Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- Google Scholar
- SHERPA ROMEO
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2023) Volume 11, Issue 4
Evidence of Global Warming: A Meta-Analysis of Temperature Management in Aortic Surgery
Florian Huber*Received: 21-Jul-2023, Manuscript No. JVMS-23-22300; Editor assigned: 24-Jul-2023, Pre QC No. JVMS-23-22300 (PQ); Reviewed: 14-Aug-2023, QC No. JVMS-23-22300; Revised: 21-Aug-2023, Manuscript No. JVMS-23-22300 (R); Published: 28-Aug-2023, DOI: 10.35248/2329-6925.23.11.534
Abstract
Objectives: Treatment of aortic pathologies involving the distal ascending aorta, aortic arch, and descending aorta remains a complex and challenging procedure. Appropriate management is important to achieve satisfactory outcome. Surgical management aims to reduce the time of circulatory arrest. The optimal level of hypothermia is still a matter of debate. The present meta-analysis shows the influence of different temperature levels on mortality and morbidity following aortic arch surgery.
Methods: We performed a meta-analysis of published data between January 2000 and March 2020 based on a literature research. 120 studies were included with a total of 32,323 patients divided into three different groups of systemic hypothermia (temperature group 1: ≥ 25°C, temperature group 2: 25-20°C, temperature group 3: ≤ 20°C) were used for statistical analysis.
Results: Early mortality was lowest in temperature group 1 compared to group 2 (OR=1.42; 95% CI, 1.09-1.85; p=0.01) and group 3 (OR=1.74; 95% CI, 1.20–2.52; p=0.003). Perioperative stroke appeared to be less frequently in temperature group 1 versus group 2 (OR=1.48; 95% CI, 1.20-1.82; p=0.0002) and group 3 (OR=1.61; 95% CI, 1.19- 2.18; p=0.002). Similar results are obtained concerning new renal insufficiency (group 1 versus group 2: OR=1.20; 95% CI, 0.91-1.57, p=0.19; group 1 versus 3: OR=0.94; 95% CI, 0.67-1.32, p=0.73) and re-exploration for bleeding (group 1 versus group 2: OR=1.10; 95% CI, 0.80-1.53, p=0.55; group 1 versus group 3: OR=1.92; 95% CI, 1.26-2.94, p=0,0025).
Conclusions: We observed that moderate level of hypothermia during circulatory arrest reduced the incidence of early mortality. Most dreaded neurologic complications occurred less frequently in TG 1. In contrast there was no difference with regards with new onset of renal failure which is commonly accepted as a reliable marker of the quality of visceral organ protection.
Keywords
Hypothermia; Hypothermic circulatory arrest; Aortic dissection; Aortic aneurysm
Introduction
Aortic arch surgery is still a surgical challenge associated with high mortality and morbidity [1,2]. Cerebral and visceral organ protection can be performed using various surgical strategies. Historically, aortic arch surgery has been mainly performed during a period of Deep Hypothermic Circulatory Arrest (DHCA) introduced by Griepp, et al [3]. Deep hypothermic circulatory arrest requires extended time of Cardiopulmonary Bypass (CPB) needed for cooling and rewarming and is associated with serious negative side effects such as clotting disturbances and organ dysfunction [4]. Adjunct techniques of Retrograde Cerebral Perfusion (RCP) and Antegrade Cerebral Perfusion (ACP) at distinct temperature levels have been developed to avoid severe complications of DHCA. Retrograde perfusion via the superior caval vein failed to achieve sufficient brain perfusion. Therefore, it has lost its popularity [5]. Selective antegrade cerebral perfusion offers a more physiologic method and has become the method of choice for cerebral protection during aortic arch surgery in many centers [5-8]. The use of selective antegrade cerebral perfusion makes deep hypothermia nonessential and there is a growing tendency to increase body temperature during circulatory arrest [6-8]. However, controversy still exists regarding the optimal modality and temperature level for cerebral protection.
The aim of the present meta-analysis was to review all published literature to evaluate the influence of different temperature levels during circulatory arrest on mortality and clinical outcome.
Materials and Methods
Search strategy and study selection
We performed a comprehensive literature research using the PubMed database. Keywords such as hypothermia, hypothermic circulatory arrest, aortic dissection, aortic aneurysm, mortality and morbidity in various combinations were used. All articles published in English language between January 2000 and March 2020 based on human subjects was initially considered. Case reports, letters, editorials, and systematic reviews were excluded. A multistage assessment was used to determine if articles are qualified for the analysis. Initially, only the abstracts were screened. Publications reporting data about aortic arch surgery at different levels of hypothermia were selected. A minimum of fifty patients per study group was necessary for study inclusion. A too wide temperature range or incomplete data on hypothermia during circulatory arrest were predefined exclusion criteria. Further exclusion criteria were not reporting data about mortality or neurological events. At a second stage full text versions of the selected articles were reviewed for data extraction. In case of multiple reports, we used the most complete and/or most recent one. All studies were reviewed by 2 independent investigators and disagreements were resolved by the senior author. The meta-analysis was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta- Analyses (PRISMA) statement for reporting systematic reviews and meta-analysis [9]. The study was performed based on published data. More ethical approval was not needed.
