Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2023) Volume 14, Issue 5
Exploring the Knowledge, Attitudes and Practices of Perinatal Women towards Hypertensive Disorders in Pregnancy (HDP) and its Implication for the Implementation of Maternal Mental Health Services (MMHS): A Quantitative Descriptive Study
Mustapha Karikari1*, Joyce BP Pwavra2, Victor Adeleke2, Jane Okarfo Akunna2 and Ernest Opoku-Antwi22Department of Maternal and Child Health, School of Nursing and Midwifery, University of Ghana, Accra, Ghana
Received: 14-Aug-2023, Manuscript No. JCRB-23-22590; Editor assigned: 17-Aug-2023, Pre QC No. JCRB-23-22590 (PQ); Reviewed: 30-Aug-2023, QC No. JCRB-23-22590; Revised: 06-Sep-2023, Manuscript No. JCRB-23-22590 (R); Published: 13-Oct-2023, DOI: 10.35248/2155-9627.23.14.473
Abstract
Background: Hypertensive Disorders in Pregnancy (HDP) refer to a spectrum of conditions of vascular origin and systemic manifestations caused by a mixture of genetic and acquired factors, which occur during pregnancy and represent the most common medical complications of pregnancy with a reported incidence of 5%-10%. HDP greatly impacts birth outcome and complicates almost a tenth of all pregnancies globally. This poses a great deal of psychological distress to the mother and the developing foetus. The aim of this study was to explore the knowledge, attitudes, and practices of perinatal women regarding hypertensive disorders that occur during pregnancy and its implication for the implementation of maternal mental health services.
Method: A self-structured questionnaire was used as a guide to solicit information from the participants at a single point in time, with focus on three main thematic areas that include knowledge of participants on hypertensive disorders in pregnancy, attitudes, and practices of perinatal women towards hypertensive disorders in pregnancy as well as the access to maternal mental health services during the perinatal period. Convenience sampling technique was employed to select participants. A total of 267 subjects participated in the study. All pregnant women from Gravida 2 Para 1 and above as well as those who experienced hypertensive disorders such as PIH in their previous pregnancies and are presently attending ANC were included in the study whiles first time perinatal women without a history of hypertension were excluded. The data collected was analyzed with Microsoft Excel and Statistical Package for Social Sciences (SPSS) (Version 24) software. Basic descriptive quantitative analysis was used based on frequency tables, pie chart and graphical illustration to interpret the data.
Results: The findings revealed that most of the study participants (52.2%) had inadequate knowledge of Hypertensive disorders in pregnancy regarding the causes, risk factors and clinical manifestations of HDP. Despite their insufficient knowledge about the range of complications that may emanate from HDP, all the study participants identified stroke (cardiovascular accident) as a common effect of HDP whiles about 87.6% of the participants labelled seizures as the most common demonstrable consequence. This finding also resonates with some earlier reports on the subject matter. It is imperative to note that the study did not prioritize identifying respondents with a history of any complications resulting from HDP. Interestingly, the study revealed that mental health screening did not form part the routine care at the ANC.
Conclusion: Perinatal women attending antenatal services have inadequate knowledge about Hypertensive Disorders in Pregnancy (HDP). Despite this, most respondents demonstrated a favourable understanding of the management of HDP as well as the behaviours and practices that could minimize the development of HDP. However, there could be serious repercussions if HDP is not detected on time or is poorly managed. Midwives and other stakeholders must prioritize and intensify client teaching and education and encourage pregnant women to report to the hospital for identification and prompt treatment to reduce the negative outcomes of HDP. Additionally, mental health services should be incorporated into routine antenatal care services to address the many psychological challenges that may be confronting perinatal women as this may impact birth and treatment outcomes in diverse ways.
Keywords
Hypertensive disorders in pregnancy; Maternal mental health services
Introduction
Hypertensive Disorders in Pregnancy (HDP) mostly occur after 20 weeks of gestation in women with previously normal blood pressure. HDP can be grouped into three categories as gestational hypertension, pre-eclampsia, and eclampsia. Hypertension is defined by a systolic blood pressure of ≥ 140 mmHg and diastolic blood pressure ≥ 90 mmHg or both. Both systolic and diastolic blood pressure spikes are important in the identification of HDP.
Gestational hypertension is characterized by an abnormal rise in blood pressure that usually develops after 20th week of pregnancy. In addition to hypertension, symptoms of preeclampsia include proteinuria and oedema. If the condition progresses to eclampsia, life threatening convulsions and coma can occur. PIH can also result in preterm labour and low birth-weight infants. Hypertensive disorders represent the most common medical complications of pregnancy with a reported incidence of 5%-10%. Globally, pre- eclampsia is the leading cause of maternal and neonatal mortality and morbidity, predominantly in developing countries. The disorder is usually diagnosed in late pregnancy by the presence of high blood pressure with proteinuria and oedema. The World Health Organization estimates that at least one woman dies every seven minutes from complications of pregnancy induced hypertension disorders. Pregnancy complicated with hypertensive disorder is related with increased risk of adverse foetal, neonatal, and maternal outcome.
Although pregnancy-induced hypertension occurs in less than 10% of pregnancies, it is a major risk factor for maternal as well as perinatal morbidity and mortality. Earlier studies report that the incidence of pregnancy induced hypertension is higher in developing countries in comparison to developed countries which complicate about 10% of pregnancy. Studies conducted on HDP indicate that pre-eclampsia and eclampsia as the second leading causes of direct maternal death accounting for 10%-15% of maternal mortality. Moreover, pre-eclampsia has also been noted as responsible for various morbidities associated with pregnancy such as seizure (leading to eclampsia), intracranial haemorrhage, pulmonary oedema, haematological abnormalities (coagulation defect) and heart, renal, liver failure. This notwithstanding, the foetus is also not spared from the hypertensive disorders of pregnancy, facing complications including still birth, abruption placenta, intrauterine growth retardation and premature delivery.
It has also been observed that severe hypertension increases the mother's risk of cardiac failure, heart attack, renal failure, and cerebral vascular accidents. In addition, the foetus is at increased risk from complications like poor placental transfer of oxygen, growth restriction, preterm birth, placental abruption, stillbirth, and neonatal death.
Hypertensive Disorders in Pregnancy (HDP) complicates many pregnancies, especially in the developing world. The cause of this condition is not clear. Several studies have therefore sought to evaluate the risk factors in different parts of the world. Some risk factors have been commonly reported in the developed world while others are common to the developing countries. Since the cause of HDP is unclear, primary prevention largely depends on the identification of its risk factors. Some of the identified risk factors include; Null parity, multiple pregnancies, history of chronic hypertension, gestational diabetes, foetal malformation, obesity, extreme maternal age (less than 20 years or over 40 years), history of PIH in previous pregnancies and chronic diseases like renal disease, diabetes mellitus, cardiac disease, unrecognized chronic hypertension, positive family history of PIH which shows genetic susceptibility, psychological stress, alcohol use, rheumatic arthritis, extreme underweight and overweight, asthma and low level of socioeconomic status.
