Indexed In
- Open J Gate
- Genamics JournalSeek
- ResearchBible
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
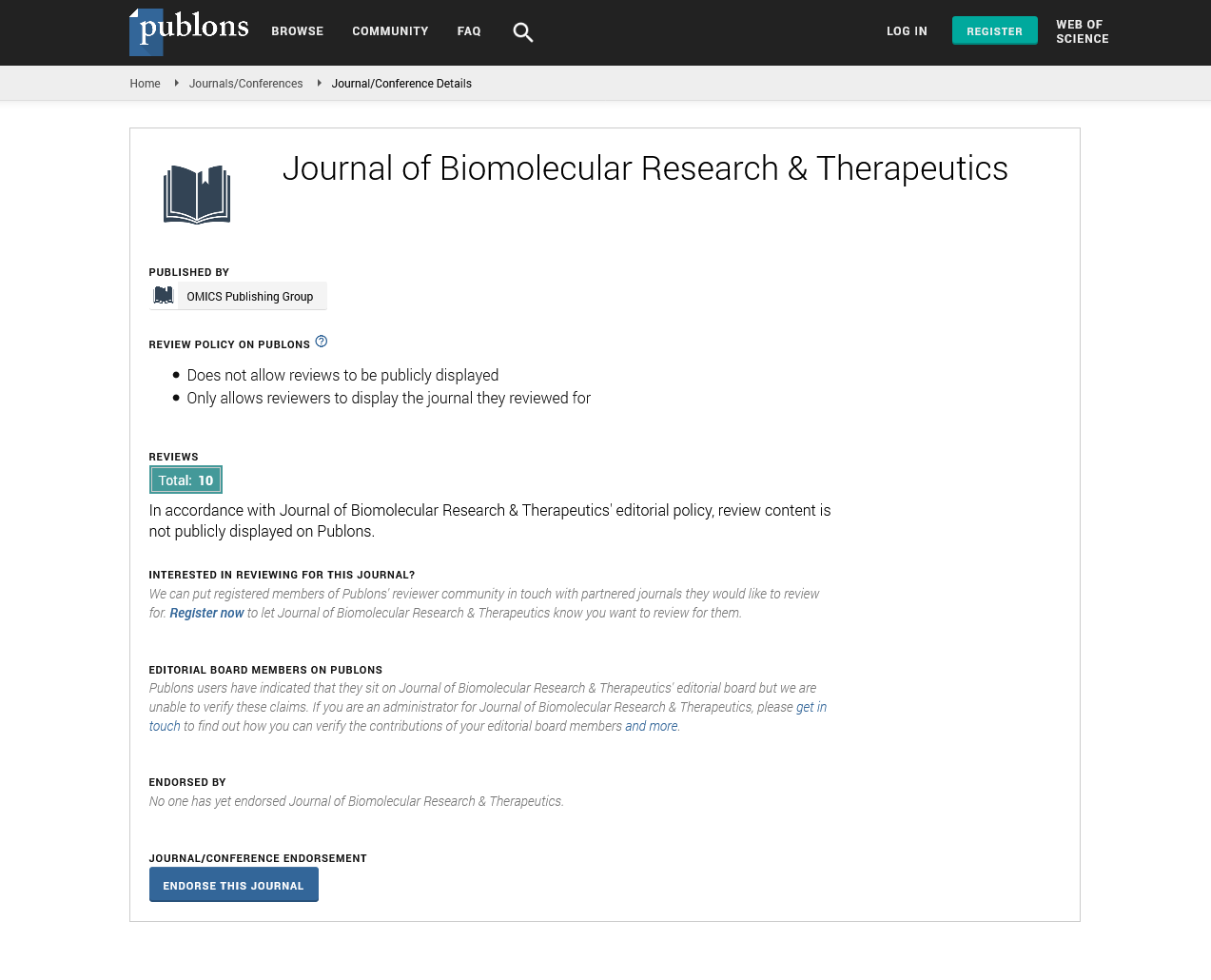
- Publons
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Commentary - (2025) Volume 14, Issue 2
Immunotherapy Strategies for Autoimmune Disorders
David Miller*Received: 28-Mar-2025, Manuscript No. BOM-25-29594; Editor assigned: 31-Mar-2025, Pre QC No. BOM-25-29594; Reviewed: 14-Apr-2025, QC No. BOM-25-29594; Revised: 19-Apr-2025, Manuscript No. BOM-25-29594; Published: 28-Apr-2025, DOI: 10.35248/2167-7956.25.14.437
Description
Immunotherapy has transformed modern medicine by offering approaches that modulate the immune system to restore balance or enhance its protective functions. While initially developed for cancer treatment, immunotherapy is now being explored as a strategy to manage autoimmune disorders, which arise when the immune system mistakenly attacks healthy tissues. Autoimmune diseases such as type 1 diabetes, lupus and multiple sclerosis present complex challenges because they involve dysregulation of immune tolerance, often with varied manifestations in different individuals. A central approach in immunotherapy for autoimmune diseases is the induction of immune tolerance. Therapies are being designed to retrain immune cells so that they recognize self-antigens as harmless. One method involves antigen-specific immunotherapy, where disease-associated proteins are (diabetes with peptides from insulin and in multiple sclerosis with myelin-derived peptides, showing potential to reduce disease progression.
