Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- Google Scholar
- SHERPA ROMEO
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2025) Volume 13, Issue 5
Epidemiology of Venous Thromboembolic Disease at the National Reference Teaching Hospital, N'Djamena, Chad
Naibé Dangwe Temoua1,2, Doune Narcisse3*, Zakaria Abdelmadjid Zacharia1,4, Houba Dallah Tchimby Urbain1, Adjougoulta Koboy Allah Amine1, Allawaye Lucien1,2, Adam Ali Ahmat2,3, Taday Moussa2,5, Médila Moussa Ali2,5, Mahamat-Azaki Oumar1, Binwe Dikoua1, Langtar Mianrho Hiby1,3, Djimadoum Nahodjide1, Bamouni Joel6,7 and Zabsonré Patrice6,72Department of Cardiology, Renaissance University Hospital Center, N’Djamena, Chad
3Department of Cardiology, Renaissance University Hospital Center, N’Djamena, Chad
4Department of Health Sciences, Adam Barka University, Abéché, Chad
5Department of Imaging and Radiology, National Reference Teaching Hospital, N’Djamena, Chad
6Department of Cardiology, Teaching Hospital of Yalgado Ouedraogo, Ouagadougou, Burkina Faso
7Department of Training and Research Unit of Health Sciences, University Joseph Ki-Zerbo, Ouagadougou, Burkina Faso
Received: 08-Apr-2024, Manuscript No. JVMS-24-25435; Editor assigned: 11-Apr-2024, Pre QC No. JVMS-24-25435 (PQ); Reviewed: 25-Apr-2024, QC No. JVMS-24-25435; Revised: 10-Oct-2025, Manuscript No. JVMS-24-25435 (R); Published: 17-Oct-2025, DOI: 10.35248/2329-6925.25.13.597
Abstract
Introduction: Venous thromboembolic disease is a clinical entity that includes deep vein thrombosis and its complication, pulmonary embolism that can lead to an immediate death. Its prevalence in hospitals has evolved over time, especially with improved diagnostic methods, ranging from 1.6% to 15% according to sub-Saharan series. The aim of this study was to describe the epidemiological, clinical and evolutionary profile of at the National Reference Teaching Hospital, N’Djamena and Chad.
Materials and methods: This was a prospective, monocentric cohort study conducted in cardiology department of the National Reference Teaching Hospital. It was spread over a period of three (03) years, from January 1st, 2021 to December 31, 2023. All patients hospitalized and/or followed as outpatient for an acute episode of venous thromboembolic disease in the said department were systematically collected in this registry. Diagnoses were confirmed by venous Doppler ultrasound and pulmonary angiography. The variables studied were sociodemographic, clinical, paraclinical and therapeutic characteristics.
Results: 1,754 patients were hospitalized, including 90 with venous thromboembolic disease, representing a hospital prevalence of 5.1%. The mean age was 48.6 ± 14.4 years, with females predominating (52.2%; n=47). For the majority of patients (92.4%; n=84), this was a first inaugural episode of venous thromboembolic disease. The thrombotic risk factors found were: Prolonged bed rest/long journey, obesity and trauma with 45.6%, 31.6% and 22.8% respectively. Pulmonary embolism symptoms were dominated by dyspnea 95.7% (n=22), chest pain 87% (n=20), dry cough 43.5% (n=10), hemoptysis 21.7% (n=5) and syncope 13% (n=3). Signs associated with thrombophlebitis were mainly swelling of the limb in 93.5% of cases (n=72), pain of the limb 92.2% (n=71) and warmth of the limb 77.9% (n=60). Treatment in all cases involved curative dose low molecular weight heparin, followed by oral anticoagulants. The outcome was favorable in 86.7% (n=78) and patient mortality was 11.1% (n=10).
Conclusion: Venous thromboembolic disease is a multifactorial, frequent and potentially serious disease, which is increasingly diagnosed in our context with the improvement of the therapeutic platform. Prevention remains the most effective weapon in the management strategy.
