Citations : 2345
Dentistry received 2345 citations as per Google Scholar report
Indexed In
- Genamics JournalSeek
- JournalTOCs
- CiteFactor
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2025) Volume 15, Issue 3
Evaluation of the Early Implant Loss in Elderly Patients: A 10 Years Retrospective Study
Aristides da Rosa Pinheiro, Marina Pinheiro, Valquiria Quinelato, Jose Jorge Schoichet, Rackel Gonçalves, Alexandre Campos Montenegro, Telma Aguiar, Aldir Nascimento Machado and Priscila Ladeira Casado*Received: 16-Aug-2023, Manuscript No. DCR-23-22729; Editor assigned: 18-Aug-2023, Pre QC No. DCR-23-22729 (PQ); Reviewed: 11-Sep-2023, QC No. DCR-23-22729; Revised: 09-Jan-2025, Manuscript No. DCR-23-22729 (R); Published: 16-Jan-2025
Abstract
Objective: The present study aimed to evaluate the treatment with osteointegrated implants in elderly patients, by a retrospective and cross-sectional analysis.
Background: Despite the local and systemic peculiarities that accompany the elderly patient, the success rate can be high, provided that specific care is considered in clinical and surgical procedures.
Materials and methods: We evaluated 173 patients records of research participants who received late loading implants during 10 years. The specifications of the implants placed and the respective factors associated with success rates were described, including patients characteristics, the types of prostheses, the use of drugs and systemic diseases and region of implant placement. From a total of 1,000 patients` records analyzed, 173 research participants were included and evaluated in this study, being 104 (60%) women and 69 (40%) men, with a mean age of 63 ± 4.52 years. A total of 121 (70%) research participants had systemic disease and 106 (61.3%) used drugs.
Results: It was observed a greater tooth loss in the maxilla compared to the mandible (p<0.001), as well as a higher number of partial dental absence in the mandible (p<0.001). From the total of 805 implants placed, 33 (4%) implants were lost, with a higher incidence in the maxilla.
Conclusions: The success implant rate was 96%. It was concluded that the success rate after implant placement in elderly patients is high, even with medication use and systemic disease.
Keywords
Osseointegrated implant; Elderly patient; Primary implant loss; Implant successIntroduction
At present, it is possible to observe that the population of the elderly over 60 years is growing at an accelerated rate, when compared to any other age group. The last Census conducted by the Brazilian Institute of Geography and Statistics (IBGE) in 2010 showed that individuals over 60 years-old already numbered more than 20.5 million people, representing 11% of the Brazilian population. In 2012, the group of people aged 60 years and over corresponded to 12.8% of the population. In 2016, this percentage rose to 14.4%, evidencing the aging of Brazilians [1].
Current projections by the World Health Organization, 2022, affirmed that the number of people aged 60 years and older outnumbered children younger than 5 years. In addition, between 2015 and 2050, the proportion of the world's population over 60 years will nearly double from 12% to 22% which indicates that by the middle of the century this group will be equivalent to 30% of the countryâ??s population. By the year 2025, it is expected to grow by 23%, or something around 694 million older people, with the prospect of Brazil being the sixth country in the world in the number of the elderly, reaching a figure of 33.4 millions of people [2].
The strong growth in the life expectancy rate of the elderly population leads people of this age group to seek improvement in their survival conditions, at which time these elderly people also seek a more qualified dental treatment, in order to replace them the missing dental elements. To support these aspirations, modern dentistry offers oral rehabilitation treatment with the installation of titanium implants to retain and support prostheses.
From the 1970's onwards, Professor Per Ingvar Branemark, a Swedish researcher, showed the world a system of retention of the total prosthesis with osseointegrated implants, which revolutionized dentistry worldwide, which became known as the Branemark protocol. In the following decades, several scientific publications have shown that osseointegrated implants can also be used to support single, partial or total removable prostheses with excellent patient acceptance [3].
Considering that the elderly present more oral health impairment than the young, being mostly partial or total edentulous, this group of patients is a strong candidate for treatment with dental implant. However, the presence of systemic diseases and the continuous use of medications make this population a group with specific clinical characteristics, which should be considered during implant installation.
The presence of comorbidities and the use of medications may directly affect bone remodelling, through the chemical alteration of the bone composition. Experimental studies have shown that estrogen deficiency affects bone mineralization and remodelling. In the same way, there is low periosteal cell differentiation and decrease of the osteoblastic response to the mechanical stimuli, besides insufficient vascularization [4]. The increased inflammatory reaction in these patients also promotes adverse effects during bone repair by stimulation of bone resorption.