Outcomes of interest
The primary outcomes were operative mortality and neurological morbidity. Early mortality was defined as death during the initial hospitalization. Transient Neurological Deficit (TND) was defined as the presence of reversible postoperative motor deficit, confusion, agitation, or transient delirium. Computed Tomograph (CT) findings were required to be normal, with resolution of all symptoms before discharge. Permanent Neurological Deficit (PND) was defined as the presence of new focal (stroke) or global (coma) permanent neurological dysfunction. Secondary outcomes were postoperative renal failure and re-exploration for bleeding. Acute renal failure was defined as a threefold increase in serum creatinine from baseline or a urine output of less than 0.3 ml/kg/h for more than 24 hours.
Statistical analysis
The selected 120 studies consist of 147 study groups. 52 study groups are part of studies where comparisons between temperature groups are conducted. For nominal variables such as mortality measures overall proportions are calculated by dividing the number of cases (e.g. deaths) by the sum of all study participants. Proportions per study group are calculated analogously using only valid observations. For metric variables overall means are computed as weighted study group means using the number of patients per study group as weights. If study group means of metric variables such as durations (of e.g. x-clamp time or circulatory arrest) were not reported imputation was performed using the available information: if quartiles were reported the method of Luo et al. was used otherwise the median was used as estimator for the mean. The corresponding standard errors were only reported in few studies and therefore we report overall means and temperature group means together with standard deviations between studies.
Main and secondary outcome measures between temperature groups are compared by fixed Odds ratios, using only those studies that contain the relevant temperature groups. Weights were estimated using the inverse variance method and 95% confidence intervals are reported. To test for significant differences in main and secondary outcome variables between the temperature groups fixed effects models were used. Forest plots are provided to present estimates and confidence intervals for odds-ratios in study groups. The level of significance was set to 5%.Statistical analysis was conducted using the software package R and the R-packages metafor and metaviz.
Results
Study selection
Figure 1 summarizes the results of the literature search. 1916 studies were identified published within the determined time span of the analysis. After careful review, 120 studies met the study criteria and were selected for analysis. A total of 32 323 patients were included divided into three temperature groups depending on the temperature level of each study group (temperature group 1 ≥ 25°C=12.495 patients, temperature group 2 25°C-20°C=11.655 patients, temperature group 3 ≤ 20°C=8.173 patients).
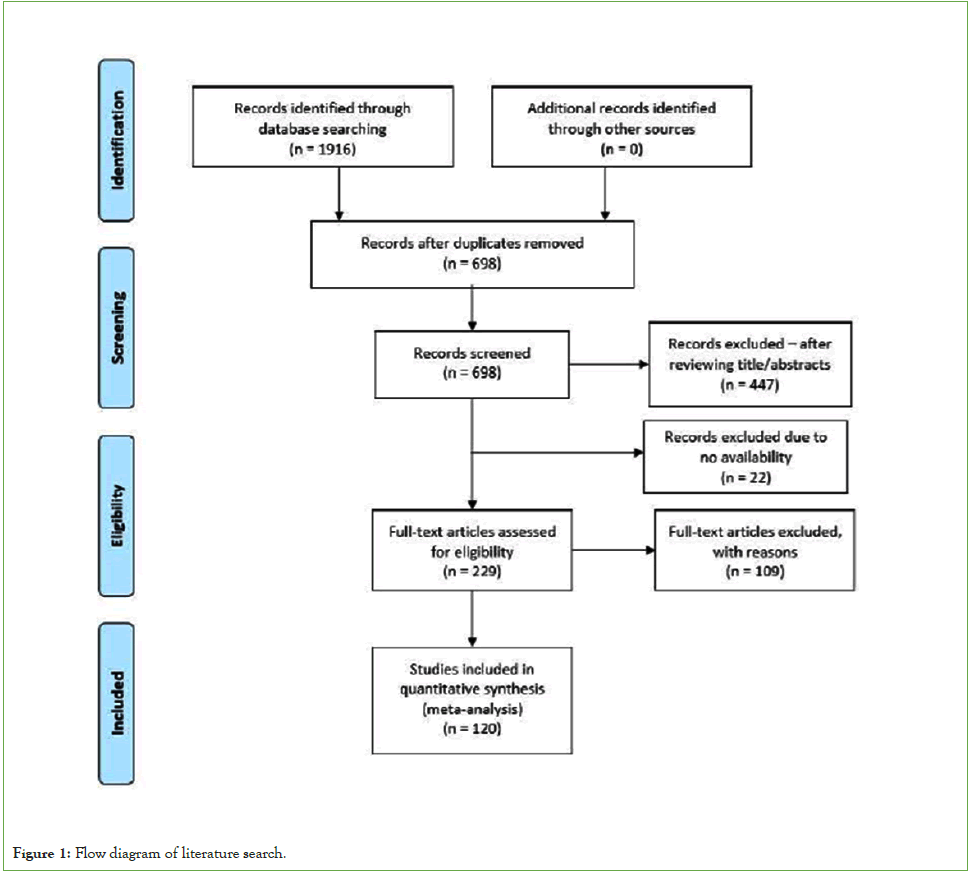
Figure 1: Flow diagram of literature search.