Monoclonal antibodies targeting immune checkpoints have also been adapted for autoimmune therapy. Unlike in cancer, where checkpoint inhibitors are used to enhance immune activity, autoimmune therapies aim to enhance inhibitory pathways. For example, drugs that boost CTLA-4 or PD-1 signaling may reduce excessive immune activity and help restore balance. These approaches are under investigation in diseases such as rheumatoid arthritis and systemic lupus erythematosus. Another strategy involves cellular therapies. Regulatory T cells, which naturally suppress immune activity, are being expanded and infused back into patients to counteract autoimmune responses. Clinical trials using T cell-based therapies for type 1 diabetes and graft-versus-host disease have reported encouraging results. Advances in cell engineering also enable modification of these cells to enhance their suppressive functions, improving their therapeutic potential.
Immunotherapy for autoimmune disorders must address challenges of safety and specificity. Broad immunosuppression can leave patients vulnerable to infections and malignancies. Therefore, current research emphasizes precision treatments that selectively target disease-relevant pathways while preserving protective immunity. This requires detailed understanding of the molecular drivers of autoimmunity, which vary across diseases and individuals. The role of biomarkers in guiding therapy is increasingly recognized. Biomarkers can identify patients most likely to respond and monitor treatment effectiveness. For example, specific cytokine signatures or genetic profiles may help predict which patients benefit from tolerance-inducing therapies. Integrating biomarker analysis with clinical decision-making represents a significant step toward personalized immunotherapy.
Despite challenges, the field is advancing rapidly with novel strategies including nanoparticle-based delivery of tolerogenic agents, gene editing of immune cells and microbiome-targeted interventions. These emerging approaches highlight the dynamic potential of immunotherapy beyond oncology. By focusing on immune regulation rather than suppression, immunotherapy strategies for autoimmune diseases hold the potential to transform patient outcomes. Continued research and clinical trials will clarify their long-term safety and effectiveness, ultimately leading to therapies that restore immune balance and improve quality of life for millions of patients worldwide.
Recent advances are pushing the boundaries of what immunotherapy for autoimmune disease can achieve. A promising avenue involves Antigen-Presenting Cells (APCs) engineered to promote tolerance. Dendritic cells, for example, can be modified ex vivo to express tolerogenic markers or loaded with disease-specific antigens in forms that favor immune suppression. When reintroduced into the patient, these tolerogenic dendritic cells can induce regulatory T cell production, suppress autoreactive effector cells and shift the immune response toward a more balanced state. Moreover, immune checkpoint agonists, beyond simply blocking overactive pathways, are being designed to deliver signals that actively reign in autoimmunity. Agents that mimic or amplify immune-inhibitory signals such as those from CTLA-4, PD-L1, or other regulatory pathways are under development. These agonists aim to dampen overactive immune responses without completely shutting down immune defense, achieving a middle ground between autoimmunity and immunodeficiency.
Another exciting direction is the fusion of gene therapy with immunomodulation. Scientists are exploring ways to edit immune cells to reduce their auto reactivity. For instance, using gene editing tools, researchers can disrupt genes that encode costimulatory molecules required for full immune activation, or introduce genes encoding inhibitory molecules. This could lead to permanently modified immune cells that resist autoimmunity while retaining the ability to fight infections. The concept of tissue-specific delivery is also being refined. Localized immunotherapies such as delivering immunomodulatory agents directly into affected joints in rheumatoid arthritis, or into the pancreas in type 1 diabetes can reduce systemic side effects. Biomaterial scaffolds or hydrogels loaded with tolerogenic agents are being explored to create localized microenvironments that foster immune regulation.
Simultaneously, there is growing interest in combination strategies. For example, combining antigen-specific therapy with checkpoint agonists or with engineered Tregs may produce additive or synergistic benefits. Alternatively, coupling immunotherapy with metabolic modulators for instance, targeting metabolic pathways in T cells to reduce their activation can enhance tolerogenic effects.
Understanding the timing and disease stage at which immunotherapy is applied is critical. Early intervention, possibly even before clinical disease onset or during the initial phases of autoimmune attack, may yield much better outcomes than late-stage interventions when tissue damage has already occurred. Predicting risk via genetic, environmental, or biomarker profiling may enable preventative immunotherapies. Finally, ethical, regulatory and societal aspects are being actively debated. Ensuring long-term monitoring of patients, standardizing protocols, managing risks of off-target effects and delivering equitable access are essential considerations. Public engagement and transparent risk-benefit communication will be needed as more powerful immunotherapeutic approaches, including engineered cells and gene editing, move closer to routine clinical use.
Citation: Miller D (2025). Immunotherapy Strategies for Autoimmune Disorders. 14.437
Copyright: © 2025 Miller D. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.