A two-stage model which was developed to explain the mechanisms of HDP revealed that abnormal implantation reduced placental perfusion and subsequent vascular remodelling interacts with maternal constituents (genetic, behavioural, or environmental) leading to the maternal syndrome. Several medications are available for pregnant women with high blood pressure due to preeclampsia. These include Methyldopa a central acting-alpha adrenergic which has been studied extensively and is recommended by many experts as the first-line oral antihypertensive medication in pregnancy. It is given orally, and it comes in 250 mg per dose of which a maximum dose of 1 g is given three times daily for 24 hrs and, upon administering the drug, the foetal heart must be checked at least 4 hourly and the patient placed on fetal kick count. Methyldopa can be given intravenously in severe cases. Labetalol is another first-line oral antihypertensive medication that blocks blood vessel receptors; its route of administration is orally and intravenously. Nifedipine is a calcium channel blocker. It works by relaxing blood vessels and reducing the heart rate. It’s given orally in 20 mg-60 mg depending on the severity of the condition. Hydralazine is another drug that can be given orally or intravenously to control hypertension in pregnancy. This drug may be used as an injection in very severe cases of high blood pressure [1].
In the Western region of Ghana, high prevalence of HDP is recorded each year. This poses serious consequences to the expectant mothers and their unborn children as well as the health system in the region. Details of the HDP occurrences in four hospitals in the region from 2019 to 2022 are shown in Table 1 below.
| Year under review | Apinto government | Tarkwa municipal hospital | Essikado hospital | Kwesimintim hospital |
|---|---|---|---|---|
| 2019 | 50 | 48 | 25 | 19 |
| 2020 | 59 | 93 | 32 | 31 |
| 2021 | 101 | 107 | 61 | 38 |
| 2022 | 142 | 148 | 32 | 28 |
Table 1: Occurrences of HDP in four hospitals of the Western region.
District health information management system
The Table 1, above indicates that the region, specifically the Tarkwa Nsueam municipality has been recording a progressive increase in hypertensive cases among perinatal women and despite the detrimental effects of HDP on maternal and foetal health, not many studies have been conducted in the region and the country at large. Nonetheless, such studies could help to reduce the incidence of HDP thereby minimizing the associated consequences. In furtherance, the experience of HDP may impact the mental health of perinatal women in diverse ways, ranging from mild anxiety and depression to very severe forms of mental illnesses. However, the incorporation of maternal mental health services in the region and the country at large is lacking and needs to be addressed appropriately [2].
Justification of the study
The every woman to have a pleasant experience during the perinatal period without life-threatening conditions such as Hypertensive Disorders in Pregnancy (HDP) however, this is not always achieved due to the physiological changes that occur during pregnancy and certain risk factors such as family history, obesity, and placental abnormality that predispose one to this condition. Even though HDP is the leading cause of maternal morbidity and mortality during pregnancy globally about the current magnitude of HDP and its associated factors among women attending delivery service in Ghana. In Ghana, it is estimated that about 7.0% of all pregnancies are complicated by HDP, specifically preeclampsia. In the Tarkwa Municipality in the Western region of Ghana, there is no study on HDP although it is a major public health concern as shown in Table 1. It is against this backdrop that this study was conducted to explore the knowledge, attitudes, and practices of pregnant women on HDP and how it impacts maternal mental health with the hope of improving perinatal care and service delivery as well as maternal mental health services (Table 1) [3-6].
Aim
The purpose of this study was to explore the knowledge, attitudes, and practices of perinatal women regarding hypertensive disorders that occur during pregnancy and its implication for the implementation of maternal mental health.
Significance of the study/Implications for practice
This study is relevant to the health workers, pregnant women (service users) and the community since there have been many reported cases of HDP causing perinatal and maternal mortality. The findings from the study would help to clear any misconceptions associated with HDP and to support perinatal women to understand this condition. Thus, helping to minimize the fatalities associated with HDP during the perinatal period. It will also provide insight for policymakers to understand the significance of incorporating maternal mental health services into routine antenatal/perinatal care services. Additionally, it will improve collaboration between the midwives and other stakeholders to implement recommendations that will benefit both service users and service providers. In furtherance, the findings of the study would also provide baseline data for other future studies on HDP [7-10].
Literature Review
Prior studies on Hypertensive Disorders in Pregnancy (HDP) suggest that it poses the greatest impact on maternal mortality and complicates almost a tenth of all pregnancies globally. Additionally, HDP is reported to be the second leading cause of direct maternal death and directly accounts for over 70,000 cases of maternal mortality globally. In furtherance, preliminary studies indicate that perinatal women display poor knowledge and misperceptions about PIH despite its significance for prompt identification and management challenges. However, preliminary reports suggest that despite the challenges, a substantial number of deaths related to pregnancy-induced hypertension could be averted by evidence- based, effective, and timely interventions by increasing women’s knowledge and changing attitudes towards the condition [11].
Hypertensive Disorders in Pregnancy (HDP): Epidemiology
Hypertension is the leading contributor to the global burden of disease, with about 1 billion adults affected worldwide and 9 million associated deaths annually. Hypertensive Disorders in Pregnancy (HDP) are also a major threat to global health. They complicate 5.2%-8.2% of pregnancies globally and are associated with an increased risk of adverse foetal, neonatal, and maternal outcomes including premature delivery, foetal growth restriction, intra-uterine death, renal or hepatic failure, haemorrhage, and stroke. Likewise, some reports have observed that women with HDP have an increased lifetime risk of cardiovascular disease [12].
Although there is a lack of consistency in its definition, HDP refers to a spectrum of conditions of vascular origin and systemic manifestations caused by a mixture of genetic and acquired factors, which occur during pregnancy. Pressure Education Program Working Group on High Blood Pressure in Pregnancy classified HDP into four entities: chronic hypertension, preeclampsia- eclampsia, preeclampsia superimposed on chronic hypertension, and gestational hypertension, with the American College of Obstetricians and Gynaecologists (2018) suggesting that this widely used classification considers the time of appearance of the condition in relation to pregnancy. Whiles chronic hypertension occurs in women who have high blood pressure (over 140/90) before pregnancy or in early in pregnancy (before 20 weeks) and continue to experience its manifestations after delivery, gestational hypertension specifically refers to high blood pressure that develops after the 20th week in pregnancy and goes away after delivery or childbirth. Similarly, both chronic hypertension and gestational hypertension can lead to pre-eclampsia and eclampsia after the 20th week of pregnancy. Symptoms include high blood pressure and protein in the urine. This can lead to serious complications for both mom and baby if not treated quickly [13].
Pregnancy Induced Hypertension (PIH) is defined as BP ≥ 140/90 mmHg taken after a period of rest on two occasions or ≥160/110 mmHg on one occasion in a previously normotensive woman. Pregnancy-induced hypertension affects 5%-7% of all pregnancies. It is broadly defined by hypertension and proteinuria, and this includes pre-eclampsia and eclampsia with the presence of convulsions not attributable to other neurologic diseases [14].
