Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Geneva Foundation for Medical Education and Research
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Editorial - (2023) Volume 11, Issue 2
Introducing Palliative Care as Service Line in the Emergency Medicine Department
Imad El Majzoub1,2*, Amani Mohamed Abdelwahab Elkhalifa1, Mohammed Abdulbari Al Jaberi1, Mahmood Kishta1 and Mazen Naeim12Department of Emergency Medicine, Khalifa University, Abu Dhabi, United Arab Emirates
Received: 13-Feb-2023, Manuscript No. HCCR-23-19877; Editor assigned: 16-Feb-2023, Pre QC No. HCCR-23-19877(PQ); Reviewed: 02-Mar-2023, QC No. HCCR-23-19877; Revised: 09-Mar-2023, Manuscript No. HCCR-23-19877(R); Published: 16-Mar-2023, DOI: 10.35248/2375-4273.23.11.341
Editorial
The Emergency Department (ED) is the first hospital interface for patients seeking urgent care. Oncology patients or patients with chronic diseases visit the ED for various symptoms that could range between mild discomfort to life threatening emergencies. The ED is unique in providing a variety of services that could range from needs interventions such as IV fluids or pain medications to more advanced diagnostic tests and interventions 24 hours a day, 7 days a week. Often times ED physicians might find themselves in crisis as the reality of serious illness or life/ death decisions can't be ignored or postponed. ED physicians will have to engage in difficult conversations with the patients' family, including conversations pertaining to life sustaining therapies or DNR/DNI options. Thus, both palliative care providers as well as ED physicians are becoming more aware of the need to deliver palliative care services in the ED [1].
Palliative care starts in the ED
Initiating palliative care in the ED will decrease patients’ length of stay, decrease the use of ED resources and improve patient experience by alleviating distress symptoms. Some of the cornerstones of palliative care involve discussions about goals and plan of care, symptom management, and aggressive pain control.
Studies, over the past 5 years, have shown that early integration of palliative care reduces ED visits and hospitalization by 50%. Even admitted patients, on whom palliative care is initiated during their ED visit (compared to latent initiation as inpatients), have a shorter hospital stay by around 4 days. The overall results show fewer inhospital deaths while improving quality of life [2]. Other additional benefits from early palliative care interventions in the ED include resource management, less use of intensive care units, less costs, and increased appropriate direct hospice consult [3].
Given that many palliative care eligible patients present to the ED, emergency physicians have the leverage to advance this standard of care. Emergency physicians can start goal-directed assessments and plans to avoid unwanted treatments, inappropriate resource expenditures, as well as unnecessary suffering. The ED can thus play an important role in becoming a palliative care hub (Figure 1) [2].
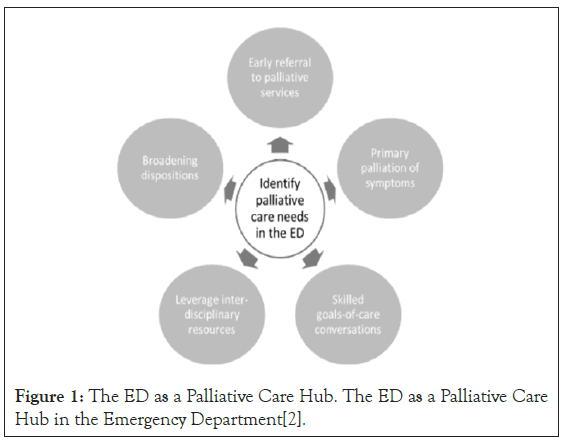
Figure 1: The ED as a Palliative Care Hub. The ED as a Palliative Care Hub in the Emergency Department [2].
Having an ED physician as an advocate of the palliative care program is thus critical to the success and growth of the program. The ED physician will play a pivotal role in educating, recruiting, addressing barriers, and promoting inclusion and continuity of the program within the ED and the hospital as a whole. The ED physician will also bring an added value in terms of addressing a variety of challenges in transitioning the plan of care from the ED to inpatient and outpatient hospital settings while remaining responsive to patients' needs and adjusting the plan of care accordingly [3,4]. The ED physician will thus have to be a member of the palliative care team in order to take calls with the team on floors.
Educational value
Introducing the palliative care service in the ED will help in:
1. Understanding the principles of palliative care among ED health care members.
2. Educating health care staff about the role of palliative care in providing better quality of life to patients eligible for palliative care.
3. Introducing palliative care curriculum into the emergency medicine residency program.
4. Educating ED physicians and health care providers about the importance of the coordination of the patient's plan of care with oncologists and palliative care team.
5. Developing Screening criteria for detecting patients eligible for palliative care and end of life care.
Ancillary medical staff
Nursing staff play an important role in advocating for palliative care and they prove to be a significant source of support. Case managers and charge nurses will receive on- site training which will be delivered by the ED palliative care privileged physician and the palliative care team. The training is a combination of lectures and workshops alongside hospital rounds.
