Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
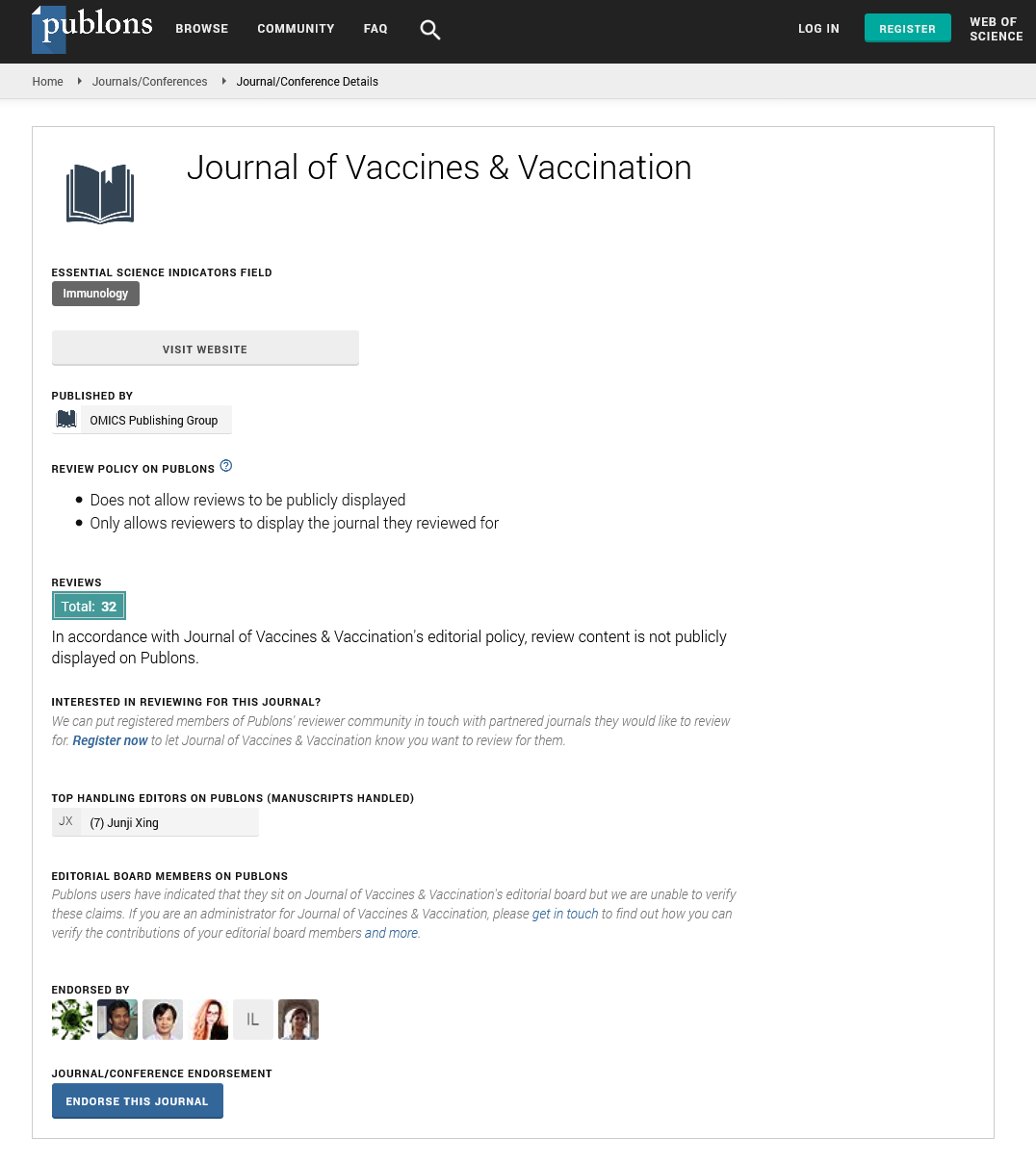
- Publons
- MIAR
- University Grants Commission
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Commentry - (2022) Volume 13, Issue 4
Hib Vaccine against Invasive Haemophilus Influenza Type B Disease
Mrigesh Anak*Received: 20-May-2022, Manuscript No. JVV-22-17762; Editor assigned: 23-May-2022, Pre QC No. JVV-22-17762 (PQ); Reviewed: 10-Jun-2022, QC No. JVV-22-17762; Revised: 16-Jun-2022, Manuscript No. JVV-22-17762 (R); Published: 24-Jun-2022, DOI: 10.35248/2157-7560.22.13.489
Description
Haemophilus influenza is a gram-negative coccobacillus that commonly infects children's upper respiratory tracts via nasal secretions. While non-encapsulated bacillus strains are relatively harmless, strains with a polysaccharide capsule or coat cause a more serious disease. Until the Hib vaccine became available, the most common cause of meningitis in children under the age of five was it was also a common cause of infections in children's ears, lungs, blood, skin, and joints. Hib vaccines help prevent Haemophilus infections but not infections caused by other strains of the H. influenzae bacteria. Many childhood infections are caused by H. influenzae. Hib bacteria can live in healthy people's noses and throats and usually does not cause any problems or symptoms. The bacteria are typically spread through infected droplets of fluid in coughs and sneezes, much like cold and flu viruses. Healthy people, who carry the bacteria, as well as those who are ill with Hib, can spread the bacteria. Invasive disease episodes occur when Hib is isolated from blood, Cerebrospinal Fluid (CSF), or other normally sterile fluids such as pleural fluid. This organism, which primarily causes pneumonia and meningitis in young children, is a major public health concern in many parts of the world, with up to 3 million cases of serious disease occurring each year. Antibiotic resistance in Hib has been reported in many parts of the world, and vaccination is the only public health tool that can rapidly reduce the global incidence of Hib disease.