Globally, 10% of all pregnancies are complicated by hypertension, with pre-eclampsia and eclampsia being the major causes of maternal and prenatal morbidity and mortality. It is also estimated that Pregnancy Induced Hypertension (PIH), one of the hypertensive disorders of pregnancy, affects about 5%-8% of all pregnant women worldwide. Studies conducted within the sub-African region report the prevalence of PIH to be around 33% of all pregnancies, whiles in Ghana it is reported to be between 45% to 50%.
Knowledge of pregnant women on hypertensive disorders in pregnancy and its related complications
Preliminary studies have shown that women younger than 20 years as well as those older than 40 years are mostly at risk of HDP. The studies further identify women with first pregnancy and those with pre-existing hypertension to be highly vulnerable to the development of HDP [15-18].
However, health education during antenatal care attendance may play an important role in preventing the disease from aggravating. The World Health Organization report, 2011 shows that high blood pressure levels are more effectively controlled through enhancing the pregnant mothers’ self-awareness and knowledge. Nonetheless, most perinatal women have inadequate knowledge about HDP which hinders their ability to seek prompt medical attention. Studies across the sub-African region have demonstrated a deficit in knowledge among pregnant women on HDP. For instance, findings from a qualitative study in women in South Africa showed that pregnant women with Pregnancy Induced Hypertension had inadequate knowledge on signs and symptoms, management, and the prevention of complications as well as how it impacts the Embryonic fetus. Similarly, another study revealed a deficit in knowledge among pregnant Moroccan women residing in Morocco and The Netherlands on HDP and further reports that more than 50% of the women had no knowledge at all even though they acknowledged that HDP and its complications were dangerous. Since HDP and its associated complications poses a serious threat to pregnant women and their unborn babies, it is prudent for pregnant women to be sensitized and encouraged to regularly attend antenatal clinics for early identification and prompt treatment of the condition [19-22].
Attitudes and practices of pregnant women towards hypertensive disorders in pregnancy
Reports from several studies conducted globally suggest that there is a significant gap among pregnant women related to knowledge, attitude, and perception towards pregnancy-induced hypertension which directly or indirectly influence health seeking-behaviours leading to increased maternal mortality and morbidity. These studies further identify lack of knowledge to be the predisposing factor to practice risky behaviours for pregnancy-induced hypertension as well as other hypertensive disorders in pregnancy whiles poor understanding of the disease leads to anxiety and becomes a source of worry to the family as well. Despite the above, ample evidence exist that suggest a positive correlation between higher educational status and attitude formation towards PIH among pregnant women. For instance, some reports indicate that pregnant women with basic education usually manifest positive attitude, evidenced by their punctuality and regularity to antenatal care clinics and promptly seeking medical attention for any perceived manifestation of PIH. Several other factors such as diet, smoking, and the consumption of alcohol as well as stress during pregnancy have been identified as predisposing factors to PIH. Explored the knowledge and attitudes of pregnant women towards the management of pregnancy induced hypertension in Nigeria and narrates that a substantial number of participants (about 80%) believed that PIH is preventable and would seek medical attention at the hospital should they experience and signs of PIH whiles about 20% of the participants were of the believe that traditional medicine is more effective and therefore they would prefer the later to the former [23].
Similarly, Zuo et al (2016) have highlighted that stress management is essential for the treatment of HDP and further adds that pregnancy in its natural sense could be a significant stressor. Nonetheless, there are no established protocols at antenatal clinics to counsel pregnant women on how to properly manage stress during pregnancy.
Consequences of hypertensive disorders in pregnancy on birth outcomes
Hypertensive Disorders of Pregnancy (HDP) are multisystem diseases, which include chronic hypertension (pre-existing), gestational hypertension, preeclampsia, eclampsia, and superimposed preeclampsia on chronic hypertension. Hypertensive Disorders of Pregnancy (HDP) increase adverse perinatal outcomes in women with the disorder. Whiles 16% of the estimated 2.6 million still births are attributable to HDP globally, 10% of early neonatal deaths are accounted for by the condition. Previous studies reveal that HDP complicates about 6% of all pregnancies and further adds that women with hypertensive disorder of pregnancy of any form were at higher risk of adverse perinatal outcomes compared to their normotensive counterparts. Reports that HDP is associated with disturbed vascular manifestations, oxidative stress, and endothelial damage. This affects placental function resulting in minor perfusion and nutrient supplementation to the foetus that enhances adverse perinatal outcomes [24].
One study found that 1 in 4 (about 37%) of all pregnancies complicated by hypertensive disorders end up in perinatal death and new-born with low birth weight. Consistent with this is another report that suggests that Sub-Saharan (SSA) Africa accounted for the highest Maternal Mortality Ratio (MMR) in Africa, with 546 deaths/100,000 live births in 2015 compared to any other region in the world. The report further states that MMR for SSA represented 65% of all maternal deaths in the developing world. However, in Ghana, there was a steady reduction in the MMR and Infant Mortality Ratio (IMR) from 740 to 319/100,000 live births and 80 to 41 infant deaths/ 1000 live births, respectively, between 1990 and 2015. In furtherance, recent reports on Obstetrical intervention rates and maternal and neonatal outcomes of women with gestational hypertension revealed that, women with PIH had obstetrical intervention rates much higher than normotensive ones. The obstetrical interventions here were the induction and Caesarean delivery rates, with an increased rate of caesarean section among severe preeclamptic women.
Impact of hypertensive disorders in pregnancy on maternal mental health
Existing evidence regarding the relationship between Hypertensive Disorders of Pregnancy (HDP) and the risk of maternal mental illness is inconclusive. Preliminary studies have sought to investigate whether HDP are associated with depressive and anxiety symptoms during pregnancy and reports indicate that mothers with pre-eclampsia had a 53% increased risk of antenatal depressive symptoms compared with those without pre-eclampsia. It further adds that having pre-eclampsia and being a nulliparous woman resulted in the highest risk of antenatal depressive symptoms. It is imperative that perinatal women attending antenatal services be routinely screened for anxiety and depressive symptoms and provided with interventions when indicated [25].
Methodology
A cross-sectional study approach was adopted in this study which seeks to gather information at a single point in time. This approach best suited the subject matter as it allowed the researchers to describe various characteristics among participants as well as gathering preliminary information to support further studies and future directions regarding the knowledge, attitudes, and practices of perinatal women towards Hypertensive Disorders in Pregnancy (HDP).
Study design
A self-structured questionnaire formulated by the researchers was used as a guide to collect data from the participants at a single point in time, with focus on three main thematic areas that include knowledge of participants on hypertensive disorders in pregnancy, attitudes, and practices of perinatal women towards hypertensive disorders in pregnancy as well as knowledge about the consequences of hypertensive disorders in pregnancy on maternal mental health [26].