Malpractice issues
Palliative care delivery and ethics are both complementary; and the use of both of them together will help maximize patient protection and satisfaction [5]. Effective palliative care delivery, confidentiality of patient information, use of antibiotics and blood transfusions, nutrition and advance directives are all aspects of palliative care practice. Failure to abide by the legal and ethical aspects of palliative care and end of life care like the DNR/DNI policy will result in malpractice issues.
Barriers to service/potential solutions
The below table shows the barriers and potential solutions to address palliative care needs in the ED [1] (Table 1).
| Limited availability of palliative care team | Increase hours and response time dedicated palliative care staff to emergency Department |
|---|---|
| ED Setting | |
| Crowding | Dedicated private space |
| Lack of privacy | Sound proof curtains or door |
| Fast-paced | Observation units |
| Interventional/procedural | Physician champions |
| Knowledge | |
| Emergency providersPatients and families | Education in Palliative and End of Life Care (EPEC-EM) |
Table 1: The barriers and potential solutions to address palliative care needs in the ED.
Marketing plans for emergency departments
The new palliative care service at the EDs will be introduced to the hospitals through presentations at different departments, grand rounds, workshops, and seminars. The ED physician with palliative care privileges will be a member of the palliative care committee to ensure support and commitment from executive leadership. A needs assessment could also help identify gaps in the current versus ideal practice. The results of the assessment can identify existing resources which could leverage the current practice. Educating patients and family members about the current service is also part of the marketing plan. Case managers or palliative care eligible physicians can talk to patients and their family members directly to help introduce the service.
Performance indicators
There are various involved metrics pertaining to palliative care service assessment in the ED [6], these include:
• Patient satisfaction surveys
• In-hospital mortality rates of palliative care eligible patients
• Length of stay
• Decreased costs (ED visits costs and overall hospitalizations costs)
Departments impacted by the service
The primary department affected with this service is the Department of Internal Medicine; namely, intensive care units, oncology, and palliative care. As mentioned earlier, integrating this service will reduce patients' length of stay at intensive care units, allow for earlier consultation of palliative care team, and early involvement of primary care physicians in the patient's plan of care.
Advantages to the patients and the community
During the course of a chronic or aggressive illness, a severe burden is placed on the patients and their family members. It is often the case that the entire family function is interrupted with the entire family's focus being consumed by the disease itself. In addition to the financial burden that the whole family has to withstand, there's an added emotional suffering. Thus, early palliative care integration reflects positively on both the patient and family. Infact, the quality of palliative care is measured in terms of symptoms management and the family perception of their beloved one's death [3].
Service/privilege replacing other existing privileges
If implemented, palliative care in the EDs will be an add-on service to the current service lines of emergency medicine [7].
Service/privilege approved by agencies
In 2008, The American Board of Emergency Medicine became an official sponsor of Hospice and Palliative Medicine as a subspecialty.
The American Academy of Emergency Medicine (AAEM) dedicates every year during its annual assembly a section on palliative care [8].
References
- Grudzen CR, Stone SC, Morrison RS. The palliative care model for emergency department patients with advanced illness. J Palliat Med. 2011; 14(8):945-950.
[Crossref] [Google Scholar] [PubMed]
- Wang DH. Beyond code status: Palliative care begins in the emergency department. Ann Emerg Med. 2017; 69(4):437-443.
[Crossref] [Google Scholar] [PubMed]
- Mierendorf SM, Gidvani V. Palliative care in the emergency department. Perm J. 2014;18(2):77.
[Crossref] [Google Scholar] [PubMed]
- DeVader TE, Albrecht R, Reiter M. Initiating palliative care in the emergency department. J Emerg Med. 2012; 43(5):803-810.
[Crossref] [Google Scholar] [PubMed]
- Kiesewetter I, Schulz C, Bausewein C, Fountain R, Schmitz A. Patients’ perception of types of errors in palliative care–results from a qualitative interview study. BMC Palliative Care. 2016; 15:1-2.
[Crossref] [Google Scholar] [PubMed]
- Basol N. The integration of palliative care into the emergency department. Turk J Emerg Med. 2015; 15(2):100-107.
[Crossref] [Google Scholar] [PubMed]
- Grudzen CR, Stone SC, Morrison RS. The palliative care model for emergency department patients with advanced illness. Journal of palliative medicine. 2011; 14(8):945-950.
[Crossref] [Google Scholar] [PubMed]
- Palliative Care & Ethics COVID-19 Story Submissions. 2019.
Citation: El Majzoub I, Elkhalifa AMA, Al Jaberi MA, Kishta M, Naeim M (2023) Introducing Palliative Care as Service Line in the Emergency Medicine Department. Health Care Curr Rev. 11:341.
Copyright: © 2023 El Majzoub I, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

