Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Publons
- International committee of medical journals editors (ICMJE)
- Geneva Foundation for Medical Education and Research
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2025) Volume 28, Issue 6
From Hurt to Harm: How Childhood Trauma Shapes Cognitive Control and Decision Making in Late-Life Depression
Naomie Conde1, Laura Osborne1, Ayla Inja1, Josie-Anne Bertrand2, Gustavo Turecki1,2 and Stéphane Richard- Devantoy1,2,3*2Douglas Mental Health Research Institute, McGill Group for Suicide Studies, Montreal, Quebec, Canada
3Department of Psychiatry, Douglas Mental Health University Institute, Montréal, Quebec, Canada
Received: 13-Oct-2025, Manuscript No. JOP-25-30091; Editor assigned: 15-Oct-2025, Pre QC No. JOP-25-30091; Reviewed: 29-Oct-2025, QC No. JOP-25-30091; Revised: 04-Nov-2025, Manuscript No. JOP-25-30091; Published: 12-Nov-2025
Abstract
Objective: To investigate the neuropsychological component features of elderly patients with a history of late-life depression reporting a previous history of Childhood Trauma (CT).
Methods: Outpatients between 60 and 85 years old with a recent history of late-life depression were divided into two groups, childhood trauma and no childhood trauma, according to a previous history of childhood trauma assessed with the Childhood Trauma Questionnaire (CTQ). Cognitive abilities were assessed using the stroop color and word test (inhibition), iowa gambling task (decision-making), and verbal fluency test (semantic verbal fluency).
Results: Total CTQ scores were associated with lower stroop color and word test time scores (p=0.041). Physical Abuse (PA) was associated with a lower Iowa Gambling Task (IGT) net score (p=0.015). Emotional Neglect (EN) was associated with a higher semantic verbal fluency score (p=0.021) and a lower stroop test time score (p=0.037). Emotional abuse, sexual abuse and physical neglect had no neuropsychological pattern. These results remained significant even after controlling for confounding factors including age, gender, level of depression, antidepressant treatment, and history of previous suicide attempts.
Conclusion: Patients with a history of physical abuse had low decision-making scores and those with a history of emotional neglect had good cognitive control. It is necessary to examine how neurocognitive mechanisms are impacted by childhood traumas to develop therapeutic intervensions that improve cognitive performance in older adults.
Keywords
Child abuse; CTQ; Late-life depression; Stroop; Decision-making
Introduction
The experience of a traumatic childhood event is both common and a public health concern with approximately 47% of older adults reporting having experienced a form of Childhood Trauma (CT) [1,2]. Childhood Trauma (CT), including abuse and maltreatment, is generally defined by sustained or repeated exposure to events that typically involve a betrayal of trust [3]. Active examples of CT include childhood sexual, physical and emotional abuse, whereas passive examples include emotional and physical neglect [4]. Experiencing maltreatment in childhood significantly increases the odds of suicide attempts and depression in adulthood, with individuals being 24 times more likely to attempt suicide [5]. While current research shows that deficits in decision-making, category verbal fluency and inhibition are associated with a history of suicidal behaviour in patients with mood disorders, the specific neurocognitive mechanisms that link childhood traumas to suicide attempts in older adulthood remain unclear [6].
Experiences of childhood maltreatment have widely been found to be associated with the development of cognitive dysfunction and suicidal behaviours in children, young adults, and adults [7-9]. Furthermore, previous literature has investigated the mechanisms in which childhood maltreatment influences cognition throughout development. In a 2019 systematice review, Su, et al. [9] examines cognitive development through nine domaines of cognitive functioning, including but not limited to executive functioning, processing, and processing speed, to demonstrate an association between trauma subtypes (i.e., emotional, physical, sexual, abusive, or neglectful) and cognitive impairment. One potential factor that predicts the relationship between childhood trauma and suicidal behviours is disasociation [10]. However, disassociative experiences do not pinpoint the cognitive meachanisms involved in this association.
