Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
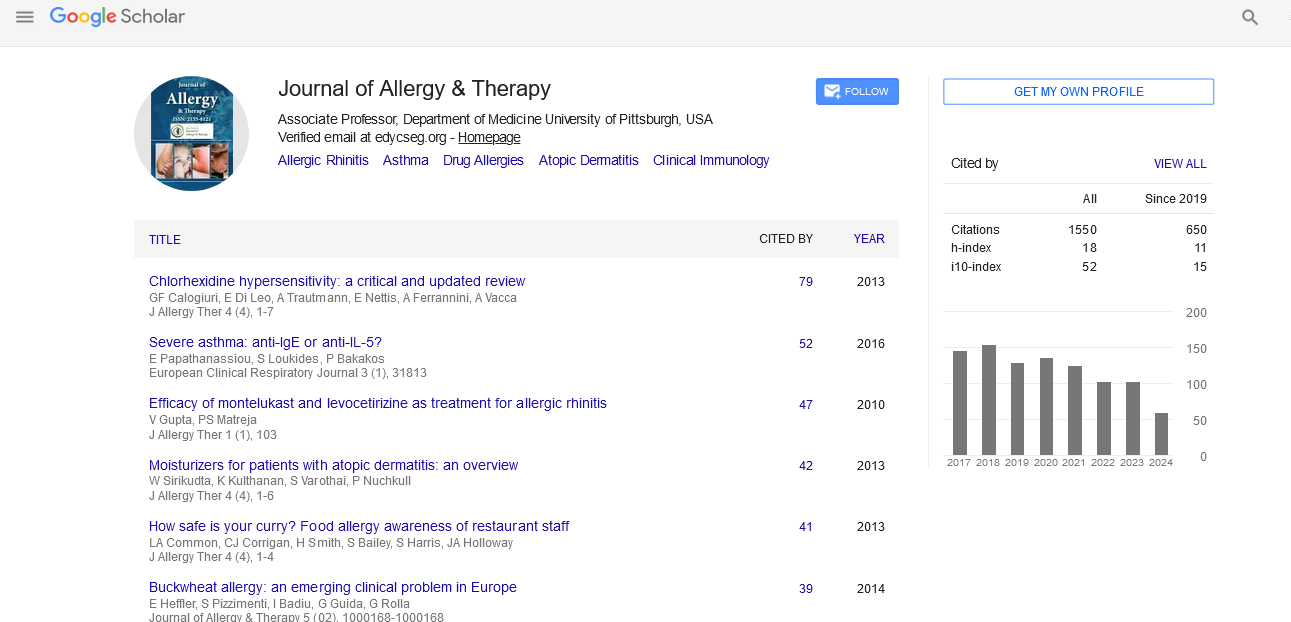
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Perspective - (2023) Volume 14, Issue 2
Methods of Allergic Rhinitis in Predatory and Mechanism of Lower Airway Hyper Responsiveness
Bagheri Matthew*Received: 03-Feb-2023, Manuscript No. JAT-23-20289 ; Editor assigned: 06-Feb-2023, Pre QC No. JAT-23-20289 (PQ); Reviewed: 20-Feb-2023, QC No. JAT-23-20289 ; Revised: 27-Feb-2023, Manuscript No. JAT-23-20289 (R); Published: 06-Mar-2023, DOI: 10.35248/2155-6121.23.14.340
Description
Allergic rhinitis is a common condition that confused many scientists. Lower airway hyper responsiveness occurs in the majority of allergic rhinitis patients and an allergic rhinitis attack can exacerbate this condition. In order to identify the mechanism at play and offer suggestions for future diagnosis, therapy, and experiments, the effects of allergic rhinitis on the lower airways are examined in this paper in terms of epidemiology, anatomy, pathophysiology, nasal function loss, inflammation drainage, nasobronchial reflex, and whole-body circulatory streams.
The connection between the upper and lower airways, which exist as a single morphological and functional unit, has long been recognized in both normal and pathological conditions. From a clinical and physiological perspective, the interaction between the upper airways, which are made up of the two nasal passages and the paranasal sinuses, and the lower airways, which are made up of the bronchi and bronchioles, is of great importance. One should be able to comprehend and visualize the operation of the entire system in order to comprehend illnesses that on the surface seem to just impact one component of a vital organ system. The upper and lower airways' mucosa is continuous, and they have a lot in common anatomically and histologically. Structures including glands, ciliary epithelium, lamina propria, basement membrane, and goblet cells are shared by the two components of the respiratory mucosa, which is made up of pseudostratified ciliated columnar epithelium and the supporting lamina propria. The basement membrane is mostly composed of type 5 laminin and type 4 collagen, and the epithelium is situated above it. The basement membrane serves as a barrier between the epithelium and the underlying mesenchymal components, allowing epithelial and inflammatory cells to move.
Microbes are a key worsening factor in patients with allergic rhinitis, asthma, and atopic dermatitis and can sensitize and develop atopic illness in predisposed individuals. Although Pyroglyphidae mites have been widely examined, very few publications on Cheyletidae spp., particularly with reference to human pulmonary disease, are available. The primary goal of the current investigation is to determine whether this predator mite's (Cheyletus eruditus) clinical role as a respiratory antigen in a particular group of sensitised humans. To determine their eligibility for the trial, 52 adult patients were selected from the outpatient allergy clinic. A positive IgE response to C. eruditus was established by a Skin Prick Test (SPT) in the 37 patients with Persistent Allergic Rhinitis (PAR) who met the Allergic Rhinitis and its Impact on Asthma (ARIA )criteria.
While the bronchial mucosa has many smooth muscle cells, the nasal mucosa has a large number of arteries. When exposed to an inflammatory insult, epithelial cells can quickly mend under normal circumstances. Epithelial shedding, goblet cell metaplasia, basement membrane thickening, extracellular matrix deposition in the submucosa, smooth muscle hypertrophy, subepithelial angiogenesis, and myofibroblast hyperplasia are all consequences of chronic epithelial damage that alters the structural makeup of the airways. The epithelial barrier hypothesis for the pathophysiology of asthma, chronic rhinosinusitis, and allergic rhinitis was developed as a result of the demonstration of leaky epithelial defects in the affected organs of these disorders. Allergen Immunotherapy (AIT) is a curative therapy for allergic conditions including asthma and hay fever that modifies the pathophysiology at the root of the problem, corrects the unbalanced Th2 response, and promotes long-term clinical tolerance against allergens. AIT significantly reduces symptoms and medication consumption, enhances quality of life, and stops the development of new sensitizations. AIT also stops the advancement of asthma that is already present and the development of asthma in people with allergic rhinitis.
Citation: Matthew B (2023) Methods of Allergic Rhinitis in Predatory and Mechanism of Lower Airway Hyper Responsiveness. J Allergy Ther. 14:340.
Copyright: © 2023 Matthew B. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.