The first vaccine to protect against Hib diseases was introduced in 1985, and an improved vaccine was licenced two years later. Several Hib vaccine preparations are now available; both as single Hib vaccinations and in combination shots (Hepatitis B and Hib vaccines are available in a combined shot). All Hib disease vaccines are inactivated and contain only a portion of the Hib bacterium. A series of Hib vaccines in which PRP was conjugated to various proteins to improve immunogenicity in young children quickly replaced PRP alone. The increased immunogenicity of conjugated polysaccharides means their immune responses are T-cell dependent, whereas responses to pure polysaccharides are T-cell independent, characterized by poor immunogenicity in children under the age of two years and poor immunologic memory. Thus, conjugated polysaccharide vaccines increase Hib antibody levels in children, induce memory cells, and induce a booster response upon subsequent exposure to the type B antigen. Consider administering to patients 5 years of age or older who have not been immunized and are immunocompromised (e.g., sickle cell disease, Leukaemia, HIV or anatomical/functional asplenia).
Hib vaccine is commercially available as a monovalent preparation as well as in combination vaccines containing DTP, sometimes in conjunction with hepatitis B or IPV. PRP antibody concentrations greater than 0.15 g/ml are considered a serological marker for short-term protection; concentrations greater than 1.0 g/ml. 1 month after primary immunisation are considered markers of long-term protective immunity against invasive Hib disease. Antibiotic resistance in Hib has been reported in many parts of the world, and vaccination is the only public health tool that can rapidly reduce the global incidence of Hib disease. The vaccine protects against Haemophilus influenza type B for a long time. Those who have been immunized are protected against Hib meningitis, pneumonia, pericarditis (an infection of the membrane covering the heart) and Hib infections of the blood, bones, and joints. The number of doses required for full immunity varies depending on the vaccine used (three or four). Adults and older children who are at high risk and have never been immunized require at least one dose of the vaccine to be protected. Even though the number of serious Hib illnesses has decreased significantly as a result of the Hib immunisation programme, children should continue to be immunized. Babies and children under the age of five should be immunized against Hib.
Citation: Anak M (2022) Hib Vaccine against Invasive Haemophilus Influenza Type B Disease. J Vaccines Vaccin. 13:489.
Copyright: © 2022 Anak M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.