Study population
Characteristics of the patient population are shown in Table 1. Mean age was 61 with a standard deviation of 7. The majority of the patients was male and arterial hypertension was identified as the most frequent comorbidity. Acute aortic dissection type A and atherosclerotic aneurysm were the most common indications for surgery.
| Characteristics | Temperature group 1 sample size n (%) | Temperature group 2 sample size n (%) | Temperature group 3 sample size n (%) |
|---|---|---|---|
| Number of patients | 12495 (39%) | 11655 (36%) | 8173 (25%) |
| Age (years ± SD) | 61.2 ± 7 | 60.1 ± 7 | 61.8 ± 6 |
| Male | 8343 (67%) | 8219 (70%) | 5445 (67%) |
| Arterial hypertension | 7267 (74%) | 3714 (69%) | 4642 (67%) |
| Diabetes mellitus | 721 (9%) | 499 (10%) | 556 (8%) |
| Coronary artery disease | 1897 (21 %) | 1510 (18%) | 1236 (22%) |
| Renal impairment | 434 (6%) | 684 (10%) | 411 (10%) |
| Prior stroke | 786 (8%) | 641 (8%) | 515 (8%) |
| Chronic lung disease | 1309 (16%) | 1093 (13%) | 605 (14%) |
Table 1: Patient characteristics and risk factors.
Operative outcomes
The mean CPB time was 170.5 minutes for group 1, 183.5 minutes for group 2, and 190.1 minutes for group 3. Mean duration of x-clamp time and circulatory arrest was shorter for temperature group 3 compared with the others (x-clamp time: TG 1 90.5 minutes vs. TG 2 104 minutes vs. TG 3 61.1 minutes, respectively; circulatory arrest time: TG 1 28.3 minutes vs. TG 2 29.9 minutes vs TG 3 26.5 minutes, respectively). Note that, TG 1 and TG 2 had a higher rate of more complex procedures. Total arch replacement ranged from 38,8% to 63,3% (TG 1, TG2) compared to 25,3% (TG3). Further details are presented in Table 2.
| Variable | Temperature group 1 sample size n (%) |
Temperature group 2 sample size n (%) |
Temperature group 3 sample size n (%) |
|---|---|---|---|
| CPB (min) | 170.5 | 183.5 | 190.1 |
| Cross-clamp time (min) | 90.5 | 104 | 61.1 |
| Circulatory arrest time (min) | 28.3 | 29.9 | 26.5 |
| Ascending aorta replacment | 672 (6.3%) | 594 (6%) | 1114 (18.5%) |
| Hemiarch replacement | 6208 (55.3%) | 3030 (30.4%) | 3597 (64.2%) |
| Total arch replacement | 4578 (38.8%) | 6466 (63.3%) | 1678 (25.3%) |
Table 2: Intraoperative results and surgical procedure.
Clinical outcomes
Early mortality rate was 5.9% in TG 1 (≥ 25°C), 8.6% in TG 2 (25-20°C) and 7.6% in TG 3 (≤ 20°C), respectively. Intergroup comparison was associated with a lower rate in TG 1 (OR=1.42, 95% CI, 1.09-1.85 and OR=1.44, 95% CI, 1.16-1.78, respectively for TG 1). The p-value for the group difference in early mortality has shown a trend to significance (TG 1 vs. TG 3 p=0.01; TG 1 vs. TG 3 p=0.004) (Figure 2).