Study setting
The study was conducted at the antenatal clinic of the Apinto Government Hospital (AGH) in Tarkwa. The AGH serves as the second referral hospital within and outside the Tarkwa Nsuaem Municipality and offers a range of services such as OPD Services, In-Patient Services, Antenatal Care (ANC) and Postnatal Services, Medical and Surgical services among other specialty areas.
Study population/ participants
The researchers recruited pregnant women who were attending ANC services at the Apinto Hospital and voluntarily opted to participate in the study. A total of 267 pregnant women volunteered to participate in the study.
Sample and sampling procedure
Convenience sampling technique was employed to select participants for the study. This allowed participants to conveniently and voluntarily avail themselves to participate in the study after the purpose of the study has been explained to them and all questions or concerns from them have been duly addressed. The Apinto Hospital records on average 800 ANC attendance monthly. Based on this, Yamane’s formula for sample size calculation was used to obtain the sample for the study. This was to ensure that the sample size is representative and statistically significant of the general population. The calculation is given below:
Where, n=the sample size, N= Population size (800 for monthly attendance), e=Acceptable sampling error (0.05)
n= 800/ 1+ 800 (0.05)2 n= 800/ 1+ 800 (0.0025) n= 800/1+2 n= 800/ 3 n= 267
Therefore, using he Yamane’s formula for sample calculation, 267 pregnant women who met the inclusion criteria were randomly recruited over a period of one month for the study.
Data collection
A face-to-face interview was conducted based on a structured questionnaire by the researchers aimed to gather information regarding the participants’ knowledge on hypertensive disorders in pregnancy, attitudes, and practices towards hypertensive disorders in pregnancy as well as their knowledge on the consequences associated with hypertensive disorders in pregnancy and birth outcomes. All the information regarding the study was explained to the participants. Those who had concerns were provided with better and further explanations to the best of their understanding. Consent was then sought from those who willingly volunteered to participate in the study. The participants who could read and write were guided to fill in the questionnaires themselves. However, for the participants who could not read nor write, the researcher translated the questions to them in their local dialect and filled out the questionnaires on their behalf based on their responses. The answered questionnaires were then collected by the researchers [27-29].
Inclusion and exclusion criteria
All pregnant women from Gravida 2 Para 1 and above as well as those who had survived hypertensive disorders such as PIH in their previous pregnancies and are presently attending ANC with their current pregnancies were included in the study whiles first time perinatal women without a history of hypertension were excluded [28].
Data analysis
The data collected were analysed with Microsoft Excel and SPSS (Version 24) software. Basic descriptive quantitative analysis was used based on frequency tables, pie chart and graphical illustration to interpret the data.
Instrument validity
The questionnaires for the study were pretested on 20 pregnant women at the ANC of the Tarkwa Apinto Municipal hospital. This was done to correct any inconsistencies in the questions. After pre-testing, the questionnaires were given to three professionals in the field of biostatistics for their perusal, approval, and validation. The questionnaire was deemed standard and appropriate for the purpose of this study.
Ethical considerations
Ethical approval was sought from the Apinto government hospital. An informed consent was obtained from the study participant.
Confidentiality: The respondents were assured of protecting any personal information that they may provide in accordance with data protection regulation policy of the hospital. The consent form was anonymously filled out without respondents’ names.
Autonomy: Autonomy of respondents was maintained. They were made to understand the purpose of the study and their right to withdraw from the study at any point.
Results
Demographic and clinical characteristics
A total of 267 pregnant women voluntarily participated in the study. Tables 2-5 describe the demographic and clinical characteristics of the study participants. A substantial number of the study participant were within the age bracket of 18-30, representing 64.8% whiles 31.8% were aged between 31 years-40 years. However, less than 5% of the study subjects were above 40 years [29-31]. Similarly, majority of the 267 participants were married (79.4%) whiles the remaining 20.6% were single which they attributed to the fact that their partners have refused to accept responsibility of the pregnancy. Additionally, less than 20% of the study participants had tertiary education (n=44; 16.5%) whiles a greater proportion of them 223 (83.5%) (Tables 2-5).
| Variables | ||
|---|---|---|
| Age | Frequency (n=267) | Percentage (%) |
| 18-30 | 173 | 64.8 |
| 31-40 | 85 | 31.8 |
| Above 40 | 9 | 3.4 |
Table 2: Demographic and clinical characteristics.
| Variables | Frequency (n=267) | Percentage (%) |
|---|---|---|
| Single | 55 | 20.6 |
| Married | 212 | 79.4 |
Table 3: Demographic and clinical characteristics-Marital status.
| Variables | Frequency (n=267) | Percentage (%) |
|---|---|---|
| Basic education | 223 | 83.5 |
| Tertiary education | 44 | 16.5 |
| Occupation | ||
| Formal sector | 89 | 33.3 |
| Informal sector | 152 | 56.9 |
| Unemployed | 26 | 9.8 |
Table 4: Demographic and clinical characteristics-Level of education.
| Variables | Frequency (n=267) | Percentage (%) |
|---|---|---|
| Gravidity | ||
| Primigravida | 63 | 24 |
| Multigravida | 204 | 76 |
| Gestation | ||
| 20–28 weeks | 95 | 36.5 |
| 29–32 weeks | 106 | 39.6 |
| 33–40 weeks | 66 | 23.9 |
| Religion | ||
| Islam | 62 | 23.2 |
| Christianity | 198 | 74.2 |
| None | 7 | 2.6 |
Table 5: Demographic and clinical characteristics-Pregnancy history.
In furtherance, 152 of the participants, representing 56.9% were employed in the informal sector with majority of them engaged in petty trading. About 89 of the participants (33.3%) were engaged in the formal sector such as banking, health, and education. The remaining 9.8% (26 participants) were unemployed. With regards to gravidity and pregnancy, 204 (76%) of the participants were multigravida whiles 63 (24%) were primigravida. Similarly, about 106 (39.6%) of the participants were within their second trimester (29 weeks-32 weeks) whiles 95 (36.5%) were in their first trimester (20 weeks-28 weeks) with the remaining 66 (23.9%) in their third and final trimester period of gestation (33 weeks-40 weeks). Data was also collected on the religious affiliation of the participants where 198 (74.2%) aligned with the Christian faith and 62 (23.2%) were Muslims. However, less than 3% of the study participants had no religious affiliation [32].