However, the exact influence of medications and systemic diseases on osseointegration of dental implants is still unclear. In the past, it was believed that as osseointegration is dependent on bone healing, it could be altered according to age, based on the age and osteoporosis ratio and in reports of bone involvement in the elderly. Currently, success in implantology is known to be unrelated to age, confirming previous data from the Toronto study in 1994, the first study discussing osseointegration in elderly patients, stating that the fact of being elderly is not a contraindication to the success of long-term osseointegration [5]. There is predictability and safety in the rehabilitation with implants of geriatric patients, increasing the quality of life of this population, with results similar to those observed in young patients.
The increase in the number of research, however, has been demonstrating that the treatment is not always successful, and try to identify the factors associated with implantodontic failures. According to Esposito et al., biological failures are defined as an inability of the tissue to establish or maintain osseointegration, being divided into primary failure (failure during the osseointegration process) and secondary failures (failure to maintain previously established osseointegration). In order to detail the previous classifications, Askary et al. classified the implant failures, considering seven aspects: etiology of failure; failure time; origin of the infection; clinical-radiographic state; personal responsibility; type of fault; characteristics of the support fabric. To date, this is the main classification that includes failures that occur during the second surgical act (between the osseointegration period and implant loading).
Based on the current aging population, it is known that treatment with osseointegrated implants can significantly improve the quality of life of the elderly patients [6]. The installation of implants, replacing conventional prostheses has revolutionized the functional, aesthetic and psychological characteristics in this population. In addition, the influence of oral health on the oral health of elderly patients has been demonstrated in some studies that indicate a higher mortality in patients who lost more teeth.
However, recent data on the characteristics of the elderly population receiving dental implants are scarce and often do not direct or clarify predictability regarding success rate, especially in the Brazilian population [7].
Therefore, considering the perspective of continuous ageing in the Brazilian and world population, and the increase of oral rehabilitation with the installation of osseointegrated implants, this all retrospective seeks to evaluate and describe the clinical and epidemiological results after implant placement and its possible correlation with early implant loss in order to become evident the different aspects associated with implant dentistry treatment. Our hypothesis is that, despite the local and systemic peculiarities that accompany the elderly patient, the success rate can be high, provided that specific care is considered in clinical and surgical procedures [8].
Materials and Methods
This is a 10 years retrospective, descriptive, observational, crosssectional research in nature. The present study was approved by the Research Ethics Committee of the Faculty of Medicine of the Universidade Federal Fluminense, under the number 2.631.531.
Sample selection
One thousand medical records in the archives of the specialization course in implant dentistry of the Fluminense federal university were evaluated for this study. The criteria for inclusion of the sample were from the medical records of 60 years-old patients or older, who received treatment with osseointegrated implants and who were rehabilitated with prostheses on the implants after the periods of osseointegration (late load), in the period between January 2010 and December 2020. We excluded from the present study the medical records of patients less than 60 years-old, the incomplete medical records and that from the patients who could not be submitted to treatment with the implant, and patients submitted to rehabilitation with an implant with immediate loading [9].
Research tools
The patients charts were used as instruments of this research, according to the inclusion criteria, as well as data collection sheet containing the necessary items that will respond to the requirements of the specific objectives. The study was performed by analyzing and collecting data from the patient records that were rehabilitated after the recommended periods for osseointegration of the implants. All the evaluated records were duly filled out by the students and teachers who make up the faculty of the course. The script with the analyzed data is part of a data collection form attached to this project [10].
Success criteria
The success criterion applied in the present study was the absence of loss of implants installed, according to Esposito et al., Implants removed before or at the time of the second surgical time (in the osteointegration period of 4-6 months) at the time of casting or at the final stage of prosthesis placement were considered as failure.
Statistical analysis
The statistical analysis was of the descriptive type, considering the median and standard deviation of the numerical variables evaluated, as well as the absolute numbers and percentages of the nominal variables evaluated. The Microsoft Office 2013 Excel program was used for the standardization of calculations and graphing.
To evaluate the correlation between dental losses in the arches studied and the number of implants installed and lost, Prisma GraphPad 6.0 software (GraphPad Software, La Jolla, CA-USA) was used. The chi-square test correlated the clinical data of these nominal variables, with significance level of 0.05%. The risk of implant loss was evidenced by the Odds Ratio (OD), constructing a 95% confidence interval. Values of p<0.05 were considered significant [11].
