Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
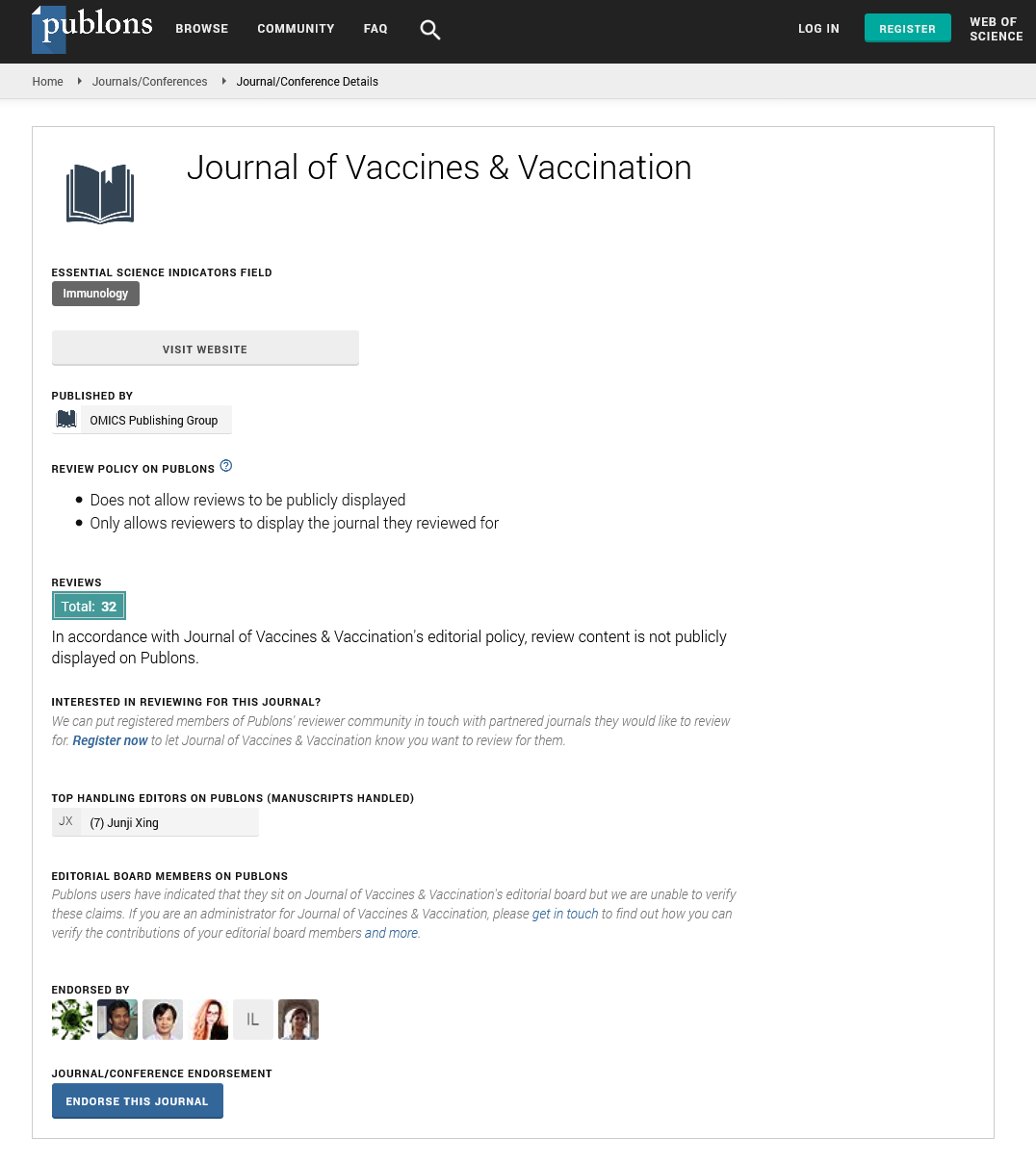
- Publons
- MIAR
- University Grants Commission
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2021) Volume 12, Issue 6
Lack of Trust, Insufficient Knowledge and Risk Denial: An in-Depth Understanding of Health Workers, Barriers to Uptake of the COVID-19 Vaccine in Kampala, Uganda
Lubega Muhamadi1*, Namulema Edith2, Waako James3, Nazarius Mbona Tumwesigye4, Safinah Kisu Museene5, Hellen Mukakaarisa6, Stefan Swartling Peterson7 and Anna Mia Ekstrom72Department of HIV Care, Mengo Hospital, Albert Cook Rd, Kampala, Uganda
3Department of Medicine, Iganga Hospital, Main St, Iganga, Uganda
4School of Public Health, College of Health Sciences, Makerere University, Kampala, Uganda
5Department of Health Education and Training, Ministry of Education and Sports, Kampala, Uganda
6Uganda Nurses and Midwives Examinations Board, Kiwatule, Nakawa Division, Kampala, Uganda
7Department of Global Public Health, Karolinska Institutet, Stockholm, Sweden
Received: 25-Oct-2021 Published: 15-Nov-2021
Abstract
COVID-19 Vaccine hesitancy among health workers remains a major hindrance to the governments vaccine roll out plan among health workers and other target populations in Uganda.