Knowledge of respondents on hypertensive disorders in pregnancy
This study sought to assess the knowledge of respondents on Hypertensive Disorders in Pregnancy (HDP) as one of its study objectives. The participants were asked to respond to a set of questions relating to the causes and risk factors of the subject matter as well as identifying symptoms of HDP as presented in Tables 6 and 7 respectively. To achieve this goal, the participants were asked a set of questions on some of the causes, risk factors and symptoms of HDP. A correct answer attracted score of 1 while a wrong answer or “Don’t know” response to a particular question was scored zero (0). The participants, who scored above 50% of the total mark, were regarded as having adequate knowledge of Hypertensive Disorders in Pregnancy whiles a score below 50% of total mark was regarded as inadequate knowledge of HDP. Presented in Table 7 describes the responses of the study participants (Tables 6 and 7).
| Statement | Yes (n=%) | No.(n=%) | Don’t Know (n=%) |
|---|---|---|---|
| Awareness of pregnancy Hypertensive Disorders in Pregnancy (HDP) | 124 (46.4) |
143 (53.6) | 0 (0.0) |
| Stress may cause HDP | 267 (100) |
0 (0.0) |
0 (0.0) |
| High salted diet and high cholesterol contribute to HDP | 172 (64.4) |
95 (35.6) |
0 (0.0) |
| smoking can cause HDP | 108 (40.5) |
159 (59.6) |
0 (0.0) |
| Obesity, cardiac disease, and diabetes mellitus are associated with HDP | 97 (36.3) |
119 (44.6) | 51 (19.1) |
Table 6: Knowledge of respondents on hypertensive disorders in pregnancy.
| Statement | Yes | No | Don’t Know n (%) |
|---|---|---|---|
| (n=%) | (n=%) | ||
| Blood pressure control helps manage HDP | 197 | 0 | 70 |
| -73.8 | 0 | -26.2 | |
| Signs of HDP | |||
| Swelling of face, fingers, and feet | 128 | 42 | 97 |
| -47.9 | -15.8 | -36.3 | |
| Nausea and vomiting | 136 | 0 | 131 |
| -50.9 | 0 | -49.1 | |
| Frontal headache | 195 | 23 | 49 |
| -73 | -8.6 | -18.4 | |
| High blood pressure | 200 | 18 | 49 |
| -74.9 | -6.7 | -18.4 | |
| Generalized body weakness | 177 | 38 | 52 |
| -66.3 | -14.2 | -19.5 | |
| Indicate whether the following are risk factors of HDP | |||
| Gestational diabetes | 0 | 28 | 239 |
| 0 | -10.5 | -89.5 | |
| Foetal malformation | 0 | 0 | 267 |
| 0 | 0 | -100 | |
| Nulliparity and Grand multiparous | 23 | 62 | 182 |
| -8.6 | -23.2 | -68.2 | |
| Extreme maternal age | 91 | 0 | 176 |
| -34.1 | 0 | -65.9 | |
Table 7: Knowledge of respondents on hypertensive disorders in pregnancy.
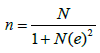
It was observed that majority of the study participants (52.2%) had a knowledge deficit of Hypertensive disorders in pregnancy whiles 47.8% were aware about the causes, risk factors and clinical manifestations of HDP. Figure 1 is a graphical presentation of the knowledge about the awareness of respondents on HDP (Figure 1).
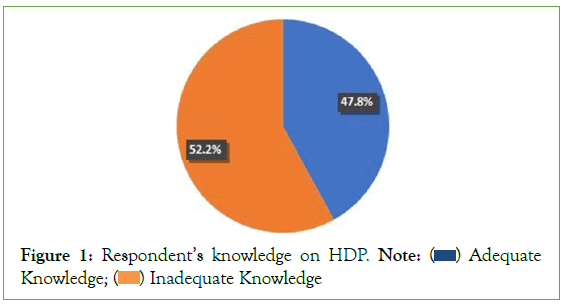
Figure 1: Respondent’s knowledge on HDP. Note:  Adequate Knowledge;
Adequate Knowledge;  Inadequate Knowledge
Inadequate Knowledge
Most importantly, almost all the study participants had no knowledge about such risk factors as gestational diabetes, foetal malformation as well as nulliparity and grand multiparity to be contributing to the development of hypertensive disorders in pregnancy [33-35].
Attitude and practice of pregnant women in dealing with hypertensive disorders in pregnancy
The antenatal clinic records of the respondents were assessed in addition to interviews to determine those with a history of HDP. It observed that 151 (56.6%) of the respondents had previously been diagnosed with HDP whiles 116 (43.4%) never experienced the condition during their pregnancy as presented in Table 8 below.
| Respondents with history of HDP | Frequency | Percentage (%) |
|---|---|---|
| Yes | 151 | 56.6 |
| No | 116 | 43.4 |
| Total | 292 | 100 |
Table 8: Proportion of respondents with history of HDP.
The respondents with history of some forms of HDP were also assessed on treatment compliance as illustrated in Figure 2 and Table 9, respectively. Interestingly, it was noted that majority of the respondents adhered strictly with the treatment regimen. The respondents were assessed on Regular medication intake, strict foetal kick count, Bed rest, and other measures such as regular exercising and adequate nutritional intake. Again, it was observed that 203 (76.0%) of the participants adhered strictly to their treatment regimen whiles 13 (4.9%) reported the regular counting of foetal kicks. Only 45 (16.9%) of the respondents reported getting enough bed rest whiles an insignificant number of respondents, about 6 (2.2%) engaged in regular exercises (Figure 2) (Table 9).
| Variable | Frequency | Percentage (%) |
|---|---|---|
| Regular intake of medication | 203 | 76 |
| Strict fetal kick count | 13 | 4.9 |
| Bed rest | 45 | 16.9 |
| Other | 6 | 2.2 |
Table 9: Participants’ adherence to treatment regimen.
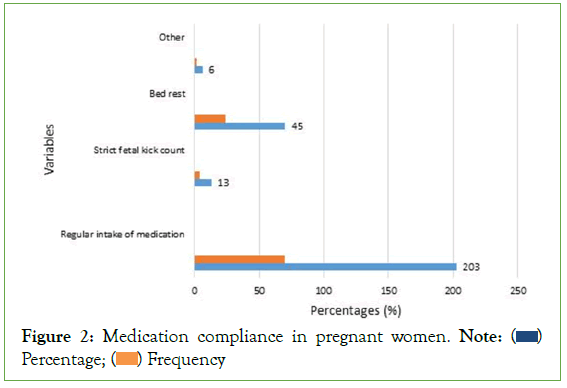
Figure 2: Medication compliance in pregnant women. Note:  Percentage;
Percentage;  Frequency
Frequency
Moreover, we sort to understand the behaviour of participants who were diagnosed with some forms of HDP for the first time using the variables shown in Table 10 below.
| Variable | Frequency | Percentage (%) |
|---|---|---|
| Deny admission | 97 | 36.1 |
| Refusal to take medication | 11 | 4.1 |
| Comply to management regime | 130 | 48.9 |
| Deny laboratory testing | 12 | 4.5 |
| Other | 17 | 6.4 |
Table 10: Behaviour after being diagnosed of HDP.
It can be inferred from the table above that whiles a significant number of participants (36.1%) denied admission following the diagnosis of HDP, a substantial number (48.9%) adhered to their treatment plan after being diagnosed with HDP for the first time.
