Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- Google Scholar
- SHERPA ROMEO
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2025) Volume 13, Issue 5
Hepatic Artery Aneurysms in Polyarteritis Nodosa: A Panoramic Mini Review
Patrick Vera Cruz*Received: 06-Apr-2024, Manuscript No. JVMS-24-25398; Editor assigned: 09-Apr-2024, Pre QC No. JVMS-24-25398 (PQ); Reviewed: 23-Apr-2024, QC No. JVMS-24-25398; Revised: 10-Oct-2025, Manuscript No. JVMS-24-25398 (R); Published: 17-Oct-2025, DOI: 10.35248/2329-6925.25.13.596
Abstract
Introduction: Hepatic Artery Aneurysms (HAAs) are rare vascular abnormalities with a high rupture and mortality rates.
Clinical presentation: We are presented with a case of a 25-year-old female with no known comorbidities who sought consult for recurrent cramping abdominal pain, lower extremity discomfort, nausea and vomiting. She was initially managed as acid reflux disease, however, symptom recurrence despite treatment prompted further workup.
Diagnosis and management: CT aerogram and invasive angiography showed a large saccular aneurysm from the hepatic artery proper and collateral blood vessels from the gastroduodenal artery supplying the right and left lobes of the liver. After thorough discussion team, high dose IV steroids were given and then she underwent open surgical resection of the aneurysm with biopsy of the aneurysm wall showed findings consistent with polyarteritis nodosa.
Conclusion: Vasculitis is an important etiology HAA among young women. Clinical presentation may mimic common gastrointestinal disorders. Thus, maintaining a high index of suspicion is needed to avoid missing this diagnosis. For this case, recognition of the urgency in managing the aneurysm, a suitable anatomy for open surgical resection and prompt control of the underlying etiology facilitated the patient’s favorable outcome. Keywords: Hepatic artery aneurysm; Polyarteritis nodosa; Visceral aneurysm; Vasculitis
Keywords
Hepatic artery aneurysm; Polyarteritis nodosa; Visceral aneurysm; Vasculitis
Introduction
Hepatic Artery Aneurysms (HAAs) are rare vascular abnormalities representing 0.002% to 0.4% of all arterial aneurysms with a high rupture rate and a mortality rate of 40%-100%. Due to its rarity, the true incidence and clinical characteristics of HAAs are uncertain. Here, we have a case of a 25-year-old female presenting with recurrent abdominal pain who was initially managed as acid reflux disease but further work-up revealed a common hepatic artery aneurysm associated with vasculitis [1].
Case Presentation
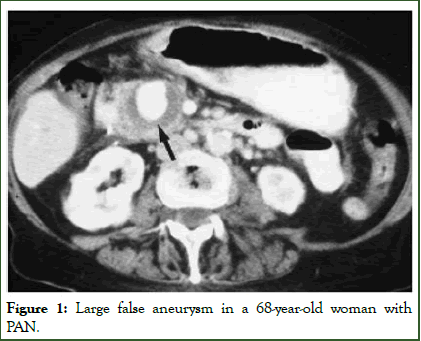
We are presented with a case of a 25-year-old female with no known comorbidities who sought consult for recurrent cramping abdominal pain, lower extremity discomfort, nausea and vomiting. She was initially managed as acid reflux disease, however, symptom recurrence despite treatment prompted further workup. CT aortogram revealed an ovoid enhancing lesion (3.05 cm) in the porta hepatis likely causing the patient’s symptoms. The lesion and hepatobiliary circulation were then further characterized by invasive angiography which showed a large saccular aneurysm from the takeoff of the hepatic artery proper and collateral blood vessels from the gastroduodenal artery supplying the right and left lobes of the liver. After thorough discussion with the management team, she underwent open surgical resection of the aneurysm and biopsy of the aneurysm wall showed findings consistent with polyarteritis nodosa. High dose IV steroid therapy was then initiated postoperatively with good outcomes (Figure 1) [2].
Figure 1: Large false aneurysm in a 68-year-old woman with PAN.
Hepatic Artery Aneurysms (HAAs) are reported to be the second most common visceral aneurysm but, because of its rarity, the true incidence is still unknown. In a study by Abbas et al., true hepatic artery aneurysms represented 12% of 306 patients with true visceral artery aneurysms. On the other hand, in previous reports with smaller populations, the incidence of true HAAs can be as high as 20%-25% of visceral artery aneurysms. There is a 3:2 male predominance and HAAs usually present in the 6th decade of life. Our patient represented a rare minority of young female patients with HAA emphasizing the need for more epidemiologic studies to characterize this disease [3].
