 28-Mar-2025, Manuscript No. BOM-25-29595; Editor assigned: 31-Mar-2025, Pre QC No. BOM-25-29595; Reviewed: 14-Apr-2025, QC No. BOM-25-29595; Revised: 19-Apr-2025, Manuscript No. BOM-25-29595; Published: 28-Apr-2025, DOI: 10.35248/2167-7956.25.14.433
Description
Nanoparticle-based drug delivery has gained substantial attention in biomedical research due to its ability to improve therapeutic efficacy while reducing side effects. Traditional drug formulations often face challenges such as poor solubility, rapid metabolism and off-target distribution. Nanoparticles address these limitations by offering carriers that protect active ingredients, control release and direct drugs to specific tissues. Various types of nanoparticles including liposomes, polymeric nanoparticles and inorganic particles are being investigated for therapeutic delivery. Liposomes have been widely used to encapsulate chemotherapeutic agents, allowing for reduced toxicity and improved accumulation in tumor tissues. Polymeric nanoparticles provide customizable platforms that can incorporate different drugs and release them under controlled conditions. Inorganic nanoparticles such as gold or silica-based particles are also being developed for both therapeutic and diagnostic applications.
Targeted delivery remains one of the greatest advantages of nanoparticles. By attaching ligands or antibodies to nanoparticle surfaces, drugs can be directed to cells expressing specific receptors. This enhances drug accumulation at disease sites while sparing healthy tissues from exposure. Such strategies are particularly valuable in cancer treatment, where precision targeting can significantly reduce adverse effects associated with chemotherapy. Nanoparticles also offer opportunities for crossing biological barriers that limit traditional drug delivery. For instance, the blood-brain barrier has historically restricted treatment of neurological diseases. Engineered nanoparticles with specific properties can traverse this barrier and deliver drugs directly to affected brain regions. This innovation holds promise for treating conditions such as Alzheimer’s disease and brain tumors.
Despite the advantages, nanoparticle-based drug delivery faces challenges in terms of safety and scalability. The long-term effects of nanoparticles in the human body remain under investigation and potential toxicity must be carefully evaluated. Moreover, manufacturing nanoparticles with consistent quality and at large scale presents technical difficulties that limit widespread adoption. Regulatory approval of nanoparticle formulations requires rigorous testing to demonstrate safety and efficacy. A few nanoparticle-based therapies have already reached the market, showing that these challenges can be overcome. Continued collaboration between researchers, clinicians and industry partners is essential to translate promising laboratory findings into clinical applications.
Moreover, the field of stimuli-responsive nanoparticles is emerging as a promising direction for controlled drug release. These smart systems respond to environmental triggers such as pH, temperature, enzymes, or light, enabling site-specific drug activation. For instance, in tumor environments with lower pH, pH-sensitive nanoparticles can release their therapeutic payload selectively, minimizing systemic exposure and enhancing local efficacy. Combination therapies are another exciting application. Nanoparticles can be designed to carry multiple drugs with synergistic effects, enabling concurrent delivery of chemotherapeutics and immunomodulatory, for example. This co-delivery approach can enhance therapeutic outcomes, reduce resistance and improve patient compliance.
Theranostic nanoparticles, which combine therapeutic and diagnostic functions, are also under active development. These systems can deliver drugs while simultaneously enabling real-time imaging or monitoring of treatment response through MRI, PET, or fluorescence. Such integrated platforms offer a personalized approach to disease management, particularly in oncology and chronic conditions. The evolution of biodegradable and biocompatible materials for nanoparticle construction has further improved safety profiles. Natural polymers like chitosan, alginate and hyaluronic acid are gaining interest due to their low toxicity and immune compatibility. These materials degrade into harmless byproducts after drug delivery, reducing the risk of long-term accumulation in tissues.
Looking ahead, nanovaccines which use nanoparticles as carriers for antigens are gaining attention in infectious disease prevention and cancer immunotherapy. These systems can enhance immune activation by presenting antigens in a highly immunogenic format and delivering them to antigen-presenting cells more efficiently. In conclusion, nanoparticle-based drug delivery systems are revolutionizing modern medicine by offering precise, efficient and adaptable solutions to drug administration challenges. While hurdles in toxicity, production and regulation persist, ongoing research and technological advancements are steadily overcoming these limitations. With the convergence of nanotechnology, materials science and biomedical innovation, nanoparticles are set to play a central role in the development of next-generation therapeutics.
Furthermore, the integration of personalized medicine with nanoparticle technologies is expected to tailor treatments based on individual patient profiles. By engineering nanoparticles to match genetic or molecular markers, clinicians can design therapies with enhanced specificity and minimal side effects. In addition, the use of real-time tracking and monitoring of nanoparticle distribution through advanced imaging techniques will allow for better assessment of therapeutic outcomes, improving clinical decision-making. As these technologies mature, nanoparticle-based systems will not only transform how drugs are delivered, but also how diseases are diagnosed, monitored and managed in a highly individualized manner.
Citation: Wilson J (2025). Nanoparticle-Based Drug Delivery in Therapeutic Development. 14.433
Copyright: © 2025 Wilson J. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited