Indexed In
- Open J Gate
- Genamics JournalSeek
- ResearchBible
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research - (2020) Volume 9, Issue 2
Molecular Mechanisms of Angiotensin-converting Enzyme Inhibitory Peptide LAP Activity on Apoptosis of Vascular Smooth Muscle
Yi Shen1, Hong Fang2*, Abdurrahman Omer Cavdar2 and Chi Liu32Department of Cardiology, Tongji Hospital, School of Medicine, Tongji University, Shanghai 200065, China
3Department of Geriatrics, Jingan District Central Hospital, Shanghai 200040, China
Received: 07-Mar-2019 Published: 31-May-2019, DOI: 10.35248/2167-7956.19.8.178
Abstract
We observe the expression levels of apoptotic cells, Bcl-2/Bax and caspase-9 on abdominal aorta of spontaneously hypertensive rats (SHRs) to investigate impact and mechanisms of angiotensin converting enzyme inhibitory peptide LAP in apoptosis of vascular smooth muscle cell. A total of 20 male SHRs were studied to detect apoptotic cells and the expression of apoptosis-related proteins (Bcl-2, Bax, caspase-9). The index of apoptotic cells in LAP group was significantly lower compared to the control group. The expression of Bcl-2 in the LAP group was significantly higher than the control group. However, the levels of Bax and caspase-9 expression in the LAP group were significantly lower compared to the control group. The apoptosis index was negatively correlated with Bcl-2 and positively correlated with Bax/caspase-9. Similarly, the inflammation markers in LAP group were significantly lower than those in the control group. The expression of Ang II was significantly decreased after treating with LAP in the abdominal arteries. Angiotensin- converting- enzyme inhibition peptide LAP inhibited apoptosis of vascular smooth muscle cells through up-regulation of Bcl-2 and down-regulation of Bax and caspase-9 in SHRs.
Keywords
Apoptosis; Vascular smooth muscle cell; Angiotensin- converting enzyme- inhibitory peptides
Introduction
Essential hypertension is an important cause and risk factor of cardiovascular and cerebrovascular diseases. It can affect the structure and function of important organs and seriously impact human health. With the development of the studies related to cardiovascular diseases, vascular remodelling has recently been proposed to be one of the most important mechanisms. Vascular remodelling with adaptive changes of hemodynamic or humoral factors is the pathophysiological basis of complications of hypertension. The major pathological manifestations in vascular remodelling were imbalance between cell proliferation, apoptosis of vascular smooth muscle cells and deposition of extracellular matrix [1]. These are important pathological changes of hypertension, and results in a continued deterioration in the structural basis of hypertension. The vascular structure remodelling including the regression of vascular hypertrophy is now being considered as a key therapeutic target in an effort to reduce mortality and morbidity associated with high blood pressure [2]. The Renin-angiotensin system (RAS) is one of the important factors in causing vascular remodelling. Angiotensin II, a component of the renin-angiotensin-aldosterone system, has been reported to be associated with the pathophysiology of vascular remodelling in hypertensive patients. Recently, several studies confirmed that a high level of Angiotensin II in local tissue would lead to an imbalance between apoptosis and proliferation of vascular smooth muscle cells, which may be one of the mechanisms of hypertensive vascular remodelling [3-5]. At present, many researchers have focused on the dietary prevention of development of hypertension. They have a particular interest in the biological activity of peptides and proteins derived from nature. ACE inhibitory peptides have been shown to inhibit ACE but they have small side effects. The ACE inhibitory peptide LAP which was purified Leu-Arg-Pro-Val-Ala-Ala from bovine lactoferrin (bLf) possesses several physiological functions. A previous study suggested that peptide LAP possesses antihypertensive activity and improves vascular remodelling [5]. But it is unclear if it really affects apoptosis of smooth muscle cells in the vascular remodelling process or not. The molecular mechanism associated with apoptosis of smooth muscle cells in the vascular remodelling process remains relatively unexplored. Therefore, the effects and molecular mechanisms of peptide LAP upon apoptosis in the vascular remodelling process were investigated in this study.