We conducted 12 focus group discussions and 20 in-depth interviews with health workers (vaccinated and unvaccinated) to understand barriers to vaccine acceptance from their own perspective and context in central and eastern Uganda. Reported barriers to vaccine acceptance included: lack of trust, fear of side effects, risk denial and insufficient information about the vaccine amidst negative publicity about the vaccine from the internet and social media platforms. Others were health system inhibition factors and religious beliefs against the vaccine.
We recommend a context specific information, education and dissemination adapted to health workers' needs to create more awareness, and knowledge about the vaccine.
We also recommend a that the government initiates and implements a broad long-term strategy including a sustained media campaign to provide the Ugandan public with updated information and dispel negative publicity and misinformation about the vaccine.
Engaging in dialouge with health workers at all levels of care, use positive peer influence, use of religious and opinion leaders as well as ensuring accessible and safe vaccination posts to could also increase uptake of the vaccine among health workers.
Keywords
Vaccine hesitancy; Health workers; COVID-19
Introduction
Although the government of Uganda continues to receive/procure COVID-19 vaccines for its people, vaccine hesitancy poses a major threat to the government’s rollout plan for vaccination against COVID-19 [1-3]. Uganda with a population of approximately 45 million people targeted to fully vaccinate 22 million people (49.6% of the population) in a phased manner [1,4]. The first phase was anticipated to vaccinate 4.8 million (20%) of the target population between March and June 2021 including; health workers, security personnel, people above 50 years, with underlying co-morbidities, teachers and students aged 18 years and above. However, according to the presidential press release of 22nd September 2021, 81% of the targeted 4.8 million people had not received their first dose, while 91% had not received their second dose of the vaccine [5]. in addition the government also planned to import and administer another estimated twelve million doses of COVID-19 vaccine by December 2021 [4,5].
Health workers who are the most vulnerable frontline staff in the fight against COVID-19 have not fully embraced the vaccination exercise. For example, by the end September 2021, approximately 30% of the health workers in Uganda had not received their first dose and 60% had not received their second dose of COVID-19 vaccine [4-6]. In Mengo hospital, located in the centre of the capital city Kampala, the office of the deputy director estimates that 40%-50% of the hospital's health workers had not yet chosen to be vaccinated despite easy access [7]. Similarly, in Iganga hospital in eastern Uganda approximately 120 kilometres from Kampala, the vaccine uptake rate among health workers was approximately 50% [8]. Health workers are trusted and communities tend to follow their example and health actions almost religiously. Therefore as the government's vaccine roll out plan evolves, the health workers' hesitancy towards vaccine uptake is likely to negatively impact how the willingess to vaccinate against COVID-19 also in the general community.
Why do health workers' are aware of the damage the pandemic had on to their communities colleagues die of COVID-19 refuse to take up the vaccine? A few online surveys and studies conducted before any vaccine against COVD19 was available, have shown that social influence, religious and cultural beliefs, fear of side effects, attitude towards the vaccine and susceptibility to illness are common barriers to uptake of vaccines [9-12]. There is, however, a paucity of information on why health workers in Uganda and other African countries have not fully embraced the COVID-19 vaccine despite having experienced COVID-19 deaths among colleagues, and clients. An in-depth understanding of health workers' perceptions towards this vaccine from their own perspective is therefore vital especially at a time when the Ugandan government is rolling out vaccination to over 20 million people.
Materials and Methods
Study setting and population
In order to get a better an understanding of the health workers' perceptions with regard to the COVID-19 vaccine Mengo and Iganga hospitals. Mengo hospital is a private not for profit entity located city Kampala. The hospital offers both general clinical and specialized services to an urban population of over three million people from the Kampala metropolitan area. The hospital employs over 800 staff consisting of technical, and administrative staff. Iganga is also a designated COVID-19 treatment centres in Kampala offering both general clinical care and supportive treatment to people infected with COVID-19. It also has a High Dependency Unit (HDU) for clients that need high level monitoring and an Intensive Care Unit (ICU) for critical cases. Over the first and second wave of the COVID-19 pandemic in Uganda, the hospital treated over 300 patients with COVID-19 of varying severity. The hospital also serves as a COVID-19 vaccination centre [7]. Iganga hospital is located approximately 120 km east of Kampala. It is a public referral hospital offering both general and specialized services. The hospital is a referral centre for about six districts constituting a population of three million people. Most of the patients live on subsistence farming while 7% live in urban and peri-urban environments. The hospital has approximately 200 staff consisting of clinical, technical and administrative staff. It is one of the designated COVID-19 treatment centres offering general clinical care to people with COVID-19 but also has an HDU. Over the first and second wave of the pandemic in Uganda, the hospital treated over 200 COVID-19 patients with of varying severity, fifteen of whom were health workers. The hospital also serves as a COVID-19 vaccination centre [8,13,14].