The most common etiology of HAAs is vascular remodeling due to atherosclerosis leading to subsequent weakening of the vessel wall. Other important causes, such as fibromuscular dysplasia, congenital and autoimmune connective tissue diseases and vasculitis (i.e., polyarteritis nodosa and Takayasu arteritis), have also been reported. Patients may be asymptomatic but the clinical manifestations, when present, depend on the size and location of the aneurysm. These symptoms include abdominal pain, jaundice, nausea or vomiting. Our patient presented with epigastric, cramping pain associated with nausea and vomiting that was initially managed as acid reflux disease. However, the recurrent episodes of abdominal pain, despite initial management, prompted further-work up revealing a common hepatic artery aneurysm associated with a positive Anti- Neutrophil Cytoplasmic Antibody (p-ANCA). This indicated that the etiology was most likely vasculitis [4].
As with other arteries, a hepatic artery aneurysm is diagnosed if the diameter is more than 1.5 times the diameter of the normal adjacent artery. Multiple diagnostic tests may be employed such as abdominal ultrasound, abdominal Contrast Tomography (CT), CT angiography and magnetic resonance imaging. A hepatic artery aneurysm may appear on ultrasound with nonspecific findings such as ill-defined or cystic lesions in the right lobe of the liver. The European Society for Vascular Surgery (ESVS) guidelines gave a class 1 recommendation for CT angiogram as the diagnostic tool of choice for patients who are suspected to have HAA. Likewise, mesenteric angiogram is also given a class 1 recommendation for patients with HAA being planned for intervention. Our patient first underwent a whole abdominal ultrasound revealing a cystic structure just below the liver along the biliary tree. A CT angiogram was then performed revealing a probable saccular aneurysm in the common hepatic artery and an attenuated left portal vein with periportal edema suggestive of an inflammatory process. The lesion was further characterized through an invasive peripheral angiogram showing a large outpouching with jet-like contrast filling coming from the takeoff of the common hepatic artery [5].
A hepatic artery aneurysm is classified as a true visceral aneurysm involving all layers of the vessel wall. This is different from a pseudoaneurysm which usually results from a tear in the vessel wall due to trauma or localized inflammation and subsequent periarterial hematoma formation. These may be differentiated through duplex ultrasonography where a pseudoaneurysm will show a typical ‘to-and-fro’ pattern or the ‘Yin-Yang’ sign indicating bidirectional flow at the neck of the lesion. Our patient underwent duplex sonography of the portomesenteric arteries showing a dilated common hepatic artery measuring 3.05 cm with hepatopetal flow [6-7].
Discussion
An important clinical implication of an HAAs is its rupture risk and it usually presents with sudden gastrointestinal bleeding. Hepatic artery aneurysms have the highest reported rupture rate among visceral aneurysms of up to 44% with an associated high mortality rate of 40% up to 100%. The classic Quincke’s triad for biliary tree hemorrhage composed of jaundice, biliary colic and gastrointestinal bleeding is present only in 22%-35% of cases of ruptured HAAs. Because of the high rupture and mortality rates, previous reports have recommended immediate repair even if asymptomatic. However, there is a growing volume of evidence reporting that only a small fraction of asymptomatic patients eventually develop symptoms or significantly increase in size. In the latest 2020 European SVS guidelines, the recommendations include repair of: 1) All symptomatic aneurysms regardless of size (Grade 1A recommendation); 2) Asymptomatic aneurysms >2.0 cm in diameter in patients without significant comorbidity (Grade 1A recommendation); 3) Asymptomatic aneurysms with growth of 0.5 cm/year (Grade 1C recommendation); and 4) Asymptomatic HAAs that is >5.0 cm in patients with significant comorbidities (Grade 1B recommendation). Hence, for our patient, urgent intervention was indicated [8-11].
The choices of intervention for the HAA are either endovascular or open surgical approaches. Reports show similar long term outcomes that primarily depend on aneurysm location. In the ESVS guidelines, it is recommended that the ideal procedure of choice should allow aneurysm exclusion while maintaining liver circulation. Just as in our patient, lesions along the common hepatic artery may usually be ligated or resected owing to the collateral perfusion provided by the gastroduodenal and right gastric artery branches. Hence, our patient underwent open surgical resection of the aneurysm with end-to-end anastomosis without intra-or peri-operative complications. The procedure also allowed the biopsy and histopathologic examination of the resected hepatic artery that showed showed neovascularization, acute and chronic inflammation with fibrinoid necrosis consistent with PAN [12-14].
The biopsy specimen plus the findings of positive p-ANCA and medium vessel involvement confirmed the diagnosis of polyarteritis nodosa as the cause of the HAA in our patient. Hence, immunosuppressive medications with high dose IV steroids was given for control of the vasculitis which was tapered after the surgery. Thus, she was discharged on the fourth postoperative day without symptoms of abdominal pain, nausea or vomiting and with oral prednisone as take home medications for control of the autoimmune vasculitis [15-20].