Although the impact of childhood trauma has been extensively studied in children and adolescent populations, research has yet to examine its impact on older adults, particularly on those with a diagnosis of depression [2]. One study demonstrates that in older adults aged 65-85, adverse childhood events were associated with a more rapid decline in processing speed when depressive symptoms were present [11]. However, this study did not use the CTQ questionnaire and did not explore specific subtypes of childhood abuse. Furthermore, current research has not examined the implications of childhood trauma on suicide vulnerability in older adults. It is crucial to understand the specific cognitive functions that are impacted by CT, specifically as it relates to depression, in order to improve targeted treatments.
Despite growing interest in the link between childhood trauma and suicide attempts in adulthood, research exploring the interactions between CT and cognition has been hindered by the lack of consensus on how to define and measure CT. As a result, existing research on CT has faced limited internal and external validity, reducing the generalizability of findings and restricting their relevance to the development of clinical treatments. One solution to improving the measurement of childhood trauma may be to systematically rely on a validated and reliable questionnaire. This approach will allow data to be obtained in a way that is replicable and generalizable across different contexts. Perhaps the most promising existing tool in this regard is the Childhood Trauma Questionnaire (CTQ), which remains the most widely used quantitative measure of childhood trauma [12]. The CTQ remains the front-runner in the assessment of CT [13,14].
The current study aims to investigate the neuropsychological features of elderly patients with a history of late-life depression reporting a previous history of childhood trauma. We hypothesize that patients who have experienced childhood trauma will have poorer performances on all neuropsychological assessments, including the stroop color and word test (inhibition), iowa gambling task (decision-making), and verbal fluency test (semantic verbal fluency), compared to those without a history of childhood trauma. Specifically, we predict that patients who have experienced childhood trauma will have poorer cognitive control and decisionmaking abilities.
Methods
Participants
Outpatients ages 60 to 85 years who present with a history of latelife depression, were recruited from an ongoing study to identify neurocognitive markers of suicide behaviours. All participants recruited in this study were separated into two subject groups (Childhood Trauma vs. No Childhood Trauma) determined by their scores on the Childhood Trauma Questionnaire (CTQ). The study was approved by the douglas institute research ethics board. Prior to enrollment, participants received a thorough briefing on the aim and procedures of the study, their role as participants, and the use of their data. All enrolled participants provided written informed consent. Participant anonymity and data security were ensured by the use of subject ID’s for all records and passwordprotected, secure data storage. All participants presented with a recent (in the previous six months) diagnosis of a major depressive episode according to the Structured Clinical Interview for Axis I DSM-IV-TR (SCID I-RV) [15]. Patients were excluded from the study if they had a lifetime history of schizophrenia, bipolar disorder, neurological disease or a history of alcohol/drug abuse or dependence over the last 12 months. Participants were taking medication at recruitment (Table 1). Participants were English or French-speaking natives of Québec, Canada.
Measures
Clinical assessment: The severity of depression was scored based on the Hamilton Rating Scale for Depression (HAMD-1) [16]. Suicidal history was assessed using the colombia suicide history form, while current suicidal ideation was assessed using the Beck Suicide Intent Scale (BSIS) and the scale for suicidal ideation [17-19]. Childhood trauma was assessed using the Childhood Trauma Questionnaire (CTQ) [12]. The CTQ has been validated in clinical and non-clinical settings and possesses excellent test-retest stability [12]. For these reasons, it currently remains the primary assessment of Childhood Maltreatment (CM), despite more novel instruments being developed [9]. The CTQ assesses patients for five subtypes of childhood trauma, including Emotional Abuse (EA), Physical Abuse (PA), Sexual Abuse (SA), Emotional Neglect (EN) and Physical Neglect (PN). Assessment scores are rated on a likert scale from 1 (“never true”) to 5 (“very often true”), by which a higher score indicates a higher severity of trauma.
Neuropsychological assessment: Cognitive control was assessed using the stroop color test, decision-making using the iowa gambling task, and verbal fluency using the FAS verbal fluency test [20-22]. Lastly, verbal IQ was assessed by the National Adult Reading Test (NART) [23,24]. The order of these assessments was randomized.