The respondents were further assessed on certain practices which are recommended to prevent the development of HDP as indicated in Figure 3 above. Additionally, study participants were assessed on such risky behaviours that are necessary to avoid when diagnosed with HDP to prevent further complications as shown in (Figure 3) (Table 11).
| Question | Yes (n=%) |
No (n =%) |
|---|---|---|
| Avoiding fatty and salty foods when diagnosed with | 243 | 24 |
| HDP | -91 | -9 |
| Avoiding alcoholism and smoking during pregnancy | 267 | 0 |
| -100 | 0 | |
| Exercising is essential to reducing HDP | 180 | 87 |
| -67.4 | -32.6 |
Table 11: Practices of respondents with regards preventing HDP.
Figure 3: Behaviour of Respondents after Being Diagnosed with HDP for the first time. Note:  Frequency;
Frequency;  Percentage
Percentage
It was observed that all the participants were very much aware of the practices that could help prevent the development of HDP as demonstrated in Figure 4 above. In furtherance Table 12, illustrates the level of knowledge of respondents regarding the complications that may occur because of developing HDP. It can be inferred that majority of the study participants had insufficient knowledge about the complications of HDP. However, a significant number of the respondents 234 (87.6%) identified seizures as the most common complication (Figure 4) (Table 12).
| Complication | Yes (n=%) |
No (n=%) |
|---|---|---|
| Seizures in the mother | 33 | 234 |
| -12.4 | -87.6 | |
| Stroke | 0 | 267 |
| 0 | -100 | |
| Temporary kidney failure | 0 | 267 |
| 0 | -100 | |
| Liver problems | 0 | 267 |
| 0 | -100 | |
| Placental abruptio causing distress to the baby | 57 | 210 |
| -21.3 | -78.7 | |
| Premature (early) delivery of the baby | 73 | 194 |
| -27.3 | -72.7 |
Table 12: Knowledge of complications among HDP respondents.
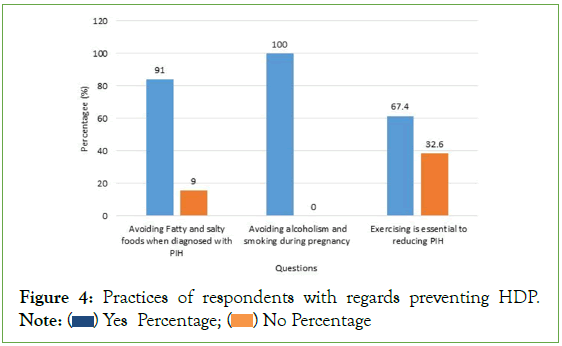
Figure 4: Practices of respondents with regards preventing HDP. Note:  Yes Percentage;
Yes Percentage;  No Percentage
No Percentage
Maternal mental health services
The study also explored the perinatal women experience with minor mental health issues and how they sought help from service providers. Some aspects of mental health such as the availability of Maternal Mental Health Services (MMHS), family support systems as well as recognizing and reporting any psychological distress was examined (See Table 13 below).
| Maternal mental health services | YES (n=%) |
NO (n=%) |
|---|---|---|
| Availability of maternal mental health services | 4.6 | 95.4 |
| Family support systems | 22 | 78 |
| Recognising Psychological Distress and Reporting | 100 | 0 |
Table 13: Maternal mental health services.
From Table 13 above, a substantial number of respondents (95.4%) indicated that they had no access to maternal mental health services whiles a little above 4% sought help from mental health professionals, mainly psychiatric nurses for advice [36]. Similarly, only 22% of the respondents received some form of support from relatives such as constantly reassuring and encouraging them to seek medical advice for any psychological distress that they may be experiencing. However, a greater number of the respondents (78%) reported absence of any form of support from their relatives. All the respondents were able to recognise the presence of psychological difficulties mostly due to the pregnancy.
Discussion
This section provides insight into the data gathered as well as making sense of the study results and further makes suggestions for improved perinatal care as part of its recommendations in relation to the subject matter (Hypertensive Disorders in Pregnancy, HDP). The study was intended to assess the knowledge, attitudes, and practices of perinatal mothers on hypertensive disorders in pregnancy accessing services at the Apinto Government Hospital in the Western Region of Ghana. A cross-sectional study approach was adopted in this study to solicit information from study participants as it allowed the researchers to describe various characteristics among participants whiles gathering preliminary information to support future directions regarding the subject matter. A self- structured questionnaire was used as a guide to collect data from the study participants at a single point in time, with focus on three thematic areas that include the knowledge of participants on hypertensive disorders in pregnancy, attitudes, and practices of perinatal mothers towards hypertensive disorders in pregnancy as well as their knowledge on the consequences of HDP in pregnancy.
A total of 267 perinatal mothers voluntarily participated in the study. All pregnant women from Gravida 2 Para 1 and above as well as those who had survived hypertensive disorders in their previous pregnancies and are presently accessing antenatal services were included in the study whiles first time perinatal women without a history of hypertension were excluded. The data collected were analysed with Microsoft Excel and SPSS (Version 24) software. Basic descriptive quantitative analysis was used based on frequency tables, pie chart and graphical illustration to interpret the data.
Demographic and clinical characteristics of participants
Perinatal mothers in the 18-30 age bracket constituted most of the study population (64.8%) whiles a little above 3% of the participants were aged above 40 years. A substantial number of study participants, about 84% had attained basic education and could read and write whiles 16% had tertiary education. This made data collection quite easier and faster since participants understood the information in the study questionnaire. Similarly, about 241 (approximately 91%) out of the 267 participants were engaged in a variety of income-generating enterprises both in the formal and informal sectors whiles the remaining 9%, although unemployed had financial support from their families. The study participants leveraged on this to access antenatal services as they did not have much financial challenges.
Knowledge of respondents on hypertensive disorders in pregnancy
The study sort to assess the knowledge of participants on HDP However, in almost all the parameters that were assessed in relation to this, it became evidently clear that participants had a knowledge deficit on the subject matter. For instance, about 54% of the study participants were not aware of HDP whiles over 60% had no knowledge about the major causes and risk factors of HDP. This finding is consistent with preliminary studies that identified a knowledge gap among perinatal mothers on hypertensive disorders in pregnancy. However, approximately 74% of study participants were very much informed that adequate control of high blood pressure was an effective way of mitigating the impact of HDP on both mother and fetus. This is also supported by prior studies that confirmed perinatal mothers’ awareness of the importance of adhering to treatment regimen in the management of hypertension in pregnancy. Generally, most of the study participants were unaware of the identified risk factors as contributing to the development of HDP. For instance, over 89% of the respondents had no knowledge of gestational diabetes as a risk factor for developing HDP while more than 68% were unaware that Nulliparity and Grand multiparity could possibly cause HDP. This notwithstanding, the study did not identify trends or patterns among participants regarding risk factors. For example, the study did not identify the number of the respondents aged over 40 years who have gestational diabetes, obesity or any other factor contributing to their diagnosis of HDP [37].