Results
General characteristics of the studied population
From a total of 1,000 medical records, 173 research participants were included in this study, of which 104 (60%) were women and 69 (40%) were men, with a mean age of 63 ± 4.52 years. A total of 121 (70%) participants had systemic disease, 11 (6.3%) had bruxism, and 106 (61.3%) used medication, among them antihypertensive, antihyperglycemic, antimicrobial, non-steroidal anti-inflammatory, anti-inflammatory steroid, anxiolytic, diuretic, anticoagulant, antihistamine, antihyperlipemic, calcium supplementation, hormone replacement and anti-acid (Table 1).
| Parameters | Participants (n=173) |
|---|---|
|
Gender |
|
|
Female |
104 (60%) |
|
Male |
69 (40%) |
|
Age |
63 ÃÂ?± 4.52 |
|
Female age |
63 ÃÂ?± 4.47 |
|
Male age |
63 ÃÂ?± 4.71 |
|
Sistemic diseases |
121 (70%) |
|
Hypertension |
76 (44%) |
|
Diabetes |
11 (6.3%) |
|
Gastritis |
21 (12.1%) |
|
Artritis |
6 (3.5%) |
|
Others* |
25 (14.4%) |
|
Bruxism |
11 (6.3%) |
|
Use of medication |
106 (61.3%) |
|
Note: *Others diseases include heart diseases, depression, glaucoma, neurological disorders |
|
Table 1: General characteristics of studied population.
Oral characteristics of the studied population
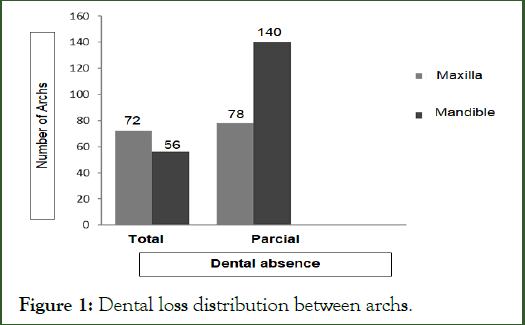
Considering the intra-oral characteristics related to missing teeth, a total of 2,939 dental absences were observed in 173 research participants. The total absence of teeth was observed in 128 (37%) arches, with 2,048 dental losses. The partial absence of teeth (891 dental losses) was present in 218 (63%) arches. Figure 1 shows the distribution of types of tooth loss in the maxilla and mandible of the research participants, with a higher number of total dental absence in the maxilla compared to the mandible (p<0.001), as well as a higher number of dental absence in the mandible relative to the maxilla (p<0.001) (Table 2).
Figure 1: Dental loss distribution between archs.
| Dental loss type | Maxilla | Mandible | p-valor |
|---|---|---|---|
| Total | 1152 | 896 | 0.0001 |
| Partial | 319 | 572 | |
| Total dental loss | 1471 | 1468 | 2939 |
Table 2: Correlation between partial or total dental loss inside the mandible and maxila.
Implants placed on research participants
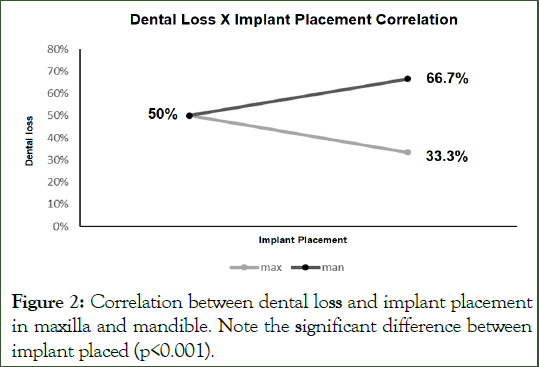
Table 3 shows the specifications of the osseointegrated implants placed in the research participants, considering the implant system, type of platform and number of implants installed. Of the total of 805 implants placed, 537 (66.7%) were installed in the mandible and 268 (33.3%) in the maxilla.
| Implant system | Platform types | Total | ||
|---|---|---|---|---|
| External hexagon | Intern hexagon | Morse cone | ||
| ConexÃÂ?£o | 524 | 86 | 7 | 617 |
| SIN* | 151 | 1 | 9 | 161 |
| Neodent | 6 | 6 | 1 | 13 |
| Ankylos | - | - | 4 | 4 |
| Intralock | 10 | - | - | 10 |
| Total | 691 | 93 | 21 | 805 |
| Note: *SIN, SÃÂ?£o Paulo- Brazil | ||||
Table 3: Characteristics of the implant placed in research participants.