Data Analysis
Categorical variables in this analysis are presented as percentages, whereas quantitative variables are presented as means with standard deviations. Shapiro-Wilk’s test was used to examine the normality of continuous variables. Sociodemographic and clinical variables were compared using a t-test analysis. Lastly, a Chi-square test was used to compare qualitative values. All analyses were performed using SPSS (version 24.0; SPSS, Inc., Chicago, IL). An alpha threshold of 0.05 was set a priori. Participants were assigned subject groups based on their history of childhood trauma (Childhood Trauma: total CTQ score of >51; No childhood trauma: total CTQ score of <51). The association between childhood trauma and neuropsychological features was investigated using a t-test to compare the two groups across the neuropsychological test scores. A linear regression analysis examined potential confounding factors including age, gender, severity of depression, medication use, and previous history of suicide attempts.
Results
Demographic and clinical characteristics
Participants, primarily women (73.6%), with a history of late-life depression were included in the present study (Table 1). Patients with a history of childhood trauma (n=30) compared to those without a history of childhood trauma (n=39) did not significantly differ on any of the demographic and clinical variables, except for antidepressant use. Subjects in the no childhood trauma group reported taking antidepressants (p=0.020).
Association between childhood trauma and neuropsychological features (Table 1)
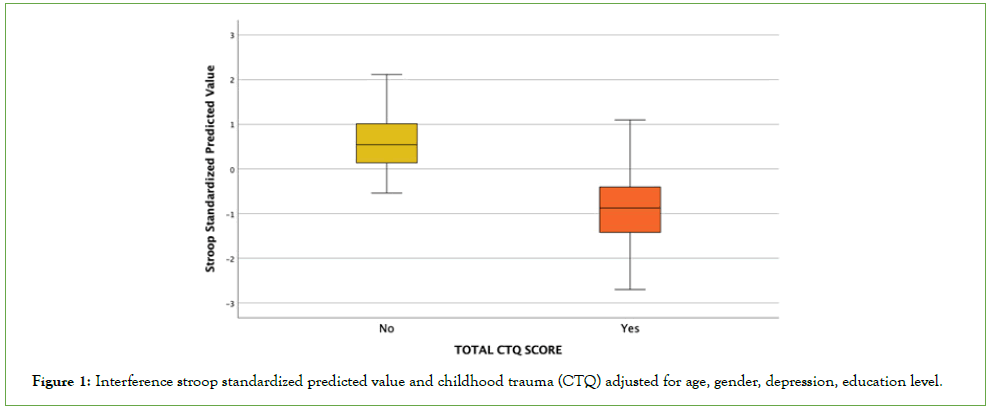
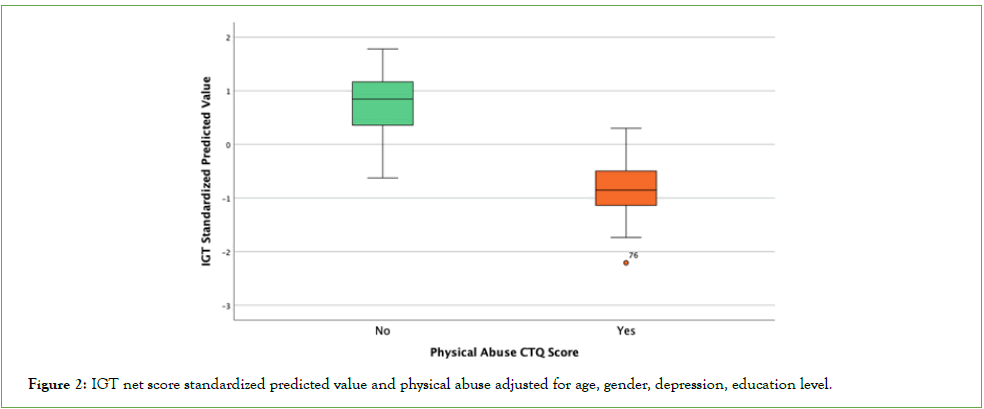
Participants with a history of childhood trauma took significantly less time to execute the interference part of the stroop color and word test than those without CT (F=5.06; t=2.08; df=67; p =0.041) (Figure 1). Patients with a history of physical abuse had significantly lower IGT net scores compared to patients with no history of PA (F=.654; t=2.49; df=65; p=0.015) (Figure 2). In addition, emotional neglect was associated with a lower reaction time at the Stroop Color and Word Test (SCWT) (F=3.20; t=2.13; df=67; p=0.037) and higher semantic verbal fluency score (F=1.47; t=-2.35; df=67; p=0.021). These results remained significant even after controlling for confounding factors including age, gender, severity of depression, antidepressant medication, and history of previous suicide attempts. There were no statistically significant neuropsychological differences across groups with and without emotional abuse, sexual abuse and physical neglect.
