Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
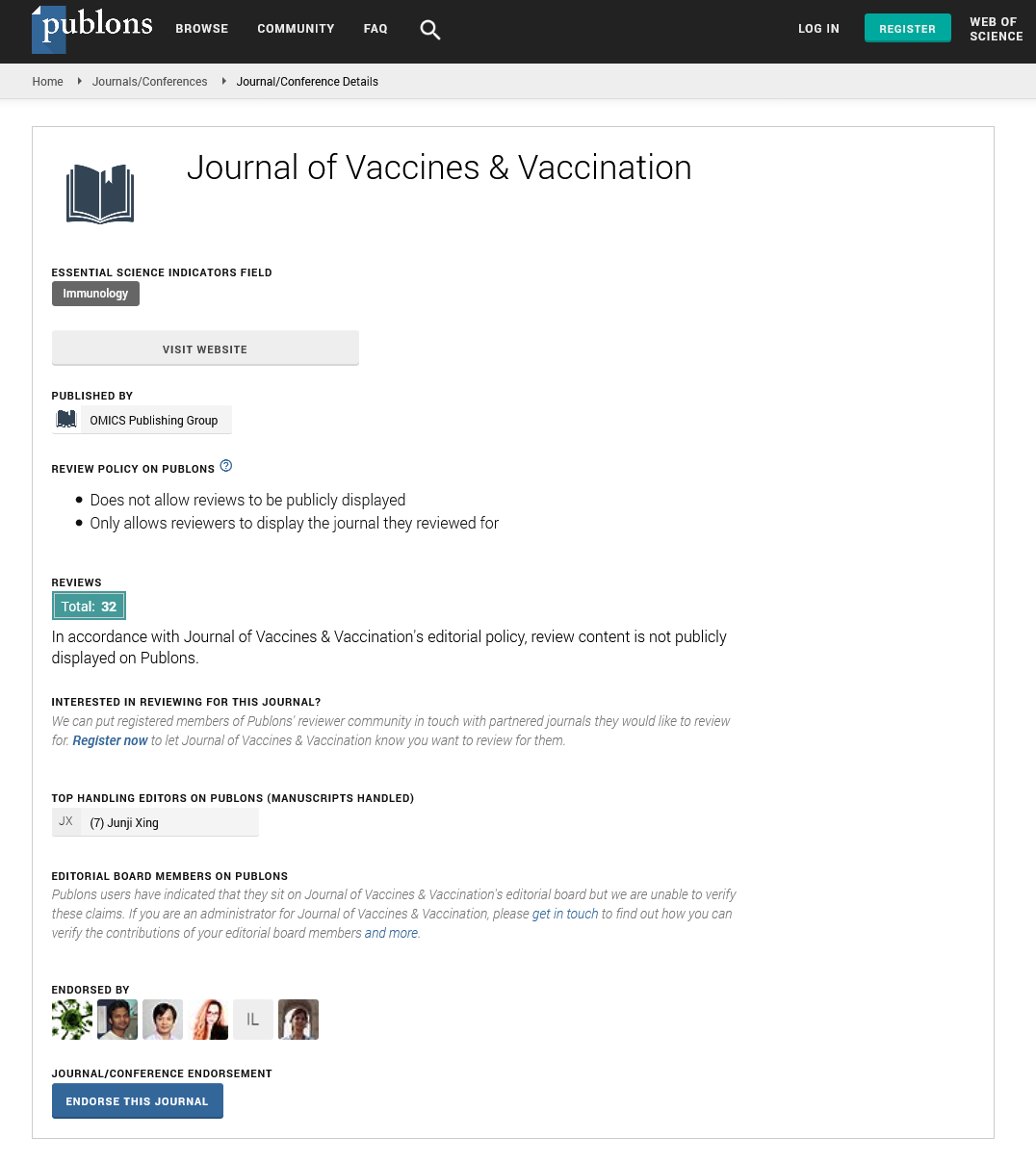
- Publons
- MIAR
- University Grants Commission
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Short Communication - (2022) Volume 13, Issue 1
Does Educating and Debunking Myths Concerning the Influenza Vaccine Improve Vaccination Rates in HIV Patients at the Medical College of Georgia?
Siddiqui B*Received: 11-Jan-2022, Manuscript No. JVV-22-15441; Editor assigned: 13-Jan-2022, Pre QC No. JVV-22-15441 (PQ); Reviewed: 27-Jan-2022, QC No. JVV-22-15441; Revised: 03-Feb-2022, Manuscript No. JVV-22-15441 (R); Published: 10-Feb-2022, DOI: 10.35248/2155-9627.22.13.472
Abstract
Introduction:Influenza-related symptoms and mortality rate are worse in AIDS patients. Studies have shown that educating patients about the safety and efficacy of the influenza vaccine have improved patient vaccine acceptance rates.