The chi-square test revealed a significant difference between the number of teeth lost in the arches (total or partial) and the number of implants installed in the maxilla and mandible, with a greater installation of implants in the mandible in relation to the maxilla (p<0.001) (Figure 2).
Figure 2: Correlation between dental loss and implant placement in maxilla and mandible. Note the significant difference between implant placed (p<0.001).
Expectations of research participants
During the patient’s anamnesis, the main reason for the rehabilitation with osseointegrated implants was questioned. The 173 participants included had as main answers, obtaining aesthetics and the possibility of recovery of the masticatory function (Table 4).
| Reason | Participants (n=173) |
| Aesthetics | 39 (22.2%) |
| Masticatory function | 50 (28.9%) |
| Masticatory function/aesthetic | 84 (48.9%) |
Table 4: Main reason for implant rehabilitation.
Failure rates
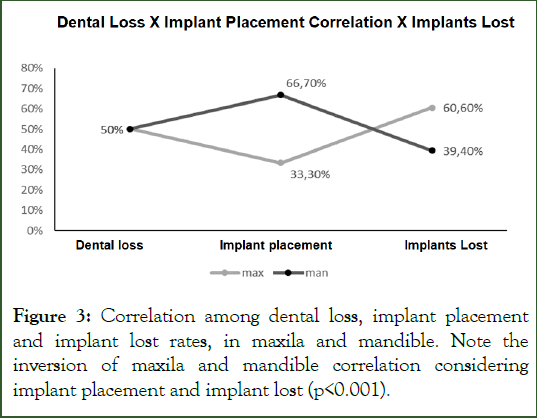
A total of 33 implants were lost, 20 implants during the period of osseointegration and at the end of this period, and 13 implants were not stable and were lost at the time of implant installation. Of the 33 (4%) implants lost, 20 (60.6%) were installed in the maxilla and 13 (39.4%) in the mandible. The success rate of the implants installed until the installation of the prosthesis was 96% [12].
The chi-square test showed that, despite the higher jaw implant index, there was a highly significant difference in the percentage of implant loss, with a higher incidence of maxilla loss compared to the mandible (p=0.002) (Figure 3). The maxilla is 3 times more likely to lose an implant early compared to the mandible in the group of participants studied (OR 3.08 CI: 1.51-6.29). Benefits and drawbacks of using phages as antimicrobials.
Figure 3: Correlation among dental loss, implant placement and implant lost rates, in maxila and mandible. Note the inversion of maxila and mandible correlation considering implant placement and implant lost (p<0.001).
Post-surgery intercurrences
We observed the reports of the patients, at the moment of removal of the suture (one week after) of the following intercurrences, in the 173 medical records:
• Regarding the appearance of edema in the postoperative period, 31 (17.9%) reports of patients who had postoperative edema were found, of which 4 (2.3%) were reports of signs of infection in the operated region. Sixteen (9.2%) reports with residual (discrete) edema on removal of the suture.
• Twenty-six (15%) cases of bruising were reported on the clinical record, at the time of removal of the suture.
• Among all the analysed sample, a patient record with paresthesia complaint was found in the operated region, which normalized in 6 months.
• In 141 (81.5%) medical records, no records of any postoperative complications were found.
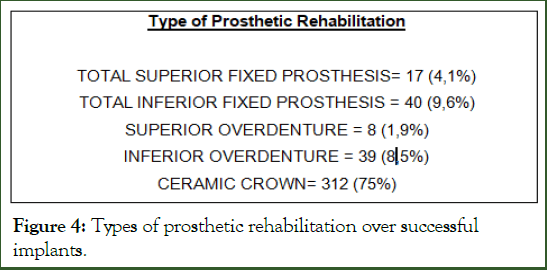
Characteristics of prosthetic rehabilitation
From a total of 805 implants installed, 33 (4%) implants were lost and 772 (96%) implants were submitted to rehabilitation with fixed total prostheses, muco-supported overdentures and metal-ceramic crowns, as described in Figure 4.
Figure 4: Types of prosthetic rehabilitation over successful implants.
