Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- Google Scholar
- SHERPA ROMEO
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2025) Volume 13, Issue 5
Extracranial-Intracranial Bypass Surgery for Symptomatic Middle Cerebral Artery Occlusion-How to Prevent Intraoperative Complications
Chun-Chung Chen1,2,3, Chun Wei Tseng2, Charlton Chen-Ting Cheng2, Chih-Hsiu Tu2, Chun-Jen Chang2, Yu-Chung Juan2, Jeng-Hung Guo2, Der-Yang Cho2, Wei-Lin Hsu2 and Chien-Tung Yang2*2Department of Neurosurgery, China Medical University Hospital, Taichung, Taiwan
3Department of Neuroscience and Brain Disease, China Medical University, Taichung, Taiwan
Received: 22-Apr-2024, Manuscript No. JVMS-24-25536; Editor assigned: 25-Apr-2024, Pre QC No. JVMS-24-25536 (PQ); Reviewed: 09-May-2024, QC No. JVMS-24-25536; Revised: 10-Oct-2025, Manuscript No. JVMS-24-25536 (R); Published: 17-Oct-2025, DOI: 10.35248/2329-6925.25.13.599
Abstract
This retrospective, single-center study, conducted without randomization, aimed to evaluate the management of patients with symptomatic total occlusion of the Middle Cerebral Artery (MCA). The study focused on the effectiveness of Extracranial–Intracranial (EC–IC) bypass as a treatment for those with atherosclerotic MCA total occlusion, ischemic symptoms such as Transient Ischemic Attacks (TIAs), or inadequate cerebral hemodynamics despite maximal medical therapy. A total of 94 patients, who met specific criteria including experiencing ischemic syndromes (e.g., TIA) associated with atherosclerotic MCA total occlusion confirmed by radiological assessment and showing an insufficient response to optimal medical therapy, were included. This insufficiency was indicated by the potential recurrence of TIAs or ischemic stroke despite maximal medical treatment. Postoperatively, three patients experienced Intracerebral Hemorrhage (ICH), while none suffered from an ischemic stroke either within the first 30 days or over the following 24 months. Post-operative imaging, which included MRI (MR angiography) or four-vessel digital subtraction angiography, demonstrated a 100% patency rate in the Superficial Temporal Artery-Middle Cerebral Artery (STA-MCA) anastomosis. The 30-day ischemic stroke rate post-EC-IC bypass in our series was 3.1%, and this rate persisted at 3.1% even after 24 months in patients with atherosclerotic MCA total occlusion and hemodynamic impairment. The lower postoperative stroke rate can likely be credited to our comprehensive perioperative management, including the continuation of antiplatelet therapy and rigorous blood pressure control. However, to firmly establish the effectiveness of the EC-IC bypass as a viable intervention, larger-scale studies are necessary.
Keywords
MCA occlusion; EC-IC bypass; Hemodynamic impairment; Stroke
Introduction
Patients experiencing symptomatic occlusion in the Internal Carotid Artery (ICA) or Middle Cerebral Artery (MCA) face an annual risk of recurrent stroke exceeding 10%. Moreover, a subset of these patients demonstrates cerebral hemodynamic insufficiency, leading to a significantly higher 2-year risk of ischemic stroke despite medical therapy. One potential treatment approach addresses hemodynamic ally compromised ICA or MCA occlusions by restoring blood flow through superficial temporal artery anastomosis to the MCA. However, clinical trials have yielded mixed results in proving the efficacy of EC-IC (Extracranial-Intracranial) bypass surgery. Recent studies, such as the Carotid and Middle Cerebral Artery Occlusion Surgery Study (CMOSS) trial, have not established the efficiency of EC-IC bypass surgery in ICA or MCA occlusion. Nonetheless, subgroup analyses from CMOSS indicate a more favorable outcome in MCA occlusion patients post-bypass surgery compared to those with ICA occlusion. This benefit, however, is offset by a higher incidence of postoperative complications, which reduces the overall advantages of the bypass surgery. In individuals with symptomatic total MCA occlusion, the prognosis without surgical intervention is notably worse than in those with ICA occlusion. According to the CMOSS findings, patients with MCA occlusion may experience improved outcomes post-EC-IC bypass if the rate of intraoperative complications can be minimized. We have reported our preliminary results on EC-IC bypass surgery for MCA occlusion patients with a postoperative recurrent stroke rate of 0% in our report [1].
Consequently, we present a retrospective, single-center, nonrandomized study focusing on the management of symptomatic total MCA occlusion disease. This study evaluates the EC-IC bypass surgery as an intervention for individuals with atherosclerotic total MCA occlusion, ischemic symptoms (such as Transient Ischemic Attacks (TIAs) or poor cerebral hemodynamics unresponsive to maximal medical treatment. Additionally, our study discusses perioperative strategies employed to prevent and mitigate intraoperative complications [2].
Materials and Methods
Patients and inclusion criteria
Between October 2006 and February 2021, patients diagnosed with symptomatic total occlusion of the Middle Cerebral Artery (MCA) and poor hemodynamic parameters underwent a series of diagnostic procedures. These included Diffusion-Weighted Imaging (DWI) brain MRIs to identify any new or existing ischemic strokes, assess the condition of major cerebral vessels, and prepare for the standard end-to-side anastomosis of the superficial temporal artery to the M4 segment of the MCA. Digital Subtraction Angiography (DSA) was also used to evaluate the state of major cerebral vessels in all patients. Cerebral hemodynamic parameters were measured using CT perfusion techniques, as outlined in the 'CT perfusion techniques' section. The patients' neurological status was assessed using the modified Rankin Scale (mRS) before surgery, one month post-surgery, and again at 24 months post-surgery. Imaging assessments, including DSA or MRA, were repeated one month after surgery [3].
The criteria for considering the STA-MCA bypass procedure aligned with established standards. These included patients exhibiting ischemic symptoms (such as Transient Ischemic Attacks (TIA)) associated with atherosclerotic total MCA occlusion disease (confirmed by radiological assessment), nonresponsive to optimal medical therapy (e.g., antiplatelet therapy), experiencing recurrent TIA or ischemic stroke despite maximal medical therapy, demonstrating poor cerebral perfusion on CT imaging, and exhibiting Regional Cerebrovascular Reactivity (rCVR) of less than 20% during acetazolamide challenge. Patients with acute ischemic stroke or other significant medical conditions were excluded. Those presenting solely with TIA symptoms without compromised rCVR due to MCA total occlusive disease were also excluded [4].
All enrolled patients received optimized medical treatment focused on managing vascular risk factors. This included controlling low-density lipoprotein cholesterol levels and hypertension with medications, promoting smoking cessation through counseling or oral cessation aids, and managing excess weight through behavioral changes or medications. In addition, patients were prescribed aspirin (100 mg/day) or clopidogrel (75 mg/day). Surgical intervention was performed within 7 days of randomization by certified surgeons [5].
Preoperative and perioperative management
Pre-op:
- Continue the use of antiplatelet medications to prevent ischemic stroke.
- Maintain any other antithrombotic therapies, particularly oral anticoagulants, throughout the surgical procedure.
Perioperative:
- Keep intraoperative blood pressure at the same level as it was pre-anesthesia.
- Limit ischemia duration to less than 30 minutes during the anastomosis procedure.
- Implement strict hemostasis protocols to prevent postoperative hemorrhage.
- Ensure that intraoperative arterial PCO and PCO targets are maintained between 35 and 40 mm Hg.
Post-op:
- Control blood pressure to below 140 mmHg to prevent hyper perfusion and postoperative haemorrhage.
CT Perfusion techniques
Resting CT perfusion studies were performed using a CT scanner equipped with an 8-detector array (Light speed; GE Healthcare, Milwaukee, WI, USA). Thirty minutes after the initial perfusion study, all patients underwent an acetazolamide challenge.
The same procedures were repeated six months post-surgery. Maps showing regional Cerebral Blood Flow (rCBF) were generated using a workstation (Advantage Windows; GE Healthcare) with CT perfusion software. Regions of Interest (ROIs) were designated for calculating the absolute value of Cerebral Blood Flow (CBF) in mL/100 mg/min from each ROI. regional Cerebrovascular Reactivity (rCVR) was calculated as a percentage using the formula: ((acetazolamide challenge rCBF–resting rCBF)/resting rCBF) × 100%.
For statistical analysis, sequential changes in the NIHSS (National Institutes of Health Stroke Scale) and Barthel Indices were assessed using Analysis of Variance (ANOVA) followed by the Fisher exact test. Statistical significance was determined at P ≤ 0.05 [6].
Results
In the study, a total of 94 patients were involved, consisting of 64 males and 30 females. The mean age of the participants was 56.3 ± 14.1 years. The average intraoperative temporary occlusion time was 23.5 minutes. Among these patients, three experienced postoperative Intracerebral Hemorrhage (ICH) during the study. The stroke rate within 30 days post-surgery was recorded at 3.1%. Over the 24-month follow-up period, the risk of recurrent stroke for patients who underwent EC-IC bypass procedures was 0%. However, the overall complication rate was observed to be 3.1% (3 out of 94 patients). Post-operative imaging follow up, which included MRI (MR angiography) and four-vessel digital subtraction angiography, demonstrated 100% patency of the STA-MCA anastomosis in all patients (Figure 1) [7].
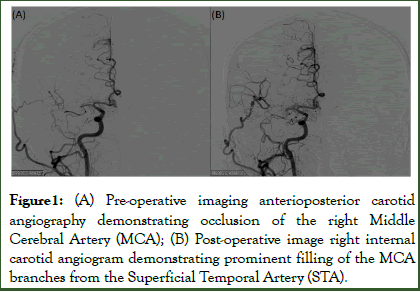
Figure1: (A) Pre-operative imaging anterioposterior carotid angiography demonstrating occlusion of the right Middle Cerebral Artery (MCA); (B) Post-operative image right internal carotid angiogram demonstrating prominent filling of the MCA branches from the Superficial Temporal Artery (STA).
Discussion
Patients with Intracranial Atherosclerotic Disease (ICAD) who exhibit hemodynamic impairment tend to face a higher annual stroke risk. In cases of Middle Cerebral Artery (MCA) occlusion, there is often associated hemodynamic impairment in the distal cerebral circulation, primarily due to limited collateral pathways, typically only pial or meningeal to pial collaterals. However, with Internal Carotid Artery (ICA) occlusion, the presence of the circle of Willis and external to internal carotid collaterals often maintains normal perfusion pressure despite of the occlusion. This results in a relatively higher occurrence of hemodynamic compromise in symptomatic MCA stenosis patients. Consequently, the prognosis is generally worse for patients with MCA occlusion compared to those with ICA occlusion or MCA stenosis. Current treatment options for Intracranial Atherosclerotic Disease (ICAD) encompass antithrombotic therapies, such as antiplatelet agents, and advanced techniques including angioplasty and stenting. However, these approaches are not suitable for cases involving total occlusion of the Middle Cerebral Artery (MCA), resulting in a notable gap between treatment and ideal result for these patients [8].
Clinical trials, such as the EC-IC bypass study, have failed to demonstrate the benefits of bypass surgery in symptomatic patients with atherosclerotic stenosis or occlusion in the ICA and MCA. Criticism of this trial stems from its inclusion of patients with atherosclerotic stenosis who might not benefit from bypass surgery, and the failure to specifically identify patients with hemodynamic insufficiency who could potentially benefit most from such surgery. Other trials, like the Carotid Occlusion Surgery Study (COSS) in North America, were halted prematurely due to perceived lack of effectiveness. There have been debates about whether reducing perioperative risks could make bypass surgery more effective, considering the high postoperative stroke rates observed in these trials [9].
Additionally, the CMOSS trial did not show any benefits of bypass surgery in patients with hemodynamically compromised occlusions in the Internal Carotid Artery (ICA) or Middle Cerebral Artery (MCA). This led to ongoing debates about whether minimizing perioperative risks could potentially improve the efficacy of bypass surgery, especially in light of the higher postoperative stroke rates observed in both the COSS and CMOSS trials [10].
In our study, postoperative Intracerebral Hemorrhage (ICH) occurred in three patients, representing 3.1% of cases, which contributed to a 30-days complication rate of 3.1%. Notably, over the two-year follow-up period, there were no new cases of ischemic stroke, suggesting a lower incidence rate compared to what was observed in the COSS and CMOSS trials. This favorable outcome may be attributed to our rigorous perioperative management strategies, which included continuous preoperative antiplatelet therapy, maintaining optimal blood pressure during anesthesia, reducing ischemia time during anastomosis, and strict control of blood pressure after the surgery [11].
While the ongoing use of antiplatelet therapy did result in a 3% increase in postoperative bleeding in our series, it effectively prevented ischemic strokes post-surgery, with a 0% occurrence rate within the first 30 days following the procedure. Despite the increased risk of perioperative hemorrhage associated with continuous antiplatelet therapy, we believe that this risk is manageable through stringent hemostasis practices. It's noteworthy that the incidents of postoperative ICH in our study were confined to the initial 20 cases, with no further occurrences thereafter. The strict control of blood pressure postoperatively, aimed at preventing hyperperfusion, likely played a role in reducing the rates of postoperative ICH [12].
In our study, the average intraoperative temporary occlusion time was 23.5 minutes, which is below the 30 minutes threshold and aligns with the 21.0 minute average reported in the CMOSS trial. This finding is significant given the ongoing debate about longer ischemia times, such as the 55.9 minutes noted in the COSS trial, which were associated with higher postoperative stroke rates. Our results indicate that an ischemia time of less than 30 minutes appears to be adequate in preventing ischemic complications [13].