Materials and Methods
Animal experiments
A cohort study of spontaneous hypertensive rats (SHRs) aged ≥ 10 weeks, with a body weight of 220-240 g, was obtained from the Animal Centre of second Military Medical University. SHRs, an animal model of genetic hypertension that allows us to study essential hypertension, were maintained in an air-conditioned room (25 ± 1°C) and kept on a 12-hour light/12-hour dark cycle (lights on at 06:00 h). Food and water were available ad libitum. All animal procedures were performed according to the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health as well as the guidelines of the Animal Welfare Act [5,6]. The rats were randomized to one of two groups: control group and the experimental group. In each group, the same dose of LAP (experimental group) or saline (control group) was intraperitoneally injected into SHRs at weeks 0, 4, 8, 10, and 12 (total 5 times). The desired concentration of LAP was 50 g per rat. In the beginning and at the end of the experiment, 0.3 - 0.5 ml of blood was collected by cardiac puncture sampling technique to assess serum Interleukin-6 (IL-6) and tumour necrosis factor alpha (TNF-α ) levels [6].
Abdominal aortic media measurement: Serial transverse abdominal aorta sections cut from each paraffin block, stained with HE, were subjected to media morphometry assessment. The media thickness was determined by measuring 4 regions of a section divided by a cross and recorded in micrometers under a regular microscope (Olympus, Japan) (× 100–400). Photos were taken and were analyzed with a computer-aided image analysis system (LEICA QWin V3) [6].