Keywords
Venous thromboembolic disease; N'Djamena; Chad
Introduction
Venous Thromboembolism (VTE) is a clinical entity that groups together deep vein thrombosis and its complication, pulmonary embolism which can lead to an immediate death. Once considered a rare disease in Sub-Saharan Africa, it is becoming increasingly frequent and now constitutes a real public health problem. It's prevalence in hospitals has evolved with time and above all, with improvements in diagnostic methods, ranging from 1.6% to 15% according to Sub-Saharan series. VTE risk factors can be divided into acquired and constitutional. The mechanism common to this entity is explained by the VIRCHOW triad. In our working context, the most frequently encountered risk factors are acquired. These include surgery, prolonged bed rest, pregnancy, childbirth and long journeys. The risk of VTE in the tropics is increased in certain specific conditions, notably HIV. In France, the annual incidence of VTE was 183/100,000 people (124/100,000 for VT and 60/100,000 for PE).The incidence of VTE increased with age, irrespective of gender, reaching 1% in people aged over 75. While venous thrombosis is easy to diagnose, this is not the case for pulmonary embolism, for which the gold standard is pulmonary angiography, which is difficult to access in our working conditions. The management of VTE is also a challenge for physicians. In Chad, few studies have focused on the common entity that is VTE. The aim of this study was to describe the epidemiological, clinical and evolutionary profile of VTE at the National Reference Teaching Hospital, N’Djamena and Chad [1-5].
Materials and Methods
Type and period of study
This was a prospective, monocentric cohort study carried out in the cardiology department of the national reference teaching hospital. It was spread over a period of three (03) years, from January 1, 2021 to December 31, 2023 [6].
Study population
All patients hospitalized and/or followed as outpatients for an acute episode of VTE in the said department were systematically collected in this register. The diagnosis of Deep Vein Thrombosis (DVT) and/or Pulmonary Embolism (PE) was made using a decision tree based on international VTE guidelines. The diagnosis of VTE was based on a personal history of VTE, but above all on ultrasound (for DVT) and/or pulmonary angiography (for PE) diagnostic criteria. Patients with superficial vein thrombosis, with venous thrombosis of unusual locations (mesenteric vein thrombosis, cerebral vein thrombosis and central retinal vein thrombosis) and those with incomplete and/or usable medical records were not included in the study [7-10].
Study variables and data collection techniques
The variables studied were sociodemographic characteristics (age, sex, residence, education level, health coverage and monthly income), clinical data (thromboembolic risk factors, cardiovascular risk factors, symptoms) and paraclinical data (topography of DVT and/or PE) on patient admission. The various medical therapies and progress data were also recorded. These data for each patient were recorded on a previously prepared data collection sheet. These forms were completed by the physicians. The data were extracted from the VTE register available in the cardiology department of the national reference teaching hospital [11].
Data analysis
Data analysis was performed using Epi Info software version 7.1. Quantitative parameters were presented as mean ± standard deviation and qualitative parameters as percentages. Pearson's Chi2 test was used to compare proportions. When application conditions were not observed, Fisher's exact test was used. The student's T-test was used to compare two means. The threshold of statistical significance was p<0.05 [12].
Ethical considerations
The study was conducted in accordance with the declaration of Helsinki. Informed consent was obtained from patients prior to inclusion in the study. Participation in the study offered no direct benefit to the patient and did not expose him/her to any additional risk other than those associated with his/her care [13].
Results
During the study period, 1,754 patients were hospitalized, including 90 with VTE, representing a hospital prevalence of 5.1%. They were divided into 13 cases (14.4%) of PE, 67 cases (74.4%) of DVT and 10 cases (11.1%) of combined PE and DVT.
Socio-demographic characteristics
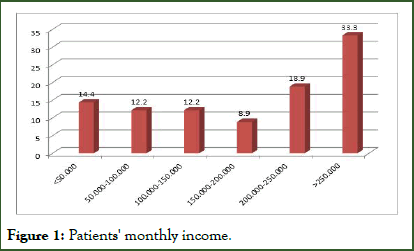
The mean age of our patients was 48.6 ± 14.4 years (20; 81 years). Females predominated with 52.2% (n=47) and the sex ratio was 0.9. In 78.9% of cases, patients came from urban areas, semi-urban areas (13.3%) and rural areas (7.8%). Patients had a higher level of education in 37.8% of cases (n=34) and no schooling in 32.2% of cases (n=29). Table I summarizes the sociodemographic characteristics of our patients. Eighteen patients (20%) had health coverage. Patients with a monthly income of over 250,000 FCFA accounted for 33.3% (n=30) of cases (Figure 1). The minimum wage in Chad is 60,000 FCFA [14].