This qualitative study employed 12 Focus Group Discussions (FGDs) with health care workers of different cadres and deployment. Six of the FGDs were conducted in Mengo and another six in Iganga hospital. We also conducted 20 In Depth Interviews (IDIs) with health workers from both Mengo and Iganga hospitals 10 of whom had been vaccinated with the COVID-19 vaccine and 10 who had not been vaccinated. The study aimed at exploring possible motivators/barriers for uptake of the vaccine amongst health workers from their own perspective [15,16]. The FGD and IDI respondents were purposively selected based on maximum variety sampling from a sampling frame covering all cadres from specialist health personnel to the support staff to to get a broad variety of viewpoints. The selected respondents were considered to be more “knowledge rich” on the study subject and chosen from consenting staff at in both hospitals. The FGDs were stratified by cadre to encourage more active participation and included a mix of been vaccinated and un-vaccinated to avoid potential stigmatization. Each FGD consisted of a maximum of 12 respondents. The participants were not told how their groups were selected or other participants' vaccination status [15-18].
Data collection tools and methods
Using a topic guide, the selected participants were probed on their knowledge, attitudes and perceptions about the COVID-19 vaccine. Their views on values and norms related to risk/benefit of vaccines and public health interventions, acceptance and uptake of vaccines in general and the COVID-19 vaccine in particular, as well as prevailing common misconceptions and myths about the vaccine were also probed. Interviews were stopped when it was judged that saturation had been reached and no more new information could be retrieved from the respondents. All data collection was supervised and assessed by the first author (LM) who is a male, indigenous public health physician and the second and second last authors (WJ, NE) both of whom are conversant with qualitative research and the health system dynamics at Iganga and Mengo hospitals. Five research assistants conversant with qualitative data collection in the study setting and moderated and took notes were all fluent in Luganda and Lusoga (the local languages). They were trained for two days on the study aim, design and tools. Role-plays were used to prepare the research assistants for their interaction with the informants [17,19,20].
Data management and analysis
All the FGDs and the IDIs were conducted in a mixture of English, Lusoga or Luganda, transcribed and later translated into English by the interviewers. The authors who are conversant in the local languages listened to the audio recordings to confirm the validity of the information. Data collection stopped when information relating to the topic guides revealed no new information. The data analysis was iterative including reviews and discussions at different stages of data collection and appropriate modifications were made in the tools to address emerging issues [18,21]. The units of analysis were the transcripts from the IDIs and the FGDs. Content analysis was used to analyze the transcripts. This entailed reading and reviewing the entire interviews back and forth to identify meaningful units in relation to the research questions [16,20,21]. Meaningful units were condensed and coded by categories and themes, and discussed by (LM, WJ and EN) until consensus was reached [20].
Ethical clearance
The study was approved by the Mengo hospital Research and Ethics Committee (REC) ref MH/REC/39/06-2021, and the Uganda National Council for Science and Technology (UNCST). We also sought the approval from the management of both Mengo and Iganga hospitals. As part of informed consent, participants were thoroughly informed about the aims of the study, the anticipated benefits and risks, their ability to participate or withdraw at any time, and assured that all information obtained would be kept confidential. They signed two copies of the consent form before the interview commenced, and one copy was given to the participant.
Results
Our analysis of the transcribed interviews generated six themes including:
• Gross lack of trust in the vaccine.
• Fear of real and perceived side effect.
• Insufficient sensitization of health workers amidst vaccine negative publicity.
• Risk denial
• System inhibition factors
• Religious beliefs against vaccination.
Gross lack of trust in vaccine
Health workers expressed lack of trust in particular against the AstraZeneca vaccine based on several unanswered questions (Table 1). Their concerns varied from why the Ugandan government required a consent for the COVID-19 vaccine contrary to common practice for other vaccination, the short duration of research preceding the recommendation of COVID-19 vaccination and whether this was not a vaccine trial on Ugandans being used as Guinea pigs (Table 2).