| |
No childhood trauma CTQ total <51 n=39 |
No childhood trauma CTQ total <51 n=39 |
Statistics | F | p-value |
|---|---|---|---|---|---|
| Demographic and clinical variables | |||||
| Women, n (%) | 29 (54.7%) | 24 (45.3%) | X2=0.30 | - | 0.58 |
| Age (years), mean (SD) | 67.3 (6.7) | 66.13 (5.87) | - | 0.710 | 0.43 |
| Education level, (NART score, mean (SD) |
72.8 (16.6) | 70.53 (16.58) | - | 0.10 | 0,56 |
| HAMD-17 items total score, mean (SD) |
7.4 (6.2) | 5.3 (4.8) | - | 0.399 | 0.12 |
| Previous history of suicide attempts, n (%) |
19 (67.9%) | 9 (32.1%) | X2=2.46 | - | 0.11 |
| Antidepressants, n (%) | 34 (87.2%) | 19 (63.3%) | X2=5.41 | - | 0.02 |
| Antipsychotics, n (%) | 22 (56.4%) | 13 (43.3%) | X2=1.16 | - | 0.28 |
| Mood stabilizer, n (%) | 2 (5.1%) | 2 (6.7%) | X2=0.07 | - | 0.78 |
| Neuropsychological variables | |||||
| IGT net score, mean (SD) |
10.4 (30.5) | 2.2 (22) | - | 2.063 | 0.21 |
| TMT B/A score, mean (SD) |
4.7 (14.4) | 2.5 (1.0) | - | 2.324 | 0.40 |
| HSCT B time (ms), mean (SD) |
223.8 (164.6) | 182.3 (103) | - | 0.622 | 0.23 |
| SCWT interference time score (ms), mean (SD) |
92.3 (58.5) | 67.5 (32.2) | - | 5.061 | 0.041 |
| Phonemic verbal fluency test, mean (SD) |
19.7 (7.6) | 20.6 (6.8) | - | 0.006 | 0.616 |
| Semantic verbal fluency test, mean (SD) |
24.4 (9.8) | 25.8 (7.5) | - | 0.627 | 0.530 |
Table 1: MClinical and neuropsychological features of childhood trauma (according to CTQ total scores) in elderly population with a history of late-life depression.
Figure 1: Interference stroop standardized predicted value and childhood trauma (CTQ) adjusted for age, gender, depression, education level.
Figure 2: IGT net score standardized predicted value and physical abuse adjusted for age, gender, depression, education level.
Secondary analyses
Further subject group analysis, based on a history of suicide attempts, revealed that in patients with a history of suicide attempts, EN was associated with a higher semantic verbal fluency score (p=0.021), compared to those without EN. This association was not found in the group without a history of suicide attempts. Additionally, in the group of patients with no history of suicide attempts, those who experienced PA had significantly lower IGT net scores compared to patients with no history of PA (p=0.015). This result was not found in the group with a history of suicide attempts.
Discussion
This study aims to differentiate neurocognitive pathways through a history of childhood abuse and neglect. To our knowledge, this is the first exploratory study to document an association between childhood trauma and cognition in late-life depression. The results from this study demonstrate that CT is associated with strong cognitive performance, based on a sample of older patients presenting with a history of late-life depression. Furthermore, the results illustrate that the specific impact on cognitive performance varies depending on the type of CT that was experienced.