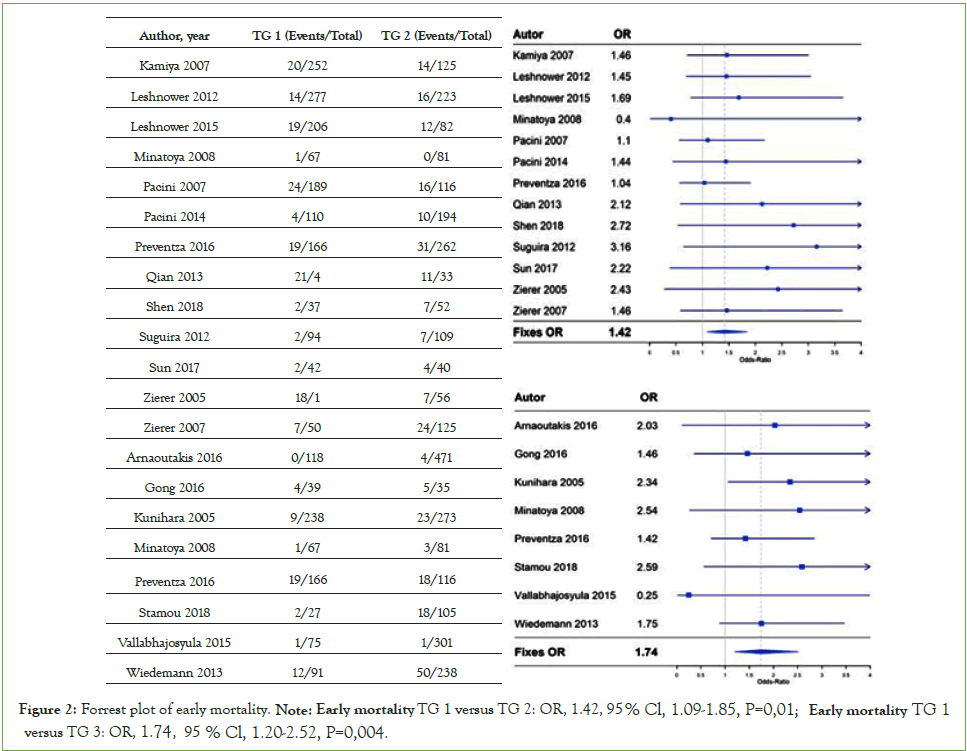
Figure 2: Forrest plot of early mortality. Note: Early mortality TG 1 versus TG 2: OR, 1.42, 95% Cl, 1.09-1.85, P=0,01; Early mortality TG 1 versus TG 3: OR, 1.74, 95% Cl, 1.20-2.52, P=0,004.
New postoperative neurologic complications occurred in 10.6% TG 1 vs. 13.6% TG 2 vs. 14.5% TG 3, respectively (TG 1 vs. TG 2, p=0.0002; TG 1 vs. TG 3 p=0.002). Comparison between the three temperature groups, TG 1 (>25°C) was associated with a lower postoperative stroke rate (OR=1.48, 95% CI, 1.20- 1.82 and OR=1.42, 95% CI, 1.16-1.73, respectively for TG 1). Differentiating between PND and TND, we found similar findings with an advantage for TG1 (PND: OR=1.20, 95% CI, 0.87-1.66 and OR=1.62, 95% CI, 1.07-1.2.46, respectively for TG 1; TND: OR=1.49, 95% CI, 1.15-1.92 and OR=1.56, 95% CI, 1.01-2.43, respectively for TG 1) (Figure 3).
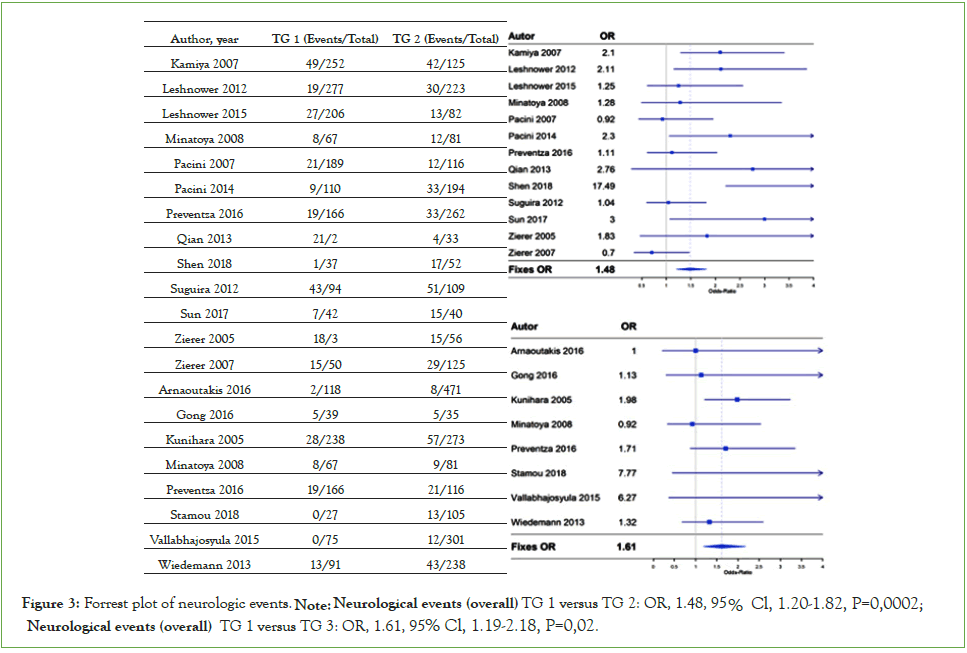
Figure 3: Forrest plot of neurologic events. Note: Neurological events (overall) TG 1 versus TG 2: OR, 1.48 , 95% Cl, 1.20-1.82, P=0,0002; Neurological events (overall) TG 1 versus TG 3: OR, 1.61, 95% Cl, 1.19-2.18, P=0,02.
There was no significant difference between TG 1, TG 2, and TG 3 in renal failure and re-exploration for bleeding (renal failure-TG 1 vs. TG 2: OR=1.20, 95% CI, 0.91-1.57, p=0.19 and TG 1 vs. TG3: OR=0.94, 95% CI, 0.67-1.32, p=0.73; re-exploration for bleeding- TG 1 vs. TG 2: OR=1.10, 95% CI, 0.80-1.53, p=0.55 and TG 1 vs. TG 3: OR=1.92, 95% CI, 1.26-2.94, p=0.0025) (Figure 4).
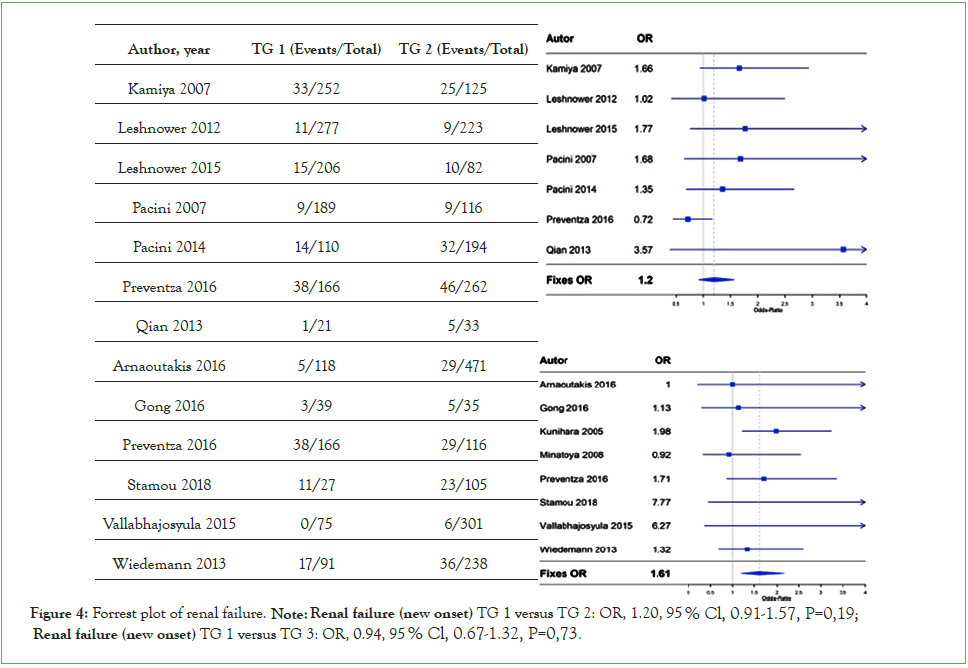
Figure 4: Forrest plot of renal failure. Note: Renal failure (new onset) TG 1 versus TG 2: OR, 1.20, 95% Cl, 0.91-1.57, P=0,19; Renal failure (new onset) TG 1 versus TG 3: OR, 0.94, 95% Cl, 0.67-1.32, P=0,73.