Conclusion
Vasculitis is an important etiology of hepatic artery aneurysms that must be considered especially among young women. The clinical presentation is related to its size and location and may present with nonspecific symptoms that mimic more common gastrointestinal disorders. Thus, maintaining a high index of suspicion is needed to avoid missing this diagnosis. For this case, recognition of the urgency in managing the aneurysm, a suitable anatomy for open surgical resection and prompt control of the underlying etiology facilitated the patient’s favorable outcome.
References
- Altaca G. Ruptured aneurysm of replaced left hepatic artery as a cause of hemorrhagic shock: A challenge of diagnosis and treatment. Inter cardio thoracic surg. 2011;14(2):220-222.
- Chadha M, Ahuja C. Visceral artery aneurysms: Diagnosis and percutaneous management. Semin Inter Rad. 2009;26:196-206.
- Arneson MA, Smith RS. Ruptured hepatic artery aneurysm: Case report and review of literature. Anna vascular surg. 2005;19:540-545.
- Abbas MA, Fowl RJ, Stone WM, Panneton JM, Oldenburg WA, Bower TC, et al. Hepatic artery aneurysm: Factors that predict complications. J Vasc Surg. 2003;38(1):41-45.
- Haghighatkhah H, Taheri MS, Kharazi SM, Zamini M, Khorasgani SR, Zarkani ZJ. Hepatic artery aneurysms as a rare but important cause of abdominal pain; a case series. Arch Acad Emerg Med. 2019;7(1):e25.
- Lal RB, Strohl JB, Piazza S, Aslam M, Ball D, Patel K. Hepatic artery aneurysm. J Cardiovasc Surg. 1959;15:509-513.
- Salcuni PF, Spaggiari L, Tecchio T, Benincase A, Azzarone M. Hepatic artery aneurysm: An ever present danger. J Cardiovasc Surg. 36;1995: 595-599.
- Rosenberg A, Trebska-McGowan K, Reichman T, Sharma A, Cotterell A, Strife B, et al. Management of hepatic artery aneurysm: A case series. Ann Hepatobiliary Pancreat Surg. 2020;24(3):333-338.
- Cordova AC, Sumpio BE. Visceral artery aneurysms and pseudoaneurysms-should they all be managed by endovascular techniques? Ann Vasc Dis. 2013; 6:687.
- Dolapci M, Ersoz S, Kama NA. Hepatic artery aneurysm. Annals Vasc Sur. 2003;17(2):214-6.
- Huisman M, van den Bosch MA, Mooiweer E, Molenaar IQ, van Herwaarden JA. Endovascular treatment of a patient with an aneurysm of the proper hepatic artery and a duodenal fistula. J Vascul Surg. 2011;53:814–817.
- Wu L, Wang LJ, Wong YC, Hung YC, Liu YC, Hsu YP. Hepatobiliary and Pancreatic Hemobilia caused by bleeding from hepatic artery aneurysms. J Gastroenterol Hepatol. 2010;648.
- Roberto M, Meytes V, Liu S. Ruptured hepatic aneurysm as first presenting symptom of polyarteritis nodosa. Oxf Med Case Reports. 2018.
- Dolapci M, Ersoz S, Kama NA. Hepatic artery aneurysm. Ann Vasc Surg. 2003;17:214-216.
- Chaer RA, Abularrage CJ, Coleman DM, Eslami MH, Kashyap VS, Rockman C, et al. The society for vascular surgery clinical practice guidelines on the management of visceral aneurysms. J Vasc Surg. 2020;72:3S-39S.
- Rothenberg KA, McFarland GE, Stern JR. Endovascular repair of ruptured hepatic artery pseudoaneurysm secondary to fibromuscular dysplasia. Vasc Endovascular Surg. 2019;53:66-70.
- Shelton J, Raviraj S. A Case Report: Hepatic artery pseudoaneurysm causing life-threatening haemobilia. Int J Surg Case Rep. 2021;86:106350.
- Berry R, Han J, Girotra M, Tabibian JH. Hemobilia: Perspective and role of the advanced endoscopist. Gastroenterol Res Pract. 2018;2018:3670739.
- Cordova AC, Sumpio BE. Visceral artery aneurysms and pseudoaneurysms-should they all be managed by endovascular techniques? Ann Vasc Dis. 2013;6(4):687-693.
- Scott A, Berceli Y. Hepatic and splenic artery aneurysms. 2005;18:196-201.
Citation: Cruz PV (2025) Hepatic Artery Aneurysms in Polyarteritis Nodosa: A Panoramic Mini Review. J Vasc Med Surg. 13:596.
Copyright: © 2025 Cruz PV. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.