Apoptotic cells were observed by TUNEL method: After quenching endogenous peroxidase, serial sections of the transverse abdominal aorta were incubated with fluorescein-12-dUTP and immersed in propidium iodide. Sections in each group with stochastic choice were then viewed under a fluorescence microscope. The percentage of TUNEL-positive cells in each section was assessed in five randomly selected fields.
Serum inflammatory biomarker assessment
ELISA enabled simultaneous detection of IL-6 and TNF-α using an MSD Sector Imager 2400 reader.
Bcl-2/Bax, caspase-9 and Ang II expression analysis
Equal amounts of total protein from SHR vascular homogenates were separated by Sodium Dodecyl Sulphate Polyacrylamide Gel Electrophoresis (SDS-PAGE). After transferring, membranes were blocked with blocking buffer for 1 h at room temperature. Membranes were then incubated with mouse anti-mouse Anti- Ang II antibodies overnight at 4°C, followed by incubation with horseradish peroxidase-labeled secondary antibodies for 2 h. Finally, signals were detected by enhanced chemiluminescence.
Statistical analysis
All the measurement data is represented by means ± SD and data obtained were analyzed using t-test and Pearson correlation with SPSS software 13.0. Differences were considered significant if p<0.05.
Results
Abdominal aortic media
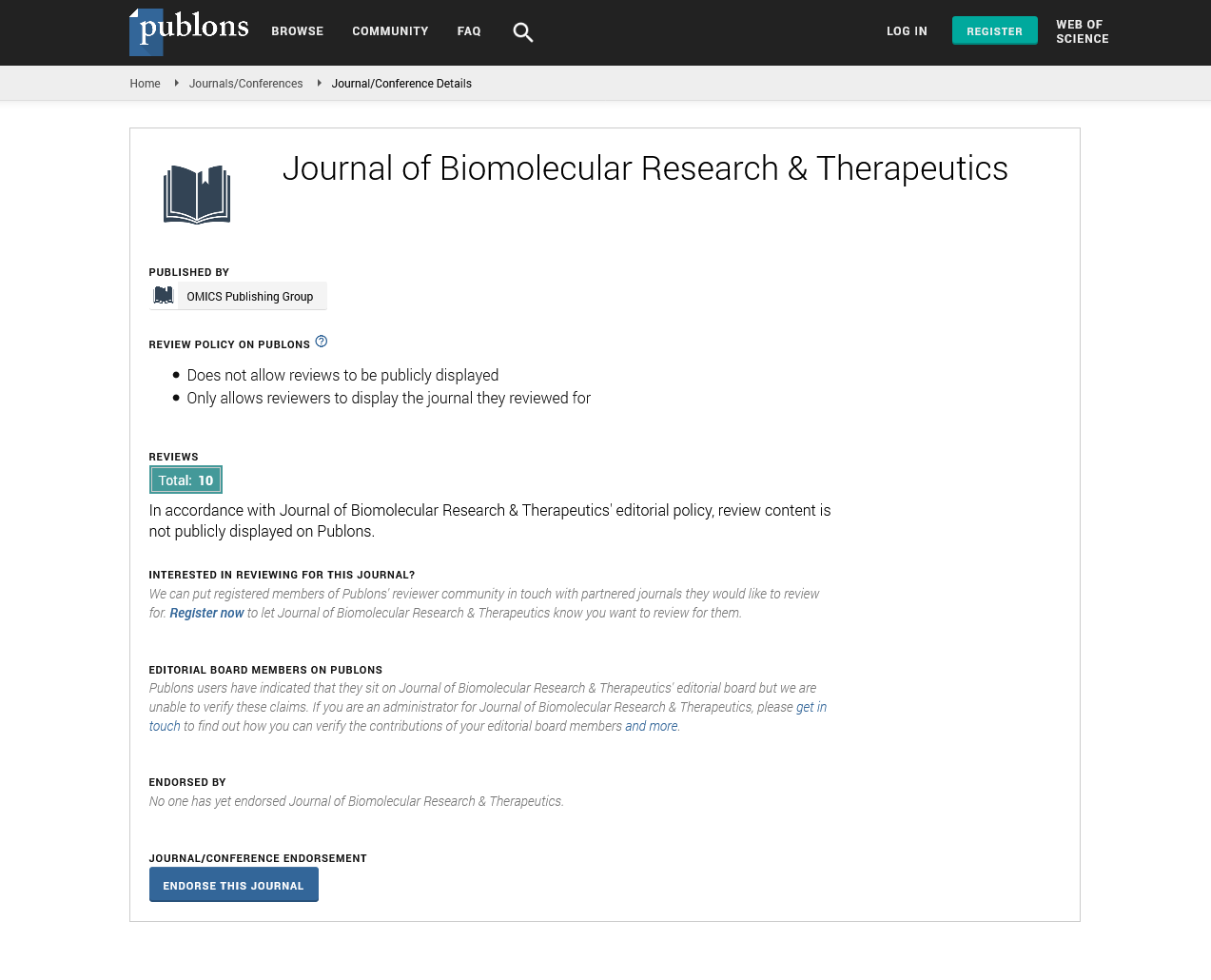
At the end of the experiment, the vascular media thickness in the LAP group decreased. The difference between the LAP group and control group is significant (Figure 1A-C).
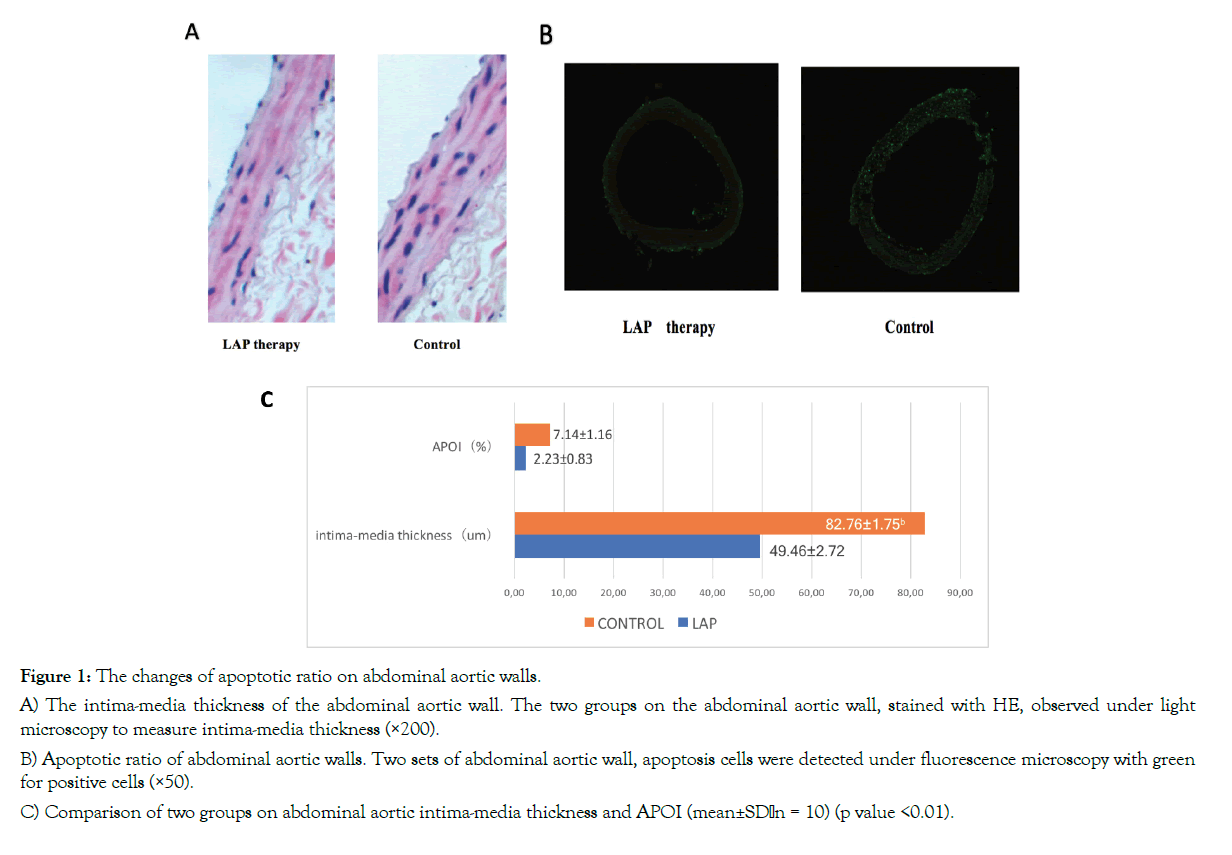
Figure 1: The changes of apoptotic ratio on abdominal aortic walls.