Discussion
The classic treatment of aortic arch pathologies is performed during open distal anastomosis [10]. Thus, physiologic blood flow to the brain and visceral organs is disrupted for the time of completion of aortic arch repair [6]. Different strategies to prevent neurological and visceral complications have been advocated. Historically, open aortic surgery has been performed in Deep Hypothermic Circulatory Arrest (DHCA), as introduced by Griepp, et al. in 1975 [3]. This strategy is based on the depression of cerebral metabolism through deep hypothermia [7]. DHCA has the main advantage of simplicity and does not need any additional cannulation but relies only on hypothermia [11]. Recent data from the Society of Thoracic Surgery Database shows that it is the most commonly method used in the United States [12]. Nevertheless, there are severe limitations. DHCA is limited to 30 minutes. The risk of stroke increases significantly after 40 minutes [13]. The prolonged time of CPB needed for cooling and rewarming is associated with clotting disturbances and organ dysfunction [6]. To avoid severe complications of DHCA and enhance the duration of open aortic procedures, adjunct techniques of Retrograde Cerebral Perfusion (RCP) and selective Antegrade Cerebral Perfusion (ACP) with various levels of systemic hypothermia have been developed [6,14]. RCP is fast and easy to establish, but its efficacy in reaching the brain parenchyma is debated [15-17]. ACP, pioneered by Bachet and colleagues and Kazui and colleagues [18,19], offers a more physiologic method of cerebral perfusion. Despite a more complex cannulation and perfusion setup, ACP has been applied more frequently worldwide and seems to be the most promising tool for reducing morbidity and mortality in open aortic surgery [20,21]. Although ACP was originally mostly used as an adjunct to deep hypothermia, systemic cooling became non-essential for neuroprotection. Because of the continuous perfusion of the brain, ACP extended the time of circulatory arrest and has led to the use of warmer core temperatures [6,8]. Despite favourable clinical results [5-8,22-24], there are still concerns about using a mild to moderate core temperature with selective ACP during CA. Furthermore, there is no widely accepted consensus regarding the optimal strategy for cerebral and organ protection.
It has been shown that brain oxygen consumption drops down to 50% of the baseline value at 28°C. Further cooling below 28°C does not decrease brain oxygen consumption effectively [25]. At the same time, regional cerebral blood flow under ACP conditions is decreased when combined with temperatures below 28°C [26]. The combination of reduced brain oxygen consumption with adequate regional blood flow at 28°C systemic temperature should allow for effective cerebral protection during aortic surgery [7].
In our present analysis, consisting of more than 32,000 patients, using a temperature level ≥ 25°C is associated with a significantly lower 30 day mortality (p=0.004). Furthermore, we observed a significantly lower incidence of postoperative neurologic events for the same temperature level (p=0.002). The advantage of a warmer temperature level was still present when differentiating between permanent and transient neurologic deficits. Our analysis did not show significant effects of temperature management on the occurrence of renal failure or re-exploration for bleeding.
Our findings are in line with Fan, et al. and Tian, et al. compared four cerebral protection strategies in open aortic surgery [27,28]. In this meta-analysis, including more than 6500 patients, DHCA is inferior to other techniques in terms of mortality and neurologic events [27]. There is a clear recommendation for using moderate to mild hypothermia adjunct to selective cerebral perfusion. Of note, Tian et al. even indicates a superiority of moderate to mild hypothermia in combination with selective antegrade cerebral perfusion in terms of stroke. The meta-analysis of Tian, et al. reveals the concern that direct canulation of supraaortic vessels with a greater chance of dislodging atherosclerotic thrombi is associated with a higher stroke rate [28-30].
Englum, et al. compared all different combinations of neuroprotection during aortic arch surgery using data of more than 12,500 patients from the Society of Thoracic Surgeons database. The authors found that DHCA was associated with the highest risk of the combined end point of operative mortality or neurologic complications. Moreover, a moderate to mild CA with ACP was favourably for all outcomes compared to all other strategies [12].
Our analysis shows that using a mild to moderate temperature level which has only been used with selective cerebral perfusion during circulatory arrest reduces mortality and the risk of neurological events. Despite the proven safety of warmer temperature levels, antegrade cerebral perfusion extend the duration of the safe time of circulatory arrest to approximately 60 minutes. In contrast, DHCA alone is sufficient for 30-40 minutes [13]. This can be helpful even in the setting of total arch replacement or acute aortic dissection with true lumen collapse of the supraaortic vessels.
Conclusion
To avoid severe complications of DHCA and enhance the duration of open aortic procedures, adjunct techniques of retrograde cerebral perfusion and selective antegrade cerebral perfusion with various levels of systemic hypothermia have been developed. RCP is fast and easy to establish, but its efficacy in reaching the brain parenchyma is debated. We focused on the influence of different temperature levels during CA. We did not perform a comparison between different cerebral perfusion strategies over DHCA alone. However, we will address this question in our future research. This can be helpful even in the setting of total arch replacement or acute aortic dissection with true lumen collapse of the supraaortic vessels.