Figure 1: Patients' monthly income.
| Parameters | Means ± standard deviation | Numbers (%) |
| Age (year) | 31.2 ± 14.4 | |
| Gender | ||
| Male | 43 (47.8) | |
| Female | 47 (52.2) | |
| Residence | ||
| Urban | 71 (78.9) | |
| Semi-urban | 12 (13.3) | |
| Rural | 07 (7.8) | |
| Education level | ||
| No schooling | 29 (32.2) | |
| Primary | 09 (10.0) | |
| Secondary | 18 (20.0) | |
| Higher | 34 (37.8) | |
| Health coverage | ||
| Yes | 18 (20.0) | |
| No | 72 (80.0) | |
Table 1: Socio-demographic characteristics.
Clinical characteristics
For the majority of patients (92.4%; n=84), this was a first inaugural episode of VTE. At least one thrombotic risk factor was found in 79 patients (87.8%). Prolonged bed rest, obesity and trauma were the most common thromboembolic risk factors, with 45.6%, 31.6% and 22.8% respectively (Table 2). At least one cardiovascular risk factor was present in 59 patients (65.5%). These cardiovascular risk factors were dominated by age above 55 years in men and 65 years in women (59.3%), hypertension (52.5%), abdominal obesity (28.8%), diabetes (22%), dyslipidemia (18.6%) and alcohol (10.2%). At least one comorbidity was noted in 34 patients (37.8%), mainly represented by anemia (51.6%), chronic renal failure (32.3%) and stroke (12.9%). Symptoms of PE were dominated by dyspnea 95.7% (n=22), chest pain 87% (n=20), dry cough 43.5% (n=10), hemoptysis 21.7% (n=5) and syncope 13% (n=3). DVT-related signs were mainly swelling of the limb in 93.5% of cases (n=72), limb pain 92.2% (n=71) and limb warmth 77.9% (n=60). Homans' sign was present in 89.6% of DVT patients (n=69). Topographically, PE was segmental in 82.6% of cases (n=19), subsegmental in 39.1% (n=9), truncal in 39.1% (n=9) and lobar in 13% (n=3). Distal vein thrombosis was found in 71.4% of cases (n=55) and proximal vein thrombosis in 68.8% (n=53). In all cases, treatment consisted of curative dose lowmolecular- weight heparin, followed by oral anticoagulants. Twenty-four patients (26.7%) had received direct oral anticoagulant therapy (factor Xa inhibitor) and in 66 patients (73.3%) anticoagulant therapy consisted of anti-vitamin K. The anti-vitamin K used were fluindione in 69.7% (n=46), acenocoumarol 25.8% (n=17) and warfarin 4.5% (n=3). No antifibrinolytic therapy was used in our study even though it was indicated in three patients with severe PE. Progression was favorable in 86.7% (n=78) of cases, with treatment completed. We recorded 2.2% (n=2) discharges against medical advice and patient mortality was 11.1% (n=10) [15].
| Thrombotic risk factors | Frequency (n) | Percentage (%) |
| Prolonged bed rest/long journeys | 36 | 45.6 |
| Obesity | 25 | 31.6 |
| Trauma | 18 | 22.8 |
| Age>65 | 12 | 15.2 |
| Heart failure | 12 | 15.2 |
| Erysipelas | 10 | 13.9 |
| HIV infection | 9 | 11.4 |
| VTE history | 6 | 7.6 |
| Neoplasia | 4 | 5.1 |
| Estrogen-progestin therapy | 4 | 5.1 |
| Venous insufficiency | 3 | 3.8 |
| Peripartum | 3 | 3.8 |
| Smoking | 2 | 2.5 |
Table 2: Thromboembolic risk factors.
Discussion
This prospective cohort has enabled us to describe the epidemiology of VTE in our department. Although the VTE registry has only recently been set up (three years), we have obtained results that we can compare with other studies and with data in the literature [16].