A) The intima-media thickness of the abdominal aortic wall. The two groups on the abdominal aortic wall, stained with HE, observed under light microscopy to measure intima-media thickness (×200).
B) Apoptotic ratio of abdominal aortic walls. Two sets of abdominal aortic wall, apoptosis cells were detected under fluorescence microscopy with green for positive cells (×50).
C) Comparison of two groups on abdominal aortic intima-media thickness and APOI (mean±SD,n = 10) (p value <0.01).
The changes of apoptotic ratio on abdominal aortic walls
Apoptotic ratio of abdominal aortic walls in LAP group showed a significant difference compared to the control group. There was a significant decrease in apoptotic cells in the LAP group (Figure 1B and C).
The expression of Bcl-2/Bax and Caspase-9
The positive cells including Bcl-2 in LAP group were significantly higher whereas Bax and Caspase-9 in LAP group were significantly lower than the ones in the control group (Figure 2A and B).
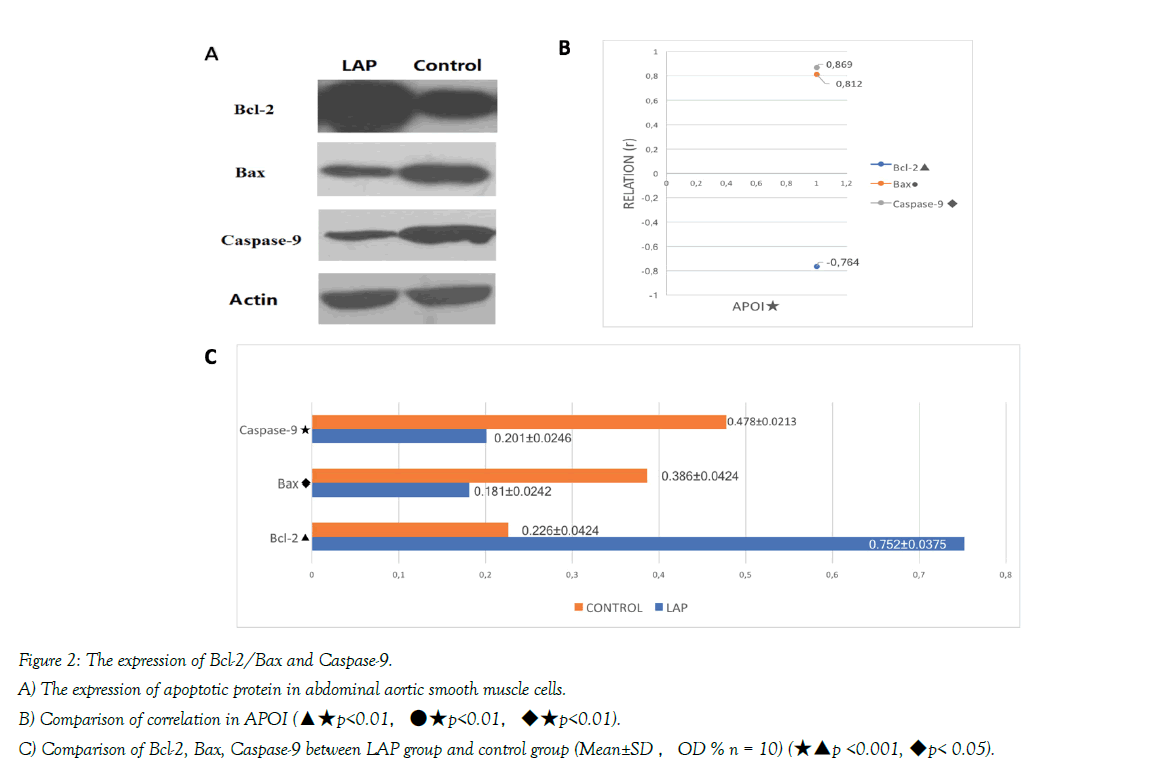
Figure 2: The expression of Bcl-2/Bax and Caspase-9.