Our results demonstrate that individuals who experienced physical abuse had lower net scores on the iowa gambling task. A study by Tjoelker, et al. [25]. found childhood PA and EN to be associated with decreased interference control. This deficit in executive functioning may be explained by a stress and inflammatory response to child abuse [26]. Furthermore, a study by Guillaume, et al. [27] reveals that patients with a history of suicide attempts who experienced sexual abuse and emotional neglect had lower IGT scores. Interestingly, our results demonstrate the contrary. Those without a history of suicide attempts but with a history of PA had lower IGT net scores than those without PA. These findings suggest that trauma may significantly impact decision-making regardless of other confounders.
Our results further demonstrate an association between total CTQ score and the stroop color and word test. Patients with a history of childhood trauma had a lower delay in response time, indicated by a lower interference score. These results illustrate that older adults with a history of CT have higher cognitive inhibition and lower levels of impulsivity compared to patients without a history of CT. This decrease in impulsivity may be explained by the impact of CT on neurocognitive regions, such as the dorsomedial prefrontal cortex (dmPFC), a region that is crucial to cognitive control. This theory is supported by a recent study by Ross, et al. [28] which demonstrates that exposure to PA during childhood increases the activation of the dmPFC regions during failed inhibition amongst adolescents.
Contrary to findings in our study, current literature supports the theory that patients with a history of CT have impaired cognitive inhibition and higher impulsivity. A study by Zhai, et al. [29] found that inhibitory control, modulated by the anterior cingulate cortex, was indicated by fewer errors on the SCWT. In these findings, childhood trauma is illustrated to potentially portend neurodevelopmental changes that impede the recruitment of control-associated ACC-functioning during distress [29]. These findings give an argument for the possible anatomical discrimination between regions primarily implicated in the IGT, such as the ventral prefrontal cortex, as well as regions significantly implicated in cognitive control, such as the dorsal prefrontal cortex [30].
These findings contribute to Brokke, et al.’s [10] theory of the role of dissociative behaviors in cognitive processing, amongst those with a history of trauma. Our findings of a lower delay in response time, indicated by a lower interference score, suggest that disassociation may create a top-down control effect in which external distractions are reduced during informatin processing [31]. Although the mediating role of dissociate behaviors and suicidal behaviors remains unclear, one potential explanation may be that diassociative behaviours are a marker of cognitive fragmentation, impaired emotional processing and problem solving. These impairments may contribute to maladaptive coping responses, exacerbating symptoms of depression and eventually suicidal behaviors in adulthood, in the face of adverse life events [32-35].
Conclusion
A previous experience of childhood trauma may impact crucial cognitive functions, such as cognitive control and decision-making, in late-life depression. Patients with a history of physical abuse demonstrated low decision-making scores and patients with a history of emotional neglect demonstrated good cognitive control. The long-term impact of childhood trauma on health outcomes in older adulthood remains understudied, despite current literature suggesting that adverse childhood experiences may have a negative impact on cognition, even years after their occurrence. There is a consequential need for further research that clarifies the mechanisms that moderate or mediate this phenomenon. Advanced research on the impact of childhood trauma on neuropsychological mechanisms in older adulthood will foster the development of optimized interventions for late-life depression and cognitive decline. As a result, effective cognitive interventions may prevent adverse outcomes including psychiatric disorders and suicidality.
Limitations
There are several limitations to this study which must be underlined. Firstly, the population for this study ranges from ages 60-85 years old. This older age cohort may skew the neurocognitive findings that we relate to childhood trauma in our study, as there may be many additional life experiences, beyond CT, that may contribute to or account for changes in neurocognition. A prospective longitudinal study from the onset of CT to late life may lead to more accurate data to examine the relationship between neurocognitive changes and childhood trauma. Furthermore, the small sample size of this study limits statistical power and the generalizability of findings. A replication of this study with larger patient groups is required to strengthen the study’s external validity. Lastly, as trauma history and patient controls represent heterogeneous groups, there is a risk of variable findings based on sample selection. Consequentially, the findings from this study may not be generalizable to all forms of trauma-related outcomes.