| FGD number | Number of participants | Age range/years | Sex | Vaccination status |
|---|---|---|---|---|
| 1 | 12 | 28-52 | Males and females | Vaccinated and unvaccinated |
| 2 | 12 | 26-50 | Males and females | Vaccinated and unvaccinated |
| 3 | 12 | 33-52 | Males and females | Vaccinated and unvaccinated |
| 4 | 12 | 38-58 | Males and females | Vaccinated and unvaccinated |
| 5 | 12 | 33-52 | Males and females | Vaccinated and unvaccinated |
| 6 | 12 | 38-58 | Males and females | Vaccinated and unvaccinated |
| 7 | 12 | 28-43 | Males and females | Vaccinated and unvaccinated |
| 8 | 12 | 24-40 | Males and females | Vaccinated and unvaccinated |
| 9 | 12 | 28-48 | Males and females | Vaccinated and unvaccinated |
| 10 | 12 | 20-33 | Males and females | Vaccinated and unvaccinated |
| 11 | 12 | 33-44 | Males and females | Vaccinated and unvaccinated |
| 12 | 12 | 36-65 | Males and females | Vaccinated and unvaccinated |
Note: A total of 144 health workers participated in the focus group discussions age range 20 to 65 years with median age of 36 years.
Table 1: Summary characteristics of the FGD participants.
| Participants number | Age range/years | Sex | Vaccination status |
|---|---|---|---|
| 1 | 31-35 | Male | Vaccinated |
| 2 | 31-35 | Female | Vaccinated |
| 3 | 46-50 | Male | Unvaccinated |
| 4 | 36-40 | Male | Unvaccinated |
| 5 | 36-40 | Male | Unvaccinated |
| 6 | 41-45 | Female | Vaccinated |
| 7 | 36-40 | Female | Vaccinated |
| 8 | 31-35 | Male | Unvaccinated |
| 9 | 26-30 | Male | Unvaccinated |
| 10 | 26-30 | Male | Vaccinated |
| 11 | 36-40 | Female | Vaccinated |
| 12 | 31-35 | Female | Unvaccinated |
| 13 | 36-40 | Female | Unvaccinated |
| 14 | 26-30 | Female | Vaccinated |
| 15 | 26-30 | Female | Vaccinated |
| 16 | 31-35 | Female | Vaccinated |
| 17 | 46-50 | Male | Unvaccinated |
| 18 | 46-50 | Female | Unvaccinated |
| 19 | 31-35 | Female | Unvaccinated |
| 20 | 51-55 | Female | Vaccinated |
Note: Twenty participants were identified for the in depth interviews. Twelve females and eight males. The age range was 28 to 55 years with a median of 36 years.
Table 2: Summary characteristics of the IDI participants.
“This is clearly a clinical trial and we are being duped otherwise why government would ask us to consent for it, something we have never done for other vaccines, Ugandans are being used as guineapig so terrible” (male informant, unvaccinated).
“Vaccine trials take about three years; do you really believe that a vaccine can be truly recommended for global use after testing for only a year? Something is certainly not right here” (Female informant, unvaccinated).
The government’s failure to accept, explain or even take liability for the vaccines side effects/adverse events. As well as the public knowledge that government had accepted to use Astra Zeneca which had been branded as dangerous and rejected in other countries but dumped in Uganda further eroded trust for the vaccine among health workers.
“If the government is confident about the vaccine, why aren’t they explaining the side effects that we see here on our clients every day, the government is even fearful of taking responsibility for these effects, why are they uncomfortable doing so if they are sure of what they are telling us to jab in, by the way do you also realize that AstraZeneca has been branded dangerous in Norway and other developed countries (male informant, unvaccinated).
Health workers were also concerned about the efficacy and effectiveness of the vaccine because it was reportedly manufactured in India, a country that had registered a high COVID-19 prevalence and resurgence waves in spite of the vaccination with AstraZeneca. Additionally, from their own experience, these health workers had reportedly seen many previously vaccinated colleagues turn up with COVID, some reportedly died from severe COVID-19 while COVID-19 patients with no history of COVID-19 vaccination had less severe COVID-19 illness.
“India where this vaccine is being manufactured still has a high COVID-19 prevalence and has also had several resurgences in spite of people being vaccinated even here in the hospital our colleagues who got the COVID-19 jab sometimes turn up or even die of COVID-19 while some of us who never vaccinated have never gotten or only get mild symptoms which raises the question of whether this vaccine prevents or accelerates severe COVID-19” (male informant unvaccinated).
Fear of real or perceived side effects
Fear of side effects the health workers had seen among clients who turned up after vaccination was a barrier for them taking up the vaccine. A few respondents reported they had received several patients come back days or weeks post vaccination with high fevers, swollen arms, severe headaches and difficulty in breathing. Other side effects which although perceived or read from social media scared health workers from getting vaccinated since they neither believed nor dismissed them given the less scientific evidence them had. The perceived effects included the vaccine causing infertility, impotence, body magnetism, vaginal bleeding and brown hair.
“We have seen many patients come back here post vaccination with severe illness, difficulty in breathing or even death. This has not happened commonly with other vaccines we normally get so as a matter of fact, some of us think we are better off not vaccinating than taking the risk of a jab” (Female informant, un vaccinated).