A) The expression of apoptotic protein in abdominal aortic smooth muscle cells.
B) Comparison of correlation in APOI (▲★p<0.01,●★p<0.01,◆★p<0.01).
C) Comparison of Bcl-2, Bax, Caspase-9 between LAP group and control group (Mean±SD ,OD % n = 10) (★▲p <0.001, ◆p< 0.05).
The correlation analysis of apoptotic index and Bcl-2/Bax and caspase-9
The correlation analysis between APOI and Bcl-2/Bax, Caspase-9 demonstrated that APOI was negatively correlated to Bcl-2, but positively correlated to Bax. APOI and Caspase-9 showed a positive correlation Figure 2B and C.
Serum biomarker assessment
In samples collected from the periphery, TNF-α and IL-6 were significantly different between the two groups. The inflammation markers in LAP group were significantly lower than those in the control group Figure 3.
Figure 3: Comparison of TNF-α, IL-6 between LAP group and control group in Peripheral Serum Samples (unit: pg/mL n = 10) (★p < 0.001, ▲p <0.05).
The expression of Ang II in abdominal aortic wall
To assess the possible mechanisms of inflammation-induced vascular fibrosis, we evaluated the effects of inflammation on the protein expression of Ang II in the arteries. At the vascular level, the expression of these proteins were assessed by Western Blotting Analysis shown in Figure 4A. The results demonstrated that the expression of Ang II was significantly decreased after treating with LAP in the abdominal arteries Figure 4B.
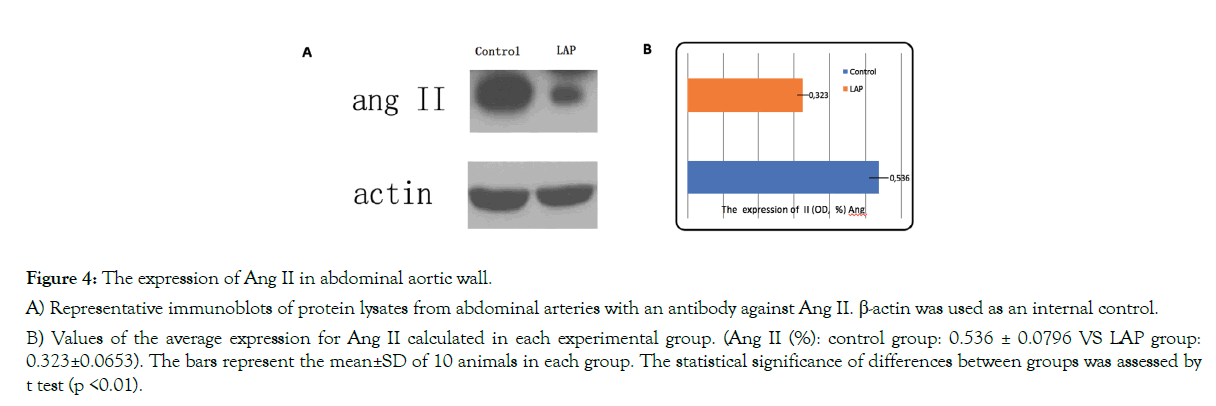
Figure 4: The expression of Ang II in abdominal aortic wall.
A) Representative immunoblots of protein lysates from abdominal arteries with an antibody against Ang II. β-actin was used as an internal control.
B) Values of the average expression for Ang II calculated in each experimental group. (Ang II (%): control group: 0.536 ± 0.0796 VS LAP group: 0.323±0.0653). The bars represent the mean±SD of 10 animals in each group. The statistical significance of differences between groups was assessed by t test (p <0.01).