Patients with symptomatic Middle Cerebral Artery (MCA) occlusion and compromised regional Cerebrovascular Reactivity (rCVR) are known to have an annual ischemic stroke rate as high as 35.6%. In contrast, our study showed that both the 30- day and 24-month stroke rates were 3.1%. These lower rates indicate a significant reduction in recurrent strokes following bypass surgery, suggesting that EC-IC bypass surgery could be a viable option for improving outcomes in patients with atherosclerotic total occlusion of the MCA [14].
Conclusion
After undergoing EC-IC bypass surgery in our study, the rate of ischemic strokes within 30 days was noted to be 3.1%. Impressively, this rate remained consistent at 3.1% even after a 24-month period for patients with atherosclerotic total occlusion of the Middle Cerebral Artery (MCA) and hemodynamic impairment. The lower postoperative stroke rate observed can likely be attributed to our comprehensive perioperative management strategy, which included the continued use of antiplatelet therapy and meticulous blood pressure control.
However, due to the limitations of our study, which include a small and heterogeneous patient sample, it's difficult to draw definitive conclusions about the broad efficacy of this intervention. Therefore, further research involving a larger and more diverse group of patients is crucial to fully assess the effectiveness of EC-IC bypass surgery in treating such conditions.
References
- Grubb Jr RL, Derdeyn CP, Fritsch SM. Importance of hemodynamic factors in the prognosis of symptomatic carotid occlusion. JAMA.1998;280(12):1055-1060.
- Kern R, Steinke W, Daffertshofer M, Prager R, Hennerici M. Stroke recurrences in patients with symptomatic vs. asymptomatic middle cerebral artery disease. Neurology. 2005;65(6):859-864.
- Flaherty ML, Flemming KD, McClelland R, Jorgensen NW, Brown Jr RD. Population-based study of symptomatic internal carotid artery occlusion: Incidence and long-term follow-up. Stroke. 2004;35(8):e349-e352.
- Reynolds MR, Derdeyn CP, Grubb Jr RL, Powers WJ, Zipfel GJ. Extracranial-intracranial bypass for ischemic cerebrovascular disease: what have we learned from the Carotid Occlusion Surgery Study? Neurosurg Focus. 2014;36(1):9.
- Grubb Jr RL, Derdeyn CP, Videen TO, Carpenter DA, Powers WJ. Relative mean transit time predicts subsequent stroke in symptomatic carotid occlusion. J Stroke Cerebrovasc Dis. 2016;25(6):1421-1424.
- Vilela MD, Newell DW. Superficial temporal artery to middle cerebral artery bypass: past, present, and future. Neurosurg Focus. 2008;24(2):2.
- Ma Y, Wang T, Wang H, Amin-Hanjani S, Tong X, Wang J, et al. Extracranial-Intracranial Bypass and Risk of Stroke and Death in Patients With Symptomatic Artery Occlusion. CMOSS Randomized Clin Trial JAMA. 2023;330(8):704-714.
- Chou CW, Chang JH, Lin SL, Cho DY, Cheng YW, Chen CC. Extracranial–Intracranial (EC–IC) bypass of symptomatic middle cerebral artery (MCA) total occlusion for haemodynamic impairment patients. Brit J Neuro surg. 26:823-826.
- Arkus H, Cullinane M. Severely impaired cerebrovascular reactivity predicts stroke and TIA risk in patients with carotid artery stenosis and occlusion. Brain. 2001;124:457–467.
- Iyazawa N, Hashizume K, Uchida M, Nukui H. Long-term follow up of asymptomatic patients with major artery occlusion: rate of symptomatic change and evaluation of cerebral hemodynamics. Am J Neuroradiol 2001;22:243–247.
- Derdeyn CP, Powers WJ, Grubb RL. Hemodynamic effects of middle cerebral artery stenosis and occlusion. AJNR Am J Neuroradiol 1998;19:1463-1469.
- Importance of hemodynamic factors in the prognosis of symptomatic carotid occlusion
- Schmiedek P, Piepgras A, Leinsinger G, Kirsch CM, Einhupl K. Improvement of cerebrovascular reserve capacity by EC-IC arterial bypass surgery in patients with ICA occlusion and hemodynamic cerebral ischemia. J Neurosurg. 1994;81(2):236-244.
- Powers WJ, Clarke WR, Grubb Jr RL, Videen TO, Adams Jr HP, Derdeyn CP. COSS Investigators. Extracranial-intracranial bypass surgery for stroke prevention in hemodynamic cerebral ischemia: The Carotid Occlusion Surgery Study randomized trial. JAMA. 2011;306:1983-1992.
Citation: Chen CC, Tseng CW, Cheng CCT, Tu CH, Chang CJ, Juan YC, et al. (2025) Morphological Features of Abdominal Aortic Aneurysms and Association with Biomechanical Assessments of Aneurysm Wall Segments. J Vasc Med Surg. 13:599.
Copyright: © 2025 Chen CC, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