“There is also a lot of information especially about this vaccine causing infertility, impotence, magnetism, severe bleeding in women or even hair turning brown unfortunately, we don’t even have scientific evidence to the contrary so we don’t know what to believe really.” (Female informant, unvaccinated).
Insufficient sensitization of the health workers amidst vaccine negative publicity
A few health workers were hesitant to take up the vaccine because they lacked sufficient knowledge about it. The government had not reportedly done enough sensitization to the health workers especially on the components, nature, development process, side effects and benefits of taking up the vaccine. There were no clear eligibility criteria, indication or contra indications to the vaccine. They were not also reportedly sensitized enough on the other vaccine alternatives and why government was only bent on AstraZeneca. This was against the background that there was a lot of negative publicity about the COVID-19 vaccine including but not limited to misinformation and distortion of scientific facts on the internet and other social media platforms about how dangerous the vaccine was hence casting more doubt about the vaccine.
“Information about this vaccine is so scanty, there has been no proper sensitization of the workers but just government ordering and threatening us with losing jobs what is in this vaccine,… what are the benefits of getting it, what is the eligibility criteria…., what are the alternatives, how about all the allegations we here about, when will government come out to clarify these issues. We can’t just ignore these pockets of information so caution” (male, informant, unvaccinated).
Risk denial
Lack of COVID-19 related fear or death was frequently reported by many respondents as one of the reasons some health workers did not take up the vaccine. Several workers believed in their own natural immunity given they had been on the COVID-19 wards, treated many COVID-19 patients but only got mild symptoms of the disease or none at all. Some of them actually retorted that strict observance to standard operating procedures was much safer and less hazardous than taking the up the vaccine.
“I have been here during the first and second wave, treated so many COVID-19 patients but for us some just get mild symptoms or other never at all. So we trust in our natural immunity besides, some of us believe that strictly observing the standard procedures is much safer than taking the vaccine” (female informant, unvaccinated).
System inhibition factors
A few respondents reported that there were many system gaps in the processes, functions and tools designed to get the health workers accept the COVID-19 vaccine. The gaps included government insistence that all workers take up the vaccine without due diligence which they perceived as coercion in their view, vaccinating them without prior testing to see if they had not been exposed in the first place, few vaccination posts making it expensive to access, putting vaccination centres within the very hospitals that had COVID-19 patients and hence a risk of exposure for those seeking vaccination among others.
“Why does the government insist that we all get vaccinated more over without even testing us to see if we have had COVID-19 already you see people lining up in crowds to get the vaccine, moreover the same hospital with COVID-19 patients, isn’t this a super spreader really”(female informant, vaccinated).
Religious beliefs against vaccination
Some health workers admitted that their religious beliefs did not agree with the notion of vaccines as prevention. Such faiths defined the prevention of illness as a preserve of God and not vaccines. They therefore saw no need for vaccination other than to please their superiors or secure their jobs.
“Our religion believes it’s only the will of God that keeps us alive. Those vaccines are just a waste of time, I have many friends in this hospital who just pray every morning not to get COVID-19 before they go to the COVID-19 ward and believe me for the two waves they have never got it as for me, I just got it (the vaccine) to secure my job because we are told that soon anyone who is not vaccinated will not enter that hospital gate. Its prayers, prayers and the Lord listens” (male informant, vaccinated).
Discussion
Our findings indicate that health workers' vaccine hesitancy is a function of multiple overlapping themes including; gross lack of trust in the vaccine, fear of real/perceived side effects and insufficient sensitization amidst vaccine negative publicity. O themes were risk denial, system inhibition factors and religious beliefs.
Health workerswanted more information about the COVID-19 vaccine especially with regard to its production processes, the types, need for consent, contents, efficacy, effectiveness, contra-indications and long term safety. They also feared real or perceived side effects of the vaccine based on what they saw and interpreted in their practice and the confusing negative publicity or misinformation over the internet and social media platforms which they neither believed nor dispelled because of lack of relevant scientific knowledge. Most of the vaccine hesitancy reported by Ugandan health workers is a function of misinformation or lack of sufficient knowledge/information by about the COVID-19 vaccine. Acceptance of a medical product, service or intervention is dependent on how much the recipients know, understand and trust it in terms of safety, benefit or risk reduction [22-24]. Knowledge is power and a foundation for appropriate decision- making, especially when making health choices. The importance for governments to involve, thoroughly inform and train of health workers on vaccine trial protocols, program design and the benefits versus risks has been found to be crucial for their decision making [25,26]. Lack of adequate knowledge, involvement and sensitization of the beneficiaries of health interventions as barriers to vaccine acceptance has also been found other studies in Europe and Africa [27-29].