Hospital prevalence of VTE was 5.1%, well below the 12.1% found by Adam, et al., in a study carried out at the Renaissance teaching hospital. This difference in prevalence observed in the two hospital of the same city may be due to the better accessibility and level of technical facilities for VTE diagnosis offered by the Renaissance teaching hospital. This prevalence is also lower than in other African series, notably in Burkina Faso (14.9%) and Benin (10.2%). On the other hand, our prevalence is close to those found by Pessinaba, et al., in Togo (3.1%) and Konin, et al., in Côte d'Ivoire (3.1%). The prevalence of this condition in our developing countries is probably underestimated due to difficulties in accessing diagnostic facilities. Inadequate knowledge of VTE diagnosis among healthcare professionals is also a major contributory factor [17].
The mean age of our patients was 48.6 ± 14.4 years. This corroborates data from African literature, where VTE affects relatively young patients. This contrasts with findings in the West, where the mean age is much higher, 68 years in Germany with an increasing incidence with age. The sociodemographic characteristics of our patients differed little from those described by other African authors. VTE patients were young, predominantly female, with low levels of education, low socioeconomic status and no health coverage. The lack of health coverage and low monthly income of the patients constituted a limitation to their quality of care [18].
Thrombotic risk factors were found in 87.8% of patients. Prolonged bed rest, obesity and trauma were the most common thromboembolic risk factors, with 45.6%, 31.6% and 22.8% respectively. These thrombotic risk factors were also found in African series. These results confirm the importance of induced venous thrombosis in our context, but also the role of prolonged bed rest, long journeys, trauma, surgery and peripartum in the etiopathogenesis of VTE in sub-Saharan Africa. These are preventable causes if adequate thromboprophylaxis had been initiated. Naibe et al. had demonstrated that the knowledge, attitudes and practices of healthcare professionals regarding VTE prophylaxis in our context were fragmented and insufficient to guarantee optimal patient management. Neoplasia was found to be the etiological factor in 5.1% of VTE cases, in line with data from the African literature. This is in contrast to Western data, where neoplasia and hospitalization dominate the etiological factors of VTE. The low prevalence of neoplasia in our series does not reflect reality and reflects the difficulties of diagnosing neoplasia at an early stage, due to patients' financial difficulties on the one hand and the weakness of therapeutic facilities on the other.
Symptoms of PE were dominated by dyspnea (95.7%), basithoracic pain (87%), dry cough (43.5%), hemoptysis (21.7%) and syncope (13%). Limb swelling (93.5%), limb pain (92.2%), Homans’ sign (89.6%) and limb warmth (77.9%) dominated DVT signs. This is also in line with the findings of Ali et al. These signs indicate an advanced stage of VTE at the time of diagnosis. Due to socio cultural as well as financial considerations, most patients turn first to traditional therapists and only consult health care facilities at a later stage.
In terms of management, the therapeutic arsenal remained conventional, with curative doses of low molecular weight heparins followed by an anti-vitamin K or direct oral anticoagulant. Direct oral anticoagulant were used in 26.7% of patients and 73.3% patient with VTE were on anti-vitamin K. Access to direct oral anticoagulant is still limited in our context, given the advantages and convenience of their use. Decision makers should be urged to make direct oral anticoagulant accessible to as many VTE patients as possible. This would guarantee effective and safe care for patients suffering from this condition [19].
The clinical course of VTE was favorable in 86.7% of cases. We recorded a mortality rate of 11.1%. A similarly high mortality rate (27.5%) was also reported by Ndongo, et al., in their series on VTE in Yaoundé. These mortality rates contrast with the low rates seen in developed countries. This can be explained by better access to care in developed countries and, above all, an adequate technical platform [20].
Conclusion
VTE is a frequent and potentially serious multifactorial disease, which is increasingly diagnosed in our context with the improvement of the therapeutic platform. They affect young adults, mostly women, with low socioeconomic status and are more often linked to provoked risk factors. In our country, VTE poses a management problem due to the high cost of complementary examinations and anticoagulant treatment. Prevention remains the most effective weapon in the management strategy.
References
- Olié V, Chin F, Lamarche-Vadel A, De Peretti C. La maladie veineuse thromboembolique: Patients hospitalisés et mortalité en France en 2010. Bull Epidémiol Hebd. 2013;33:417-424.
- Venous thromboembolic disease in Cameroon: About 18 cases. Trop Med. 2002;62:47-50.
- Dénakpo J, Zouménou E, Kérékou A, dossou F, hounton N, sambiéni O. Fréquence et facteurs de risque de la maladie thromboembolique veineuse chez la femme en milieu hospitalier a Cotonou, Benin. Ashdin Publ Clin Mother Child health. 2012;9:5.