Discussion
People worldwide are living longer. Today most people can expect to live into their sixties and beyond. Every country in the world is experiencing growth in both the size and the proportion of older persons in the population. By 2050, the world’s population of people aged 60 years and older will double (2.1 billion). The number of persons aged 80 years or older is expected to triple between 2020 and 2050 to reach 426 million people. This lead to increase the risk of systemic diseases and use of medication, which can affect the bone homeostases, essential for osseointegration process and implant success a long term. Therefore, the present study aimed to evaluate and describe, retrospectively, the oral treatment performed in the elderly patients, through the use of osseointegrated implants. The results showed that (i) The main reasons for the demand for rehabilitation with dental implants by the elderly patients were reestablishment of function and aesthetics together; (ii) Elderly patients submitted to treatment with implants commonly present with systemic diseases and drug therapy; (iii) There is a predominance of partial edentulous in this elderly population, mainly in the mandible; (iv) Total edentulism is predominant in the maxilla; (v) However, most of the implants were installed in the mandible, mainly using platform of external hexagon type; (vi) The success rate was 96% in implant osseointegrated, with a 4% loss of total implants installed; (vii) The maxilla was 3 times more likely to lose an implant early; (viii) The majority of the patients did not present surgical complications; (ix) Patients were able to be rehabilitated with fixed total prostheses, mucosupported overdentures implants and metal-ceramic crowns [13]. Thus, this study supports the hypothesis that rehabilitation with osseointegrate implants in elderly patients, despite its peculiarities, related to age and systemic care, has a high success rate.
Epidemiological projections in Brazil, based on the Young-Adult Quotient (QIJ), indicate that for each set of 100 young people under the age of 15, there should be around 46 elderly people in 2025, compared to 10 in 1975. By 2050, the number of older people will exceed that of children. Of all the people living in Brazil in 2005, around 87% will be alive in 2025 (population, then 21 years-old), and 61% in 2050 (population, then, 50 yearsold or older). Together with this fact, in the Brazilian context, when discussing the oral health conditions of the elderly population, the total loss of teeth is still accepted by society as something normal and natural with the advancement of age.
The absence of one or more dental units generates significant changes in the stomatognathic system, negatively and significantly affecting patients’ quality of life. Implantology, despite being one of the most recent dental specialties, has been shown to be of fundamental importance for the rehabilitation and reestablishment of the oral, social and psychological health condition of the edentulous patient. Acording to World Health Organization, 1980, edentulism is a relevant type of functional incapacitation, and the most affected population is in a more advanced age group and its reflexes significantly impair the quality of life of the individuals affected - mainly due to its more advanced form, which is the total edentulism.
Our study identified total maxillary and mandibular edentulism, with a higher incidence in the maxilla [14]. The majority of patients included, over 60 years-old, had partial mandibular edentulism. In this sense the implants present themselves as a great opportunity to replace the missing teeth. All patients included in the study were rehabilitated with osseointegrated implants. However, for treatment with dental implants, we must consider that the elderly patients are part of a heterogeneous group that requires an individualized treatment plan, based on their medical conditions and future expectations. Therefore, it is important to recognize the functional status and autonomy of the patient, as well as the cost-benefit of the treatment, considering the main complaint of the elderly patient. In our retrospective study, we considered the inclusion of the evaluation of the main complaints of the rehabilitated patients, thus verifying that they were basically limited to the loss of aesthetics and masticatory function, representing 100% of the complaints that justified the search for the implant rehabilitation treatment.
According to Schimmel et al., the priority in the oral rehabilitation of the elderly with dental implants is the reestablishment of the oral function. Masticatory dysfunction and food choice limitation is closely associated with social limitations, poor oral health and nutritional deficiencies [15].
On the other hand, the partial or total loss of the teeth will not only affect the masticatory functions, but will also be affected by aesthetic deficiency. With the advancement of techniques in oral implantology, in recent years, it is possible to perform functional rehabilitations, with a high percentage of aesthetic success in patients of different ages.
In our clinical practice, we consider the treatment with elderly patients as an aesthetic and functional set, encompassing particularities pertinent to this age group. Therefore, we argue that a standardized protocol of treatment should not simply be a specific type of prosthesis to achieve function and aesthetics, but should rather have some criteria, such as: Oral comfort, reestablishment of facial height, age-compatible dental characteristics, adequate retention of the prosthesis, increasing patient confidence in the treatment performed, speech/ phonation, prosthetic design that facilitates oral hygiene, considering possible physical and cognitive limitations.
From the surgical point of view, two important aspects should be considered in the implant placement planning of the elderly patient: The need to minimize surgical trauma and the evaluation of medical risk factors that may influence osseointegration.