The importance of trust for successful implemention of health interventions has been amplified by the health belief model, and also emphasized by the World Health Organsition in order to reduce barriers to vaccine acceptance in high and low income settings [6,12,30,31]. Fear of side effects as a barrier to uptake of vaccines has also been shown repeatedly in prevoius research from Europe, Asia and Africa [32-35].
Health workers believing in their own natural immunity and just adhering to the standard operating procedures as protective enough against the COVID-19 virus is indicative of lack of risk susceptibility. Many health workers did not perceive themselves as being at risk of contracting COVID-19 at all. Such risk denial may in part be attributed to the the health workers ' actual experiences on the ground of both (unvaccinated but healthy) colleagues as well as vaccinated who still got COVID-19 indicating that a proper understanding of partial protection, and, individual versus population level risk if missing R. The concept of risk denial is a known barrier to safer health behavioural change because individuals in denial tend to find confidence in scapegoating, self-confidence, false or perceived confidence and comparison between risks [36] also supported by other studies on behavioural/ attitudinal change [37-40].
The COVID-19 vaccine roll-out in Uganda would most likely have benefitted from a proper explanation from the government why it was important for every health worker to get vaccinated immediately even without previous antibody testing because of the status of the pandemic and scarcity of resources. Also the association between few vaccination posts and vaccination being conducted in hospital premises and the urgency of starting up the vaccination program despite very few available doses and other resources available, lack of affordable testing kits and refrigeration settings outside of the hospitals, should have been explained the targeted recipients (health workers). Raising knowledge and awareness on health program strategies to recipients is vital to program success and acceptance [41]. Awareness and knowledge about vaccine interventions and their objectives and processes as drivers to acceptance has been established in other studies [42,43].
Finally, religious beliefs were reported as barriers to COVID-19 vaccine uptake. Like for many other health interventions, there is sometimes an ideological clash between science and divine healing even among educated health personnel [44,45]. . Although this normally happens in minority religious groups, it may have a negative multiplier effect on other members of society [46]. as also reported earlier by other studies in the United States, Europe, Asia and Africa [47-55].
Conclusion and Recommendations
Our findings emphasize the importance for governments with low uptake of COVID-19 context specific tools/guides for dissemination of information, education and communication about the vaccine. The tools should cover vaccine trial processes and why there was need for emergency authorization of the vaccine, vaccine types, contents, efficacy, and effectivenes. The tools should also explain why consent for this vaccine is important, benefits versus risks, side effects mitigation and eligibility versus contra-indications for certain types of vaccines. To increase health workers' trust and awareness, peers who have been vaccinated, or who have experienced and survived, both vaccinated and unvaccinated, could also be used as trusted sources to inform both health worker colleagues about the vaccine. This could be done through the health worker’s social media platforms, union or association websites, personal statements, editorials or other media.
The government could also consider conducting sustained media campaigns either in mainstream or social media to not only explain the safety and benefits, but also dispel misinformation about the vaccine. Using people who got the vaccine and survived Covid-19, religious leaders and other opinion leaders in these campaigns could bolster the effort especially health workers.
To address system inhibition factors, the government could consider contexts specific dialogue series with health workers. This could be done at the different health system levels from the village health teams, to the national referral hospitals, health workers unions’ or regulatory bodies. The dialogue should aim at helping health workers understand the rationale for the rapid implementation and roll-out procedures. The government should ensure that other vaccine types are accessible and available to the majority in need, and debunk misconceptions associated with certain vaccines e.g. eh Astra Zeneca. If possible, vaccination posts could also be increased and set outside hospital settings in common public spaces to reduce the fear of exposure.
Study Limitations
Qualitative studies and deductions are purely based on narratives from the respondents with no statistical inferences. The fact that the interviewees themselves volunteered the information, however, strengthens the the validity of the data. Additionally, we also triangulated our data collection methods (FGDs, IDIs) and conducted iterative analyses. This helped us to check for consistency and contradictions inside and across the groups and interviewees. Also, our team was multi-disciplinary, grounded and had a good contextual understanding of aspects relating to uptake of Covid-19 vaccine in the study settings.
REFERENCES
- MOH, Corona Virus (Pandemic) COVID-19. Kampala: Ministry of Health. 2021.
- Muhamadi L, Edith N, James W, Museene SK, Peterson SS, Ekstrom AM. Lack of Trust, Insufficient knowledge and Risk denial; an in-depth Understanding of Health worker Barriers to uptake of the Covid-19 vaccine at Iganga Hospital Eastern Uganda, and Mengo Hospital Kampala Uganda. medRxiv. 2021.
- WHO, WHO African Region numbers at a glance. Brazzaville: WHO Regional office for africa. 2021.
- MOH, Update on Covid-19 vaccination in Uganda, Kampala: Ministry of health. 2021.
- Museveni Y. Presidential statement to the nation on progress of the Covid 19 response, Government atatehouse: Kampala. 2021.