Discussion
Growth, apoptosis, inflammation, and fibrosis contribute to vascular remodelling in hypertension. Apoptosis has been reported in hypertension to be both increased and decreased in different tissues, including blood vessels [5,7]. In recent years, the apoptotic process has emerged as an important mechanism of cardiovascular remodelling. Vascular smooth muscle cell (VSMC) within vessel walls can both divide and undergo apoptosis throughout the life. In diseased tissues, additional factors are present both locally, such as inflammatory cytokines, inflammatory cells, and so on. These factors substantially alter the normal balance of proliferation and apoptosis. Apoptosis of blood vessels may contribute to vascular remodelling [8]. Inflammation which may be low grade could play an important role in triggering apoptosis in hypertension. The findings in our studies showed that TNF- α in sample collected from the periphery were significantly different between the two groups. The level of inflammatory cytokines in the LAP group was significantly lower than those in the control group. The result indicated that the effect of LAP was anti-apoptosis through the inhibition of inflammation. The regulation of apoptosis can be simplified into two major pathways. The first pathway is apoptosis via membrane death receptors of the tumor necrosis receptor (TNF) family. The second pathway is via mitochondrial amplification. Bcl-2 family members that promote cell survival include Bcl-2 and the long form of Bcl-X, whereas Bax and Bad function to promote apoptosis. Numerous studies have examined the role of Bcl-2 family proteins in controlling vascular cell viability. Bax expression was elevated in VSMCs where high frequencies of apoptosis were observed. In SHR arteries, the Bax/Bcl-2 ratio was reduced, which suggested decreased apoptosis [9]. Vascular remodelling and vessel regression are associated with down-regulation of Bax expression in VSMCs [7,10-14]. Apoptosis is a complex, caspase-mediated protease cascade reaction process. Caspase-9 is located upstream of the caspase cascade. The apoptotic starting signal in mitochondria, ultimately induces caspase-9 to activate self-catalytic activity, which further activates downstream caspases and caspase-3. Differential proteolysis of the caspase-3 protease zymogen into two or caspase-3 activates caspase-3, and results in further cutting in the type of substrate that causes the protease cascade cutting cascade. This ultimately causes apoptosis [1,6,12,13]. A series of studies have provided convincing evidences suggesting that Ang II induces the apoptosis of VSMCs. VSMCs within vessel wall can both divide and undergo apoptosis throughout one’s life. Ang II can induce apoptosis of VSMCs by acting via AT1 receptors. Inhibiting apoptosis with ACEI decreases Ang II receptor stimulation due to the inhibition of Ang II formation. Together with apoptosis, proliferation and migration of VSMC, these are vital in the pathogenesis of vascular remodeling. In animal models, ACE inhibitors have been demonstrated to ameliorate organ damage by diminishing the inflammatory response, cell proliferation and fibrosis. Despite the widespread use of these agents in clinical practice, they have some side effects. Therefore, development of the safer ACE inhibitors has been a major focus within scientific research recently. Thus, studies should focus on the ACE inhibitory peptides derived from food proteins. ACE inhibitory peptides from nature can inhibit ACE with greater safety, also diminishing side effects, etc. Moreover, some of them have been shown to possess antihypertensive activity against established hypertension in animals or in humans. Lactoferrin (Lf), an iron-binding glycoprotein of the transferrin family, exists in many biologic fluids including milk, saliva, tears, mucous fluid and blood. Lf consists of a single polypeptide chain having a molecular mass of about 80 kDa. A study by Ming showed that ACE inhibitory peptide LAP purified from bLf possessed antihypertensive activity and improved vascular remodeling [6]. Currently, we found that LAP decreased VSMC apoptosis, which was evidenced by an increase in the Bcl-2 to Bax ratio, an accumulation of TUNEL-positive nuclei, as well as a decrease in SMC number and vascular DNA content. Our results demonstrated that treatment with LAP within this critical period prevented the effects of Ang II on aortic remodeling, which includes reduced caspase-9–like enzymatic activity, SMC depletion and aortic mass reduction. At the end of the experimental intervention, immunohistochemistry detection of Bcl-2/Bax and caspase-9 expression in the abdominal aorta of SHRs showed up-regulated Bcl-2 while Caspase-9 and Bax were down-regulated compared to the control group. There were significant differences in observed apoptotic cells by the TUNEL method. The apoptotic index in the LAP group was significantly lower compared to the control group.