Attitude and practice of pregnant women in dealing with hypertensive disorders in pregnancy
In relation to this, information was solicited from study participants regarding medication compliance, exercises, regular foetal counts as well as other important areas such as adequate nutrition and rest. Interestingly, a substantial number of respondents (76%) complied with their treatment plan as the surest way of minimizing the impact of HDP on themselves and their unborn babies. This view of the participants is again supported by earlier reports on medication adherence among perinatal mothers with HDP. Again, quite a considerable number of respondents (36.1%) demonstrated a lack of interest in adhering to treatment which subsequently led them to deny admission and management after they were diagnosed of HDP for the first time. Similarly, most participants were aware of the many healthy practices that could reduce the risk of developing HDP. For instance, all the study participants knew that reducing or avoiding the consumption of alcohol and smoking cigarette could limit their chances of developing HDP whiles over 90% were aware that limiting fatty and salty foods as well as exercising was of immense benefit. However, just a few could make time to exercise. It is noteworthy to state again that the study did not identify any correlation between higher educational levels and the attitudes and practices of the participants towards HDP even though some reports suggest a strong association between these parameters.
Knowledge of complications and consequences of HDP among respondents
Despite theirinsufficient knowledge about therange of complications that may emanate from HDP, all the study participants identified stroke (cardiovascular accident) as a common effect of HDP whiles about 87.6% of the participants labelled seizures as the most common demonstrable consequence. This finding also resonates with some earlier reports on the subject matter. It is imperative to note that the study did not prioritize identifying respondents with a history of any complications resulting from HDP.
Maternal mental health services
In as much as study participants could recognise and report psychological distress such as anxiety, panic attacks and excessive worry that impacted many facets of their lives during the perinatal period, there were no significant mental health services for perinatal women attending antenatal clinics. Further checks revealed that mental health screening did not form part the routine care at the ANC. The responses also revealed the lack of family support for majority of perinatal women and therefore it is important for service providers to intensify their education and sensitize the public in this regard.
Implications of the study for clinical practice and recommendation
Although the study participants had inadequate knowledge on the subject matter, many of the respondents had a positive attitude toward the management of HDP. This suggests that increasing awareness of HDP and other pregnancy-related problems could significantly lower their incidence and fatality rates. It is thus important to integrate awareness creation and sensitization of the subject matter into routine perinatal care to support expectant mothers who may develop HDP.
Conclusion
This study revealed that perinatal women attending antenatal services have little knowledge about Hypertensive Disorders in Pregnancy (HDP). Despite this, most respondents demonstrated a favourable understanding of the management of HDP as well as the behaviours and practices that could minimize the development of HDP. However, there could be serious repercussions if HDP is not detected on time or is poorly managed. Midwives and other stakeholders must prioritize and intensify client teaching and education and encourage pregnant women to report to the hospital for identification and prompt treatment to reduce the negative outcomes of HDP. Additionally, mental health services should be incorporated into routine antenatal care services to address the many psychological challenges that may be confronting perinatal women as this may impact birth outcomes in diverse ways.
Further studies may be required to understand the patterns or trends of admissions among perinatal mothers who may be experiencing some forms of psychological problems and the individual patient characteristics that impacts treatment and birth outcomes in HDP.
Limitations
The major challenge was the difficulty in accessing participant’s records.
Declarations
Mustapha Karikari declare that the authors of this paper have no competing interests or any other interests that seek to influence the results and discussions addressed in this paper as defined by BMC. Additionally, the results/tables/figures in this manuscript have not been published or submitted elsewhere for consideration. In furtherance, Mustapha Karikari confirms that has read the journal submitting policies and hereby submits this manuscript in accordance with these policies. Again, all the materials in this manuscript are owned by the authors and do not require any permission to be published. Lastly, participant’s engagement was done in accordance with the relevant guidelines and policies.
Ethical approval and consent to participate
Ethical approval was sought from the Apinto government hospital. An informed consent was obtained from the study participants. The participants were informed that the outcome of the study will be published for a wider readership and consent for same was sought from the participants. Mustapha Karikari confirm that the Apinto government hospital has an ethical committee that grant approval for all study activities to be undertaken in their facility and ensures that researchers conduct themselves in accordance with the relevant guidelines and regulations. The respondents were assured of protecting any personal information that they may provide in accordance with data protection regulation policy of the hospital. The consent form was anonymously filled out without respondent’s names.
Consent for publication
The study participants were informed that the outcome of the study will be published for a wider readership and consent to publish same was sought from the participants accordingly. This manuscript does not contain information or images that could lead to identification of study participants. Additionally, no such information or images about participants will be made available in an online open- access publication for readers. In furtherance, Mustapha Karikari wishes to state that the study did not employ any experiment that involved human subjects/ human tissues. Again, participants do not have legal representation, making it difficult to inform same. However, participants voluntarily participated in the study after the purpose of the study has been explained to them to the best of their understanding.
Availability of data and materials
Mustapha Karikari wish to state that the materials used for this study as well as the raw data collected can be made available by the authors upon request and only after all parties have agreed for these to be provided accordingly.
Competing interest
The authors wish to state that there is no conflict of interest related to this research or its content. This study received no funding or specific grant from any funding agency, commercial or non-profit sector. The authors also assert that all procedures contributing to this work comply with the ethical standards and principles of the relevant in the conduct of primary research. Mustapha Karikari therefore confirms that all methods were carried out in accordance with relevant guidelines and regulations. Authors also do not have any financial and non-financial interests regarding the content of this manuscript.
Author's Contribution
MK is the lead researcher. Designed the study and was responsible for data collection, analysis, writeup of manuscript and cleaning of the data.
JBP responsible for reviewing the data and study design, selection of study area and formulation of interview questionnaire.
VA participated in the selection of literature relevant to the study and literature review.
JOA was also involved in the review of study design, interpreting the responses and proof reading of the final manuscript.
EOA was involved in data collection and coding as well as securing ethical approval for the study.
Funding
Not Applicable
Acknowledgement
Not Applicable
References
- Abalos E, Cuesta C, Grosso AL, Chou D, Say L. Global and regional estimates of preeclampsia and eclampsia: A systematic review. Eur J Obstet Gynecol. 2013;170(1):1-7.
- Adu-Bonsaffoh K. Prevalence of hypertensive disorders in pregnancy at Korle-Bu teaching hospital in Ghana. J Gynecol Neonatal Biol. 2017;3(1): 8-13
- Akeju DO, Oladapo OT, Vidler M, Akinmade AA, Sawchuck D, Qureshi R, et al. CLIP Nigeria Feasibility working group. Determinants of health care seeking behaviour during pregnancy in Ogun State, Nigeria. Reproductive health. 2016;13(10):67-74.
- ACOG. American College of Obstetricians and Gynecologists. Hypertension in pregnancy. 2018.
- Asseffa NA, Demissie BW. Perinatal outcomes of hypertensive disorders in pregnancy at a referral hospital, Southern Ethiopia. PloS one. 2019;14(2):240-245.