- WHO, Vaccine acceptance is the next hurdle, Geneva: WHO. 2020.
- Director D. Covid status report. Kampala, Mengo hospital. 2021.
- DHO, Monthly Covid updates. Iganga: District health office. 2021.
- Smith LE, Amlôt R, Weinman J, Yiend J, Rubin GJ. A systematic review of factors affecting vaccine uptake in young children. Vaccine. 2017;35(45):6059-6069.
- Corona Virus Diesease (COVID-19) pandemic, Geneva: WHO. 2020.
- Fares S, Elmnyer MM, Mohamed SS, Elsayed R. COVID-19 Vaccination Perception and Attitude among Healthcare Workers in Egypt. J Prim Care Community Health. 2021.
- Muhamadi L, Edith N, James W, Museene SK, Peterson SS, Ekstrom AM. Lack of Trust, Insufficient knowledge and Risk denial; an in-depth Understanding of Health worker Barriers to uptake of the Covid-19 vaccine at Iganga Hospital Eastern Uganda, and Mengo Hospital Kampala Uganda. medRxiv. 2021.
- Uganda demographic survey. Kampala: UBOS. 2014
- Corona virus (pandemic) Covid 19. Kampala: Ministry of health. 2021.
- Boyden J, Ennew J. Children in focus: A manual for participatory research with children. Rädda Barnen; 1997.
- Holloway, A-Z of qualitative research in health care. Oxford. 2008.
- Fleury J, Lee SM. The social ecological model and physical activity in African American women. American J Commun Psychol. 2006;37(1):129-140.
- Stewart DW, Shamdasani PN. Focus groups: Theory and practice. Sage publications; 2014.
- Naomi RH. Managing moderator stress: Take a deep breath. You can do this. Marketing Research 2009;21(1):28-29.
- Dahlgren L, Emmelin M, Winkvist A. Qualitative methodology for international public health. Umeå Universitet; 2007.
- Morse F, Qualitative research methods for health proffesionals. Oaks. Sage Publications; 1995.
- Opel DJ, Salmon DA, Marcuse EK. Building trust to achieve confidence in COVID-19 vaccines. JAMA Network Open. 2020;3(10):e2025672.
- Oz M, Cetinkaya N, Apaydin A, Korkmaz E, Bas S, Ozgu E, et al. Awareness and knowledge levels of Turkish college students about human papilloma virus infection and vaccine acceptance. J Cancer Educ. 2018;33(2):260-268.
- Ozawa S, Stack ML. Public trust and vaccine acceptance-international perspectives. Hum Vaccin Immunother. 2013;9(8):1774-1778.
- Moilanen T, Rahkonen N, Kangasniemi M. Finnish adolescents' perceptions of their health choices: A qualitative study. Nurs Health Sci. 2021.
- Baronas AM, Louis MR. Restoring a sense of control during implementation: How user involvement leads to system acceptance. Mis Quarterly. 1988:111-124.
- Deal A, Hayward SE, Huda M, Knights F, Crawshaw AF, Carter J, et al. Strategies and action points to ensure equitable uptake of COVID-19 vaccinations: A national qualitative interview study to explore the views of undocumented migrants, asylum seekers, and refugees. J Migr Health. 2021:100050.
- Truong J, Bakshi S, Wasim A, Ahmad M, Majid U. What factors promote vaccine hesitancy or acceptance during pandemics? A systematic review and thematic analysis. Health Promot Int. 2021.
- Kanyike AM, Olum R, Kajjimu J, Ojilong D, Akech GM, Nassozi DR, et al. Acceptance of the coronavirus disease-2019 vaccine among medical students in Uganda. Trop Med Health. 2021;49(1):1.
- Majid U, Ahmad M. The factors that promote vaccine hesitancy, rejection, or delay in parents. Quali Health Res. 2020; 30(11):1762-1776.
- Prickett K, Habibi H, Carr PA. COVID-19 Vaccine Hesitancy and Acceptance in a Cohort of Diverse New Zealanders. SSRN. 2021.
- Graffigna G, Palamenghi L, Barello S, Stefania B. “Cultivating” acceptance of a COVID-19 vaccination program: Lessons from Italy. Vaccine. 2020; 38(48):7585.
- Gallant AJ, Flowers P, Deakin K, Cogan N, Rasmussen S, Young D, et al. Barriers and enablers to influenza vaccination uptake in adults with chronic respiratory conditions: Applying the behaviour change wheel to specify multi-levelled tailored intervention content. Psychology Health. 2021:1-20.
- Guidry JP, Laestadius LI, Vraga EK, Miller CA, Perrin PB, Burton CW, et al. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am J Infect Control. 2021;49(2):137-142.