Limitations and Data Availability Statement
A limitation of the present meta-analysis is the heterogeneous nature of aortic arch pathologies and variations in operative strategies. Inconsistent reporting of systemic outcomes has further limited our assessment. All data is available on request from the authors.
References
- Easo J, Weigang E, Hölzl PP, Horst M, Hoffmann I, Blettner M et al. Influence of operative strategy for the aortic arch in DeBakey type I aortic dissection: analysis of the German Registry for Acute Aortic Dissection type A. J Thorac Cardiovasc Surg. 2012;144:617-623.
[Crossref] [Google Scholar] [PubMed]
- Czerny M, Fleck T, Zimpfer D, Dworschak M, Hofmann W, Hutschala D, et al . Risk factors of mortality and permanent neurologic injury in patients undergoing ascending aortic and arch repair. J Thorac Cardiovasc Surg. 2003;126:1296-1301.
[Crossref] [Google Scholar] [PubMed]
- Griepp RB, Stinson EB, Hollingsworth JF, Buehler D. Prosthetic replacement of the aortic arch. J Thorac Cardiovasc Surg. 1975;70:1051-1063.
[Crossref] [Google Scholar] [PubMed]
- Di Eusanio M, Wesselink RMJ, Morshuis WJ, Dossche KM, Schepens MA. Deep hypothermic circulatory arrest and antegrade slective cerebral perfusion during ascending aorta–hemiarch replacement: A retrospective comparative study. J Thorac Cardiovasc Surg. 2003;125:849-854.
[Crossref] [Google Scholar] [PubMed]
- El-Sayed Ahmad A, Papadopoulos N, Risteski P, Mortiz A, Zierer A. The standardized concep of moderate-to-mild systemic hypothermia during selective antegrad cerebral perfusion for all-comers in aortic arch surgery: single-center experiece in 587 consecutive Patients over a 15 year period. Ann Thorac Surg. 2017;104:49-55.
[Crossref] [Google Scholar] [PubMed]
- Zierer A, Ali El-Sayed Ahmad A, Papadopoulos N, Mortiz A, Diegeler A, Urbanski P. Selective antegrad cerebral perfusion and mild (28°C-30°C) systemic hypothermic circulatory arrest for aortic arch replacement: Results from 1002 patients. J Thorac Cardiovasc Surg. 2012;144:1042-1050.
[Crossref] [Google Scholar] [PubMed]
- Zierer A, El-Sayed Ahmad A, Papadopoulos N, Detho F, Risteski P, Moritz A et al. Fifteen years of surgery for acute type A aortic dissection in moderate-to-mild systemic hypothermia. Eur J Cardiothorac Surg. 2017;51:97-103.
[Crossref] [Google Scholar] [PubMed]
- Urbanski P, Lenos A, Bougioukakis P, Neophytou I, Zacher M, Diegeler A. Mild-to-moderate hypothermia in aortic arch surgery using circulatory arrest: a change of paradigm? Eur J Cardiothorac Surg. 2012;41:185-191.
[Crossref] [Google Scholar] [PubMed]
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analysis of studies that evaluate healthcare interventions: Explanations and elaborations. BMJ. 2009;339:b2700.
[Crossref] [Google Scholar] [PubMed]
- Livesay JJ, Cooley DA, Duncan JM, Ott DA, Walker WE, Reul GJ. Open aortic anastomosis: Improved results in the treatment of aneurysms of the aortic arch. Circulation. 1982;66(Pt 2):I122-1127.
[Google Scholar] [PubMed]
- Hameed I, Rahouma M, Khan FM, Wingo M, Demetres M, Tam DY, et al. Cerebral protection strategies in aortic arch surgery: A network meta-analysis. J Thorac Cardiovasc Surg. 2020;159:18-31.
[Crossref] [Google Scholar] [PubMed]
- Englum BR, He X, Gulack BC, Ganapathi AM, Mathew JP, Brennan et al. Hypothermia and cerebral protection strategies in aortic arch surgery: a comparative effectiveness analysis from the STS Adult Cardiac Surgery Database. Eur J Cardiothorac Surg. 2017;52:492-498.
[Crossref] [Google Scholar] [PubMed]
- Gega A, Rizzo JA, Johnson MH, Tranquilli M, Farkas EA, Elefteriades JA. Straight deep hypothermic arrest: experience in 394 patients supports its effectiveness as a sole means of brain preservation. Ann Thorac Surg. 2007;84:759-766.
[Crossref] [Google Scholar] [PubMed]
- Estrera AL, Miller CC, Lee TY, Shah P, Safi HJ. Ascending and transverse aortic arch repair: The impact of retrograde cerebral perfusion. Circulation. 2008;118:160-166.