- Baragou S, Goeh-Akue E, Pio M, Afassinou YM, Atta B. Hypertension and pregnancy in Lome (sub-Saharan Africa): Epidemiology, diagnosis and risk factors. InAnnales de Cardiologie et D'angeiologie 2014; 63(3):145-150.
- Buchbinder A, Sibai BM, Caritis S, MacPherson C, Hauth J, Lindheimer MD, et al. Adverse perinatal outcomes are significantly higher in severe gestational hypertension than in mild preeclampsia. Am J Obstet Gynecol. 2002;186(1):66-71.
- Berhan Y, Berhan A. Perinatal mortality trends in Ethiopia. Ethiopia J Health Sci. 2014;24(1):29-40.
- Abedian Z, Soltani N, Mokhber N, Esmaily H. Depression and anxiety in pregnancy and postpartum in women with mild and severe preeclampsia. Iran J Nurs Res. 2015;20(4):454-455.
- Dadelszen P, Magee L. What matters in preeclampsia are the associated adverse outcomes: the view from Canada? Curr Opin Obstet Gynecol. 2008;20(2):110-115.
- Di Renzo GC, Spano F, Giardina I, Brillo E, Clerici G, Roura LC. Iron deficiency anemia in pregnancy. Women’s Health. 2015;11(6):891-900.
- Esposito G, Ambrosio R, Napolitano F, Di Giuseppe G. Women’s knowledge, attitudes and behavior about maternal risk factors in pregnancy. PloS one. 2015;10(12):0145873.
- Ejike DE, Ambrose B, Moses DA, Karimah MR, Iliya E, Sheu OS, et al. Determination, knowledge and prevalence of pregnancy-induced hypertension eclampsia among women of childbearing age at Same district hospital in Tanzania. Int J Med Med Sci. 2018;10(2):19-26.
- Fadare RI, Akpor OA, Oziegbe OB. Knowledge and attitude of pregnant women towards management of pregnancy-induced hypertension in Southwest Nigeria. J Adv Med Pharm Sci. 2016;11(2):1-2.
- GBD. Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental, and occupational, and metabolic risks or clusters of risks, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;388(53):1659‐1724.
- Gulmezoglu AM, Lawrie TA, Hezelgrave N, Oladapo OT, Souza JP, Gielen M, et al. Interventions to reduce maternal and newborn morbidity and mortality. Reproductive, maternal, newborn, and child health. 2016;2(1):115-136.
- Gofton EN, Capewell V, Natale R, Gratton RJ. Obstetrical intervention rates and maternal and neonatal outcomes of women with gestational hypertension. Am J Obstet Gynecol. 2001;185(4):798-803.
- Jaleta DD, Gebremedhin T, Jebena MG. Perinatal outcomes of women with hypertensive disorders of pregnancy in Jimma Medical Center, southwest Ethiopia: Retrospective cohort study. Plos one. 2021;16(8):256-520.
- Lawn JE, Blencowe H, Pattinson R, Cousens S, Kumar R. Stillbirths: Where? When? Why? How to make the data count. The Lancet. 2011; 377(75):1448-1463.
- Lawn JE, Blencowe H, Waiswa P, Amouzou A, Mathers C, Hogan D. Stillbirths: rates, risk factors and potential for progress towards 2030. Lancet. 2016;387(18):587-603.
- Maputle MS, Lebese RT, Khoza LB. Perceived challenges faced by mothers of pregnant teenagers who are attending a particular school in Mopani District, Limpopo Province, South Africa. Int J Educ Sci. 2015;10(1):142-148.
- Osungbade KO, Ige OK. Public health perspectives of preeclampsia in developing countries: implication for health system strengthening. J pregnancy. 2011; 2011:481-495.
[Crossref]
- Ouasmani F, Engeltjes B, Haddou Rahou B, Belayachi O, Verhoeven C. Knowledge of hypertensive disorders in pregnancy of Moroccan women in Morocco and in the Netherlands: a qualitative interview study. BMC pregnancy and childbirth. 2018;18(1):1-1.
- Hofmeyr GJ, Lawrie TA, Atallah AN, Torloni MR. Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems. Cochrane database of systematic reviews. 2018.
- Program NH. Report of the national high blood pressure education program working group on high blood pressure in pregnancy. Am J Obstet Gynecol. 2000; 183(1):S1-S22.
- Say L, Chou D, Gemmill A, Tuncalp O, Moller AB, Daniels J, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014; 2(6):323-333.
- Sibai BM. Diagnosis and management of gestational hypertension and preeclampsia. Obstetrics & Gynecology. 2003; 102(1):181-192.
- Srinivas SK, Edlow AG, Neff PM, Sammel MD, Andrela CM, Elovitz MA. Rethinking IUGR in preeclampsia: Dependent or independent of maternal hypertension. J Perinatol. 2018; 29:680–684.
- Sutan R, Hassan H, Shamsuddin K. Health information seeking behavior among Hypertensive Disorder In Pregnancy (HDP) high risks antenatal mothers. Women’s Health Gynaecology. 2016;2(1):7-8.
- Townsend R, O Brien P, Khalil A. Current best practice in the management of hypertensive disorders in pregnancy. Integr Blood Press Control. 2016; 9(1):79–94.
- Tooher J, Thornton C, Makris A, Ogle R, Korda A, Hennessy A. All hypertensive disorders of pregnancy increase the risk of future cardiovascular disease. Hypertension. 2017;70(4):798‐803.
- Tranquilli Al, Dekker G, Magee L. The classification, diagnosis and management of the hypertensive disorders of pregnancy: a revised statement from the ISSHP. Pregnancy Hypertension. 2014;4(2):97‐104.
- Umesawa M, Kobashi G. Epidemiology of hypertensive disorders in pregnancy: Prevalence, risk factors, predictors and prognosis. Hypertens Res. 2017;40(3):213‐220.
- Vidler M, Charantimath U, Katageri G, Ramadurg U, Karadiguddi C, Sawchuck D, et al. Community perceptions of pre-eclampsia in rural Karnataka State, India: A qualitative study. Reproductive Health. 2016;13(10):1-7.
[Crossref]
- WHO/RHR. WHO recommendations for Prevention and treatment of preeclampsia and eclampsia Implications and Actions.2013.
- World Health Organization. A global brief on hypertension: silent killer, global public health crisis. World health day 2013. Geneva, Switzerland: world health organization press. 2013.
- Zamorski MA, Green LA. National high blood pressure education program working group report on high blood pressure in pregnancy. Am J Obstet Gynecol. 1990;163(1):1691‐1742.
Citation: Karikari M, Pwavra JBP, Adeleke V, Akunna JO, Antwi EO (2023) Exploring the Knowledge, Attitudes and Practices of Perinatal Women towards Hypertensive Disorders in Pregnancy (HDP) and its Implication for the Implementation of Maternal Mental Health Services (MMHS): A Quantitative Descriptive Study. J Clin Res Bioeth. 14:473.
Copyright: © 2023 Karikari M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