- Bongomin F, Olum R, Andia-Biraro I, Nakwagala FN, Hassan KH, Nassozi DR, et al. COVID-19 vaccine acceptance among high-risk populations in Uganda. Ther Adv Infect Dis. 2021;8:20499361211024376.
- Peretti‐Watel P. Neutralization theory and the denial of risk: Some evidence from cannabis use among French adolescents. The British Journal of Sociology. 2003;54(1):21-42.
- Barrios JM, Hochberg Y. Risk perception through the lens of politics in the time of the COVID-19 pandemic. Nat Bureau Economic Res; 2020.
- Wise T, Zbozinek TD, Michelini G, Hagan CC, Mobbs D. Changes in risk perception and self-reported protective behaviour during the first week of the COVID-19 pandemic in the United States. R Soc Open Sci. 2020;7(9):200742.
- Motta Zanin G, Gentile E, Parisi A, Spasiano D. A preliminary evaluation of the public risk perception related to the COVID-19 health emergency in Italy. Int J Environ Res Public Health. 2020;17(9):3024.
- Huynh TL. Data for understanding the risk perception of COVID-19 from Vietnamese sample. Data in brief. 2020;30:105530.
- Elgendy MO, Abdelrahim ME. Public awareness about coronavirus vaccine, vaccine acceptance, and hesitancy. J Med Virol. 2021;93(12):6535-6543.
- Wilpstra C. Vaccine knowledge and vaccine attitudes of undergraduate nursing students doctoral dissertation, University of Windsor.2020.
- Urairak B. The Management of behavior considerations for acceptance and uptake of COVID-19 vaccines among Nurses in Thailand. Acad Strateg Manag J. 2021;20:1-8.
- Parsons SK, Cruise PL, Davenport WM, Jones V. Religious beliefs, practices and treatment adherence among individuals with HIV in the southern United States. AIDS Patient Care. 2006;20(2):97-111.
- Vess M, Arndt J, Cox CR, Routledge C, Goldenberg JL. Exploring the existential function of religion: The effect of religious fundamentalism and mortality salience on faith-based medical refusals. J Pers Soc Psychol. 2009;97(2):334.
- Ko LK, Taylor VM, Mohamed FB, Do HH, Gebeyaw FA, Ibrahim A, et al. “We brought our culture here with us”: a qualitative study of perceptions of HPV vaccine and vaccine uptake among East African immigrant mothers. Papillomavirus Res. 2019;7:21-25.
- Handebo S, Wolde M, Shitu K, Kassie A. Determinant of intention to receive COVID-19 vaccine among school teachers in Gondar City, Northwest Ethiopia. Plos One. 2021;16(6):e0253499.
- De Figueiredo A, Simas C, Karafillakis E, Paterson P, Larson HJ. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: a large-scale retrospective temporal modelling study. Lancet. 2020; 396(10255):898-908.
- Olusanya OA, Bednarczyk RA, Davis RL, Shaban-Nejad A. Addressing Parental Vaccine Hesitancy and Other Barriers to Childhood/Adolescent Vaccination Uptake During the Coronavirus (COVID-19) Pandemic. Front Immunol. 2021;12:855.
- Famuyiro TB, Ogunwale A, des Bordes J, Raji M. COVID-19: perceived infection risk and barriers to uptake of Pfizer-BioNTech and moderna vaccines among community healthcare workers. J Racial Ethn Health Disparities. 2021:1-7.
- Cocchio S, Bertoncello C, Baldovin T, Fonzo M, Bennici SE, Buja A, et al. Awareness of HPV and drivers of HPV vaccine uptake among university students: A quantitative, cross‐sectional study. Health social care community. 2020;28(5):1514-1524
- Mo PK, Wong CH, Lam EH. Can the Health Belief Model and moral responsibility explain influenza vaccination uptake among nurses? J Adv Nurs. 2019;75(6):1188-1206.
- Stilgoe J, Cohen T. Rejecting acceptance: learning from public dialogue on self-driving vehicles. Sci Public Policy. 2021.
- Amith M, Roberts K, Tao C. Conceiving application ontology to model patient human papillomavirus vaccine counseling for dialogue management. BMC Bioinformatics. 2019;20(21):1-6.
- Karras J, Dubé E, Danchin M, Kaufman J, Seale H. A scoping review examining the availability of dialogue-based resources to support healthcare provider’s engagement with vaccine hesitant individuals. Vaccine. 2019;37(44):6594-6600.
Citation: Muhamadi L, Edith N, James W, Tumwesigye NM, Museene SK, Mukakaarisa H, et al. (2021) Lack of Trust, Insufficient Knowledge and Risk Denial: An in-Depth Understanding of Health Workers Barriers to Uptake of the COVID-19 Vaccine at Iganga Hospital Eastern, Uganda and Mengo Hospital Kampala, Uganda. J Vaccines Vaccin. 12:470.
Copyright: © 2021 Muhamadi L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.