Old age and the presence of systemic diseases are often considered negative factors for implant placement. Kim, Yun, say that there is a reduction in the ability to maintain homeostasis with advancing age, increasing the risk of infections. However, it should be noted that diseases resulting from age should be distinguished from the fact of being old. The mere fact of being elderly is not a contraindication to implant procedures. Old healthy patients without systemic diseases can be treated with implants, as there is no evidence that bone metabolic changes, along the age, directly influence the osseointegration. Our study corroborates this fact to the high success rate. Of the total number of rehabilitated patients, 30% were healthy, as opposed to 70%, who had one or more systemic diseases, including controlled diabetes and hypertension, gastritis, arthritis and osteoporosis. There was no difference in success rate between these patients, after similar treatment with osseointegrated implants. However, it should be noted that all rehabilitated patients who had systemic disease were controlled by medication and were under medical care.
Although advanced age is not the main cause of implant failure, the presence of some medical conditions, including xerostomia, osteoporosis and diabetes, can cause slow healing, culminating in the need for a longer time for bone healing after implant implantation compared to young patients. Therefore, in our clinical protocol, preoperative exams, anamnesis and medical opinions, when necessary, are always incorporated into the treatment of the elderly patient, considered a multidisciplinary patient. Patients with 3 or more diseases should be classified as potential for multimorbity, requiring simultaneous medical follow-up to implant treatment.
According to a recent review of Schimmel et al., the main medical conditions that should be considered in the treatment plan for implant rehabilitation are: cardiovascular diseases, diabetes mellitus, osteoporosis, cancer, Parkinson's disease, dementia, xerostomia, rheumatism and nutritional deficiency. These diseases or the effect of medications used to treat them may influence implant placement, bone and soft tissue healing, and the long-term success of implant therapy. In our study, about 60% of patients evaluated in the 10-year period used medication for different medical conditions, with hypertension being the predominant disease. Similar results were found in a study by Lee et al., where the authors evidenced arterial hypertension in the majority of elderly patients, followed by diabetes, heart disease and kidney disease. Under these conditions, the authors do not contraindicate implant surgery, reaching high success rates, which corroborates with our clinical procedures in the implantology treatment of the elderly [16].
According to Hwang and Wang, the absolute contraindications for the installation of dental implants are myocardial infarction within 3-6 months, cerebral hemorrhage, heart valve replacement, treatment of malignant tumors and use of bisphosphonates for the treatment of osteoporosis. Relative contraindications include smoking, diabetes, cardiovascular disease, and thyroid disease. However, when properly treated and controlled these systemic diseases do not affect the success rate in implantology. Based on these studies, our clinical protocol in elderly patients included controlled patients with specific diseases that relatively contraindicate the implantation of the implant, evidencing the success of the therapy. In this sense, it is important to note that, in geriatric patients, despite the systemic conditions and the possible decrease of bone regeneration, the success rate in implant therapy is similar to that observed in young patients, reaching around 95%.
In clinical practice in prosthesis supported by implants, if we set up an absolute contraindication for the installation of implants, due to the high prevalence of systemic diseases, we may have an impossibility to restore the function and esthetics of the elderly patients. In our study, we achieved a 96% success rate in implant therapy in the elderly. Clinical osseointegration occurred adequately and the main complications were edema, with and without signs of infection, and one report of paresthesia, totaling 81.5% of elderly patients without postoperative complications. Similar finds were observed in a study by Lee et al., evaluating the success rate in 35 patients over 70 years old, who received a total of 118 implants, in which the presence of complications in 15% of the implants was found.
The process of osseointegration may suffer intercurrences which result in the loss of the implant. Therefore, the existing reactions at the bone-implant interface are influenced by the surgical technique, the health status of the recipient bone bed, the biocompatibility of the metal, the design and type of implant surface, as well as the conditions of application of loads transmitted to the implant. The initial stability of the implant and a period of free repair of loads are fundamental in this process [17].
Esposito et al, in 1998, classified the implant failure in two basic periods: Early failure (before osseointegration period) and later failure (after loading). In order to improve this classification of implant failure, Askary et al., considered in their failure classification the etiology, failure mode, failure type, failuring time, responsible personnel and reactions in different tissues type.
The time of evaluation in our study was based on Askary et al., classification, stage I (after implant placement) and stage II (with healing head or abutment insertion), excluding analysis during stage III of Askary et al. (after loading). In our study, the implants were not loaded during the evaluation period. A total of 4% of the implants were lost early, before the period of osseointegration. Similar results were found in Zarb, Schmitt, in patients over 65 years-old, who received 207 implants, with a success rate of 95.2%, and 10 implants lost (4.8%).