Acknowledgements
This study was supported by grants from the American Foundation for Suicide Prevention (AFSP) to Stéphane Richard-Devantoy (AFSP Young Investigator Grant YIG-0-118-13). The AFSP had no further role in study design, the collection, analysis, and interpretation of data, the writing of the report, or in the decision to submit the paper for publication.
Conflicts of Interest
NoneAuthor Contributions
S.R.D. obtained funding. S.R.D. designed the study and oversaw subject recruitment and data collection. N.C. performed the statistical analyses with statistical review by S.R.D. and G.T.
N.C. and L.O. drafted the manuscript, which was edited and finalized by all authors.
References
- La Greca AM, Boyd BA, Jaycox LH, Kassam-Adams N, Mannarino AP, Silverman WK, et al. Children and trauma: Update for mental health professionals. Washington DC: APA Presidential Task Force PTSD Trauma in Children and Adolescents. 2008.
- Petkus AJ, Lenze EJ, Butters MA, Twamley EW, Wetherell JL. Childhood trauma is associated with poorer cognitive performance in older adults. J Clin Psychiatry. 2017;79(1):2579.
- De Bellis MD. Developmental traumatology: The psychobiological development of maltreated children and its implications for research, treatment, and policy. Dev Psychopathol. 2001;13(3):539-564.
- Danese A, McEwen BS. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol Behav. 2012;106(1):29-39.
- Merrick MT, Ports KA, Ford DC, Afifi TO, Gershoff ET, Grogan-Kaylor A. Unpacking the impact of adverse childhood experiences on adult mental health. Child Abuse Negl. 2017;69:10-19.
- Richard-Devantoy S, Berlim MT, Jollant F. A meta-analysis of neuropsychological markers of vulnerability to suicidal behavior in mood disorders. Psychological medicine. 2014;44(8):1663-1673.
- Angelakis I, Gillespie EL, Panagioti M. Childhood maltreatment and adult suicidality: A comprehensive systematic review with meta-analysis. Psychol Med. 2019;49(7):1057-1078.
- Angelakis I, Austin JL, Gooding P. Association of childhood maltreatment with suicide behaviors among young people: A systematic review and meta-analysis. JAMA Netw Open. 2020;3(8):2012563.
- Su Y, D'Arcy C, Yuan S, Meng X. How does childhood maltreatment influence ensuing cognitive functioning among people with the exposure of childhood maltreatment? A systematic review of prospective cohort studies. J Affect Disord. 2019;252:278-293.
- Brokke SS, Bertelsen TB, Landrø NI, Haaland VØ. The effect of sexual abuse and dissociation on suicide attempt. BMC Psychiatry. 2022;22(1):29.
- Korten NC, Penninx BW, Kok RM, Stek ML, Oude Voshaar RC, Deeg DJ, et al. Heterogeneity of late-life depression: Relationship with cognitive functioning. Int Psychogeriatr. 2014;26(6):953-963.
- Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, et al. Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiatry. 1994;151(8):1132-1136.
- Grassi-Oliveira R, Stein LM, Pezzi JC. Translation and content validation of the Childhood Trauma Questionnaire into Portuguese language. Revista de saude publica. 2006;40:249-255.
- Kenny D, Bekh B, Bleijenberg G, Bohus M, Carpenter L, Carr A, et al. Minimization of Childhood Maltreatment Is Common and Consequential: Results from a Large, Multinational Sample Using the Childhood Trauma Questionnaire.
- First MB. Structured clinical interview for DSMâ?IVâ?TR axis I disorders, research version, patient edition (SCIDâ?I/P). Biom Res. 2002.
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23(1):56.
- Posner K, Oquendo MA, Gould M, Stanley B, Davies M. Columbia Classification Algorithm of Suicide Assessment (C-CASA): Classification of suicidal events in the FDA’s pediatric suicidal risk analysis of antidepressants. Am J Psychiatry. 2007;164(7):1035-1043.