- Ali AA, Doune N, Youssouf MY, Bahar AM. Aspects épidémiologiques, cliniques, thérapeutiques et évolutifs de l’embolie pulmonaire au CHU la Renaissance de N’Djamena (Tchad)â?¯: Etude rétrospective. Ann Afr Med. 2021;14(4):e4340-e4346.
- Ello FN, Bawe A, Kouakou GA, Mossou CM, Adama D, Kassi AN, et al. Manifestations thromboemboliques chez 36 patients ouest africains infectés par le VIH. Pan Afr Med J. 2018; 31:224.
- Oger E. Incidence of venous thromboembolism: a community-based study in Western France. EPI-GETBP Study Group. Groupe d’Étude de la Thrombose de Bretagne Occidentale. Thromb Haemost. 2000;83(5):657-660.
- Pessinaba S, Molba YD, Baragou S, Pio M, Afassinou Y, Kpélafia M, et al. Pulmonary embolism at the Lomé University Hospital Campus (Togo): retrospective study of 51 cases. Pan African Med J. 2017;27:129.
- Konin C, Adoh M, Kramoh E, Aevouelie-Kouassi F, Anzouan-Kacou B, N’guetta R, et al. Deep vein thrombosis of the lower limbs in tropical environments: epidemiological aspects and etiological factors. Black Afr Med. 2004;51:469-473.
- Owono Etoundi P, Esiene, Bengono Bengono A, Amengle L, Afane Ela A, Minkande J. Venous thromboembolic disease. Epidemiological aspects and risk factors in a Cameroonian hospital. Health Sci Dis. 2015;16(4):2015.
- Diall IB, Coulibaly S, Minta I, Ba Ho, Diakite M, Sidibe N, et al. Etiology, clinical presentation and development of pulmonary embolism in 30 cases. Mali Méd. 2011;26:1-6.
- Reissig A, Haase U, Schulze E, Lehmann T, Kroegel C. Diagnosis and therapy of pulmonary embolism prior to death. Dtsch Med Wochenschr. 2010;135:1477-1483.
- Mahe I, Caulin C, Bergmann JF. Age, an independent risk factor for thrombosis: Epidemiological data. Med Press. 2005;34(12):878-886.
- Pottier P, Planchon B, Pistorius MA, Grolleau JY. Risk factors and incidence of venous thromboembolic disease in internal medicine: A prospective descriptive study of 947 hospitalized patients. J Int Med. 2001;4:348-359.
- Ondze-Kafata LI, Kouala Landa C, Traore- Kissima A, Loumouamou M, Bani M, Amounya- Zobo S, et al. Venous thrombosis of the lower limbs in Brazzaville: A report of 44 cases. Cardiol Tropicale. 2012;135.
- Delluc A, Le Ven F, Mottier D, Le Gal G. Epidemiology and risk factors of venous thromboembolic disease. Review of Malad Respi. 2012;29(2):254-266.
- Kamdem F, Ngahane BHM, Hamadou B, Mongyui A, Doualla MS, Jingi AM, et al. Epidemiology, clinical presentations and in hospital mortality of venous thromboembolism at the douala general hospital: A cross-sectional study in cameroon, sub-saharan Africa. World J Cardiovasc Dis. 2018;8:123-132.
- Prandoni P. Deep vein thrombosis and hidden cancers. Blood Thrombosis Vessels. 1994;6:643-645.
- Meyer G. Venous thromboembolism and cancer. Clin Pulmonol Rev. 2014;70:91-94.
- Konstantinides SV, Torbicki A, Agnella G, Danchin N, Fitzmaurice D, Galie N, et al. 2014 ESC Guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014;35:3033–3069.
- Hoffmann B, Gross CR, Jockel KH, Kroger K. Trends in mortality of pulmonary embolism: An international comparison. Thromb Res. 2010;125:303-308.
Citation: Temoua ND, Narcisse D, Zacharia ZA, Urbain HDT, Amine AKA, Lucien A, et al. (2025) Epidemiology of Venous Thromboembolic disease at the National Reference Teaching Hospital, Nâ??Djamena, Chad. J Coast Zone Manag. 13:597.
Copyright: © 2025 Temoua ND, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.