Curiously, the maxilla was 3 times more likely to lose an implant early than the mandible, in the patients evaluated in our study [18]. Bryant et al., analyzed and reported the effects of implant site, bone condition and age on the results of implant therapy, concluding that the implant sites are related to the potential of osseointegration, and the mandibular sites are more favourable in relation to the jaws. These findings corroborate with the Sixth Workshop on Periodontics that postulated a higher index of peri-implant disease and loss of maxillary implant compared to the mandible.
However, in our study, most of the implants were installed in the mandible, mainly using external hexagon type platform. This fact may reflect that the stabilization of mandibular total dentures with the use of osseointegrated implants is one of the great advances of modern dentistry. The stabilization of the mandibular total prosthesis with a minimum of 2 implants reduces peri-implant bone atrophy, increases masticatory efficiency, reduces masseter muscle atrophy and significantly increases the patient’s quality of life.
Due to the high success rate, the patients were rehabilitated according to the initial planning, with fixed total prostheses, muco-supported overdentures implants and metal-ceramic crowns. The rehabilitation of the total edentulous arches was, for the most part, with fixed lower total prostheses and lower overdentures. This fact is common in clinical practice in elderly patients, in whom maxillary total implanted upper prosthesis is only planned if there is no need for extensive regenerative procedures and in patients with general health, which do not represent the majority of the elderly patients. On the other hand, patients are generally satisfied with conventional maxillary prostheses, limiting the smaller number of implants installed in total edentulous maxilla.
The choice of fixed and removable total dentures in implantology has been discussed in several studies. However, maintaining adequate oral hygiene should be preserved, especially in geriatric patients, due to their systemic risks. Consequently, prostheses should be designed to ensure the feasibility of peri-implant cleaning, as implants in elderly patients are expected to remain in the mouth for life. Another important aspect is the use of transitory implants to keep masticatory function during healing process of definitive implant [19]. Rangel et al., showed that in a group of elderly patient from the same Institution of our study, 100% of patients declared satisfied with transitory implants, become comfortable the use of prothesis during implant osseointegration process until implant loading.
It is important to emphasize that the choice of the type of rehabilitation of the edentulous patient is mainly related to the expectations of the patient and the oral characteristics such as bone availability, occlusal factors and facial aesthetics, besides the general systemic aspects, already discussed, that will influence the number of surgery and quantity of implants installed.
Thus, this retrospective study, including 173 patients over 60 years-old, supports the hypothesis that rehabilitation with osseointegrated implants in elderly patients, despite its agerelated and systemic care features, has a high success rate, enabling total and partial rehabilitation of missing teeth in Brazilian patients. Our results also confirm that elderly patients, even presenting systemic diseases, provided they are controlled and under drug therapy, have predictability in dental implant rehabilitation, allowing oral function recovery, comfort and quality of life. Definitely, old age is not a contraindication for rehabilitation with osseointegrated implants [20].
However, future studies are necessary, evaluating the long-term follow-up of the elderly patients, the possible prosthetic and periimplant complications from rehabilitation with implants, the level of satisfaction after the installation of the prosthesis and the influence of systemic changes in stability of osseointegration.
Conclusion
It was concluded that the success rate after implant placement in elderly patients is high, even with medication use and systemic disease.Acknowledgements
This work was supported by Fluminense Federal University, School of Dentistry, Niterói, RJ, Brazil.Author Contributions
Aristides, José Jorge, Telma and Alexandre conceived the ideas; Marina and Rackel collected the data; Valquiria and Priscila analyzed the data; and all the authors led the writing. All the authors approved the submission.Conflict of Interest Statement
None of the authors have a conflict of interest to disclose.Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.Ethics Statement
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The present study was approved by the Research Ethics Committee of the Faculty of Medicine of the Universidade Federal Fluminense, under the number 2.631.531.Ethics Statement
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The present study was approved by the Research Ethics Committee of the Faculty of Medicine of the Universidade Federal Fluminense, under the number 2.631.531.Informed Consent
Informed consent was obtained from all individual participants included in the study.References
- Brazil. Synopsis of the 2010 demographic census. Brazilian Institute of Geography and Statistics (IBGE), Rio de Janeiro, 2011.
- WHO. Ageing and health. World Health Organisation. 2022.
- Grant BT, Kraut RA. Dental implants in geriatric patients: A retrospective study of 47 cases. Implant Dent. 2007;16(4):362-368.