- Beck AT, Resnik AT, Lettieri DJ. Suicide intent scale.
- Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: The Scale for Suicide Ideation. J Consult Clin Psychol. 1979;47(2):343.
- Godefroy O. Fonctions exécutives et pathologies neurologiques et psychiatriques: Évaluation en pratique clinique. Groupe de Boeck; 2008.
- Bechara A, Damasio H, Damasio AR, Lee GP. Different contributions of the human amygdala and ventromedial prefrontal cortex to decision-making. J Neurosci. 1999;19(13):5473-5481.
- Duff K, Schoenberg MR, Scott JG, Adams RL. The relationship between executive functioning and verbal and visual learning and memory. Arch Clin Neuropsychol. 2005;20(1):111-122.
- Beardsall L, Brayne C. Estimation of verbal intelligence in an elderly community: A prediction analysis using a shortened NART. Br J Clin Psychol. 1990;29(1):83-90.
- Mackinnon A, Mulligan R. The estimation of premorbid intelligence levels in French speakers. Encephale. 2005;31(1 Pt 1):31-43.
- Tjoelker FM, Jeuring HW, Aprahamian I, Naarding P, Marijnissen RM, Hendriks GJ, et al. The impact of a history of child abuse on cognitive performance: A cross-sectional study in older patients with a depressive, anxiety, or somatic symptom disorder. BMC Geriatr. 2022;22(1):377.
- Teicher MH, Andersen SL, Polcari A, Anderson CM, Navalta CP, Kim DM. The neurobiological consequences of early stress and childhood maltreatment. Neurosci Biobehav Rev. 2003;27(1-2):33-44.
- Guillaume S, Perroud N, Jollant F, Jaussent I, Olié E, Malafosse A, et al. HPA axis genes may modulate the effect of childhood adversities on decision-making in suicide attempters. J Psychiatr Res. 2013;47(2):259-265.
- Ross MC, Heilicher M, Cisler JM. Functional imaging correlates of childhood trauma: A qualitative review of past research and emerging trends. Pharmacol Biochem Behav. 2021;211:173297.
- Yip SW, Lacadie CM, Sinha R, Mayes LC, Potenza MN. Childhood trauma moderates inhibitory control and anterior cingulate cortex activation during stress. Neuroimage. 2019;185:111-118.
- Gläscher J, Adolphs R, Damasio H, Bechara A, Rudrauf D, Calamia M, et al. Lesion mapping of cognitive control and value-based decision making in the prefrontal cortex. Proc Natl Acad Sci. 2012;109(36):14681-14686.
- White SF, Costanzo ME, Thornton LC, Mobley AM, Blair JR, Roy MJ. Increased cognitive control and reduced emotional interference is associated with reduced PTSD symptom severity in a trauma-exposed sample: A preliminary longitudinal study. Psychiatry Res Neuroimaging. 2018;278:7-12.
- Boyer SM, Caplan JE, Edwards LK. Trauma-related dissociation and the dissociative disorders: Neglected symptoms with severe public health consequences. Dela J Public Health. 2022;8(2):78.
- Nester MS, Brand BL, Schielke HJ, Kumar S. An examination of the relations between emotion dysregulation, dissociation, and self-injury among dissociative disorder patients. Eur J Psychotraumatol. 2022;13(1):2031592.
- Shim S, Kim D, Kim E. Dissociation as a mediator of interpersonal trauma and depression: adulthood versus childhood interpersonal traumas3. BMC Psychiatry. 2024;24(1):764.
- Xiang X, Wang X. Childhood adversity and major depression in later life: A competingâ?risks regression analysis. Int J Geriatr Psychiatry. 2021;36(1):215-223.
Citation: Devantoy SR, Conde N, Osborne L, Inja A, Bertrand JA, Turecki G (2025). From Hurt to Harm: How Childhood Trauma Shapes Cognitive Control and Decision Making in Late-Life Depression. J Psychiatry. 28:774.
Copyright: © 2025 Devantoy SR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.