Conclusion
The data from our studies confirmed that hypertensive vascular remodeling can be improved by inhibition of vascular smooth muscle apoptosis. Angiotensin-converting enzyme inhibitory peptide LAP can reduce Ang II and then up-regulate Bcl-2, while also down-regulating the expression of Bax and caspase-9 to inhibit apoptosis. Those findings indicated that Angiotensin-converting enzyme inhibitory peptide LAP may improve vascular remodeling through inhibiting apoptosis to protect the target organ from damage caused by hypertension.
Limitation
In this study, the experimental period was short. Although results are promising, Experimental period should be longer to explain the long-term effects of Angiotensin-converting enzyme inhibitory peptide LAP on vascular structures for more intensive studies in the future.
Ethics Approval
This study was conducted with the Approval of the Medical ethic committee in Shanghai Tongji Hospital. (No: 2014-DW-024).
REFERENCES
- Chen C, Wang Z, Wang L, Yang L, Ding M, Ding C, et al. Puerarin induces mitochondria-dependent apoptosis in hypoxic human pulmonary arterial smooth muscle cells. PLoS One. 2012;7:e34181.
- Chen J, Chen W, Zhu M, Zhu Y, Yin H, Tan Z, et al. Propofol attenuates angiotensin II-induced apoptosis in human coronary artery endothelial cells. Br J Anaesth. 2011;107:525-532.
- deBlois D, Tea BS, Than VD, Tremblay J, Hamet P. Smooth muscle apoptosis during vascular regression in spontaneously hypertensive rats. Hypertension. 1997;29:340-349.
- Hong F, Min L, Yi S, Zhanxia L, Yongquan W, Chi L, et al. The antihypertensive effect of peptides: a novel alternative to drugs. Peptides. 2008;29:1062-1071.
- Ihling C, Szombathy T, Nampoothiri K, Haendeler J, Beyersdorf F, Uhl M, et al. Cystic medial degeneration of the aorta is associated with p53 accumulation, Bax upregulation, apoptotic cell death, and cell proliferation. Heart. 1999;82:286-293.
- Ming L, Yi S, Chi L, Zheng H, Li Z, Deng Y, et al. Long-term antihypertensive effect of angiotensin-converting enzyme inhibitory peptide LAP. Kidney Blood Press Res. 2011;34:358-364.
- Madeo F, Fröhlich E, Fröhlich KU. A yeast mutant showing diagnostic markers of early and late apoptosis. J Cell Biol. 1997;139:729-734.
- Marchand EL, Der Sarkissian S, Hamet P, deBlois D. Caspase-dependent cell death mediates the early phase of aortic hypertrophy regression in losartan-treated spontaneously hypertensive rats. Circ Res. 2003;92:777-784.
- Morris CB, Gendelman R, Marrogi AJ, Lu M, Lockyer JM, Alperin-Lea W, et al. Immunihistochemical detection of Bcl-2 in AIDS-associated and classical Kaposi's sarcoma. Am J Pathol. 1996;148:1055-1063.
- Pandey R, Quan WY, Hong F, Jie SL. Vaccine for hypertension: modulating the renin-angiotensin system. Int J Cardiol. 2009;134:16016-16018.
- Rudijanto A. The role of vascular smooth muscle cells on the pathogenesis of atherosclerosis. Acta Med Indones. 2007;39:86-93.
- Sun J, Zheng J, Ling KH, Zhao K, Xie Z, Li B, et al. Preventing intimal thickening of vein grafts in vein arterybypass using STAT-3 siRNA. J Transl Med. 2012;10:2.
- Touyz RM. Intracellular mechanisms involved in vascular remodelling of resistance arteries in hypertension: role of angiotensin II. Exp Physiol. 2005;90:449-455.
- Walsh K, Smith RC, Kim HS. Vascular cell apoptosis in remodeling, restenosis and plaque rupture. Circ Res 2000;87:184-188.
Citation: Shen Y, Fang H, Cavdar AO, Liu C (2019) Molecular mechanisms of Angiotensin-converting enzyme inhibitory peptide LAP activity on apoptosis of vascular smooth muscle. J Biomol Res Ther 8:178. doi: 10.35248/2167-7956.19.8.178
Copyright: �© 2019 Shen Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.