[Crossref] [Google Scholar] [PubMed]
- Branemark PI. Osseointegrated implants in the treatment of the edentulous jaw: Experience from a 10-year period. Scad J Plast Reconstr Surg. 1977;16:1-132.
[Google Scholar] [PubMed]
- Engfors I, Ortorp A, Jemt T. Fixed implantâ?supported prostheses in elderly patients: A 5â?year retrospective study of 133 edentulous patients older than 79 years. Clin Implant Dent Relat Res. 2004;6(4):190-198.
[Crossref] [Google Scholar] [PubMed]
- Tallarico M, Caneva M, Baldini N, Gatti F, Duvina M, Billi M, et al. Patient-centered rehabilitation of single, partial, and complete edentulism with cemented-or screw-retained fixed dental prosthesis: The First Osstem Advanced Dental Implant Research and Education Center Consensus Conference 2017. Eur J Dent. 2018;12(04):617-626.
[Crossref] [Google Scholar] [PubMed]
- Müller F, Naharro M, Carlsson GE. What are the prevalence and incidence of tooth loss in the adult and elderly population in Europe? Clin Oral Implants Res. 2007;18:2-14.
[Crossref] [Google Scholar] [PubMed]
- Lee K, Dam C, Huh J, Park KM, Kim SY, Park W. Distribution of medical status and medications in elderly patients treated with dental implant surgery covered by national healthcare insurance in Korea. J Dent Anesth Pain Med. 2017;17(2):113-119.
[Crossref] [Google Scholar] [PubMed]
- Beil FT, Barvencik F, Gebauer M, Seitz S, Rueger JM, Ignatius A, et al. Effects of estrogen on fracture healing in mice. J Trauma Acute Care Surg. 2010;69(5):1259-1265.
[Crossref] [Google Scholar] [PubMed]
- Tarantino U, Saturnino L, Scialdoni A, Feola M, Liuni FM, Tempesta V, et al. Fracture healing in elderly patients: new challenges for antiosteoporotic drugs. Aging Clin Exp Res. 2013;25:105-108.
[Crossref] [Google Scholar] [PubMed]
- Cummings SR, Kelsey JL, Nevitt MC, O'DOWD KJ. Epidemiology of osteoporosis and osteoporotic fractures. Epidemiol Rev. 1985;7(1):178-208.
[Crossref] [Google Scholar] [PubMed]
- Heersche JN. Bone cells and bone turnover-the basis for pathogenesis. Boca Raton, Florida: CRC Press. 1989:1–17.
- Holmâ?Pedersen P, LOE H. Wound healing in the gingiva of young and old individuals. Euro J Oral Sci. 1971;79(1):40-53.
[Crossref] [Google Scholar] [PubMed]
- Zarb GA, Schmitt A. Osseointegration for elderly patients: the Toronto study. The J Prosthet Dent. 1994;72(5):559-68.
[Crossref] [Google Scholar] [PubMed]
- de Baat C. Success of dental implants in elderly peopleâ?A literature review. Gerodontology. 2000;17(1):45-8.
[Crossref] [Google Scholar] [PubMed]
- Esposito M, Hirsch JM, Lekholm U, Thomsen P. Biological factors contributing. Eur J Oral Sci. 1998;106(1):527-531.
[Crossref] [Google Scholar] [PubMed]
- El Askary AS, Meffert RM, Griffin T. Why do dental implants fail? Part II. Implant Dent. 1999;8(3):265-278.
[Crossref] [Google Scholar] [PubMed]
- Galagali G, Reddy ES, Nidawani P, Behera SS, Preetham P, Sarpangala M. Implant failures: A comprehensive review. IJ Pre Clin Dent Res. 2014;1(1):11-17.
- Morais JA, Heydecke G, Pawliuk J, Lund JP, Feine JS. The effects of mandibular two-implant overdentures on nutrition in elderly edentulous individuals. J Dent Res. 2003;82(1):53-58.
[Crossref] [Google Scholar] [PubMed]
- Berretin-Felix G, Machado WM, Genaro KF. Effects of mandibular fixed implant-supported prostheses on masticatory and swallowing functions in completely edentulous elderly individuals. Int J Oral Maxillofac Implants. 2009;24(1):110-117.
[Google Scholar] [PubMed]
Citation: Pinheiro AR, Pinheiro M, Quinelato V, Gonçalves R, Schoichet JJ, Montenegro AC, et al. (2025) Evaluation of the Early Implant Loss in Elderly Patients: A 10-years Retrospective Study. J Dentistry. 15:726.
Copyright: © 2025 Pinheiro AR, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.