- Ehrlich MP, Ergin MA, McCullough JN, Lansman SL, Galla JD, Bodian CA, et al. Results of immediate surgical treatment of all acute type A dissections. Circulation. 2000;102:248-252.
[Crossref] [Google Scholar] [PubMed]
- Gaudino M, Ivascu N, Cushing M, Lau C, Gambardella I, Di Franco A, et al. Retrograde perfusion through superior vena cava reaches the brain during circulatory arrest. J Thorac Dis. 2018;10:1563-1568.
[Crossref] [Google Scholar] [PubMed]
- Cheung AT, Bavaria JE, Pochettino A, Weiss SJ, Barclay DK, Stecker MM. Oxygen delivery during retrograde cerebral perfusion in humans. Anesth Analg. 1999;88:8-15.
[Crossref] [Google Scholar] [PubMed]
- Bachet J, Guilmet D, Goudot B, Termignon JL, Teodori G, Dreyfus G, et al. A new technique of cerebral protection during operations on the transverse aortic arch. J Thorac Cardiovasc Surg. 1991;102:85-93.
[Google Scholar] [PubMed]
- Kazui T, Inoue N, Yamada O, Komatsu S. Selective cerebral perfusion during operation for aneurysms of the aortic arch: a reassessment. Ann Thorac Surg. 1992;53:109-114.
[Crossref] [Google Scholar] [PubMed]
- de Paulis R, Czerny M, Weltert L, Bavaria J, Borger MA, Carrel TP. et al. Current trends in cannulation and neuroprotection during surgery of the aortic arch in Europe. Eur J Cardiothorac Surg. 2015;47:917-923.
[Crossref] [Google Scholar] [PubMed]
- Kazui T, Washiyama N, Muhammad BA, Terada H, Yamashita K, Takinami M. Improved results of atherosclerotic arch aneurysm operations with a refined technique. J Thorac Cardiovasc Surg. 2001;121:491-499.
[Crossref] [Google Scholar] [PubMed]
- Pacini D, Leone A, di Marco L, Marsilli D, Sobaih F, Turci S, et al. Antegrade selective cerebral perfusion in thoracic aorta surgery: safety of moderate hypothermia. Eur J Cardiothorac Surg. 2007;31:618-622.
[Crossref] [Google Scholar] [PubMed]
- Kamiya H, Hagl C, Kropivnitskaya I, Böthig D, Kallenbach K, Khaladj N, et al. The safety of moderate hypothermic lower body circulatory arrest with selective cerebral perfusion: A propensity score analysis. J Thorac Cardiovasc Surg. 2007;133:501-599.
[Crossref] [Google Scholar] [PubMed]
- Saritas A, Kervan U, Vural KM, Kucuker SA, Yavas S, Birincioglu LC. Visceral protection during moderately hypothermic selective antegrade cerebral perfusion through right brachial artery. Eur J Cardiothorac Surg. 2010;37:669-676.
[Crossref] [Google Scholar] [PubMed]
- Strauch JT, Spielvogel D, Haldenwang PL, Zhang N, Weisz D, Bodian CA, et al. Impact of hypothermic selective cerebral perfusion compared with hypothermic cardiopulmonary bypass on cerebral hemodynamics and metabolism. Eur J Cardiothorac Surg. 2003;24:807-816.
[Crossref] [Google Scholar] [PubMed]
- Usui A, Oohara K, Murakami F, Ooshima H, Kawamura M, Murase M. Body temperature influences regional tissue blood flow during retrograde cerebral perfusion. J Thorac Cardiovasc Surg. 1997;114:440-447.
[Crossref] [Google Scholar] [PubMed]
- Fan S, Li H, Wang D, Wu C, Pan Z, Li Y, et al. Effects of four major brain protection strategies during proximal aortic surgery: A systematic review and network meta-analysis. Int J Surg. 2019;63:8-15.
[Crossref] [Google Scholar] [PubMed]
- Tian DH, Wan B, Bannon PG, Misfeld M, LeMaire SA, Kazui T, et al. A meta-analysis of deep hypothermic circulatory arrest versus moderate hypothermic circulatory arrest with selective antegrade cerebral perfusion. Ann Cardiothorac Surg. 2013;2:148-158.
[Crossref] [Google Scholar] [PubMed]
- Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. 2018;27(6):1785-1805.
[Crossref] [Google Scholar] [PubMed]
- Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36(3):1-48.
Citation: Huber F, Schachner B, Gottsberger JZ, Benedikt P, Zierer AF (2023) Evidence of Global Warming: A Meta-Analysis of Temperature Management in Aortic Surgery. J Vasc Surg. 11:534.
Copyright: © 2023 Huber F, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