Methods: An anonymous two-question survey was distributed to HIV patients who refused the influenza vaccine at the MCG clinic. The questions included why they refused the vaccine and whether they changed their minds after reading about the safety and benefits of the vaccine.
Results: 26 of 38 patients replied to the survey. Only 12 of the 26 patients changed their minds and were agreeable to receiving the influenza vaccine after being educated.
Conclusion: Vaccine acceptance amongst HIV patients at MCG remains low after educating them and debunking myths.
Keywords
Influenza; HIV infection; Cardiovascular; Microbiome; Probiotics
Introduction
The risk for influenza-related death is estimated to be 9.4 to 14.6 per 10,000 in persons with AIDS, compared with 0.09 to 0.10 per 10,000 among all persons 25 to 54 years of age, and 6.4 to seven per 10,000 among persons 65 years of age and older [1]. Influenza symptoms may be prolonged, and the risk for complications from influenza may be increased. HIV infection may predispose individuals to increased susceptibility to influenza infection, prolonged viral replication and shedding, longer duration of influenza symptomatology and higher influenza-related mortality [2-4]. Influenza was responsible for at least 40% of all febrile respiratory illnesses among an influenza-vaccinated outpatient population of HIV-infected patients over two consecutive influenza seasons. Ninety per cent of these patients were on Antiretroviral Therapy (HAART), with a median CD4 count of 325 cells/μL and an HIV RNA level below 50 copies/mL [5]. Studies have shown that educating patients about the safety and efficacy of influenza vaccination have improved patient vaccine acceptance [6]. This study sought to determine whether educating HIV patients at the Medical College of Georgia (MCG) regarding the influenza vaccine improved vaccine acceptance.
Materials and Methods
HIV patients at the Medical College of Georgia (MCG) who refused the influenza vaccine were invited to participate in a survey. The survey consisted of information regarding the safety and efficacy of the influenza vaccine in HIV patients (see pamphlet below).
1. HIV-infected persons are at greater risk for prolonged hospitalization, severe illnesses including death related to influenza than non-HIV patients [7].
2. In general, HIV patients without AIDS defining illness or near- normal CD4+ T lymphocyte cell counts who receive the Inactivated Influenza Vaccine c develop adequate antibody responses [8].
3. Inactivated influenza vaccine (IIV) administered in HIV-infected adults did not result in potential adverse events [9].
4. In a large study from 1990-2016, there were no adverse reactions or vaccine safety concerns among HIV-positive persons [10].
5. Getting vaccinated may also protect others including those who are more vulnerable to serious flu illness, like babies, children, seniors and people with weaker immune systems.
6. Flu can be caused by many other viruses which we do not have vaccines for.
7. It is better to get the vaccine than to get infected with the flu virus because that would be a risk for hospitalization/death.
8. It is necessary to get the vaccine each year because the immune response declines over time.
9. Serious allergic reactions to flu vaccines are very rare. If they do occur, it is usually within a few minutes to a few hours after the vaccination.
10. It is not too late to get vaccinated, even in January or later.
The survey then inquired whether they changed their mind becoming agreeable to receive the influenza vaccine (Table 1).
| True | False |
|---|---|
| a) I had a misunderstanding about the vaccine side effects | d) I will take my chances |
| b) I had a misunderstanding about the vaccine effectiveness | e) I still do not think influenza is serious |
| c) I want to prevent others from getting sick with the flu | f) I still do not believe the vaccine is effective |
Table 1: Did the influenza pamphlet make me want to take the vaccine? True or false and why?
Results
Only 12 out of 26 (46%) of patients were persuaded by the information and became willing to receive the vaccine. Of the patients who changed their mind becoming agreeable to receive the influenza vaccine, only two said it was due to them having a misunderstanding about the vaccine effectiveness. Six patients had a misunderstanding about the vaccine side effects and four patients wanted to prevent others from getting sick with the flu. Of the 14 patients who did not change their mind still refusing the vaccine, nine said they will take their chances with getting sick with influenza. Four still felt that influenza is not so dangerous and only one was not convinced that the vaccine worked.
Discussion
HIV-infected persons are at greater risk for prolonged hospitalization, severe illnesses including death related to influenza than non-HIV patients [7]. In general, HIV patients without AIDS defining illness or near-normal CD4+ T lymphocyte cell counts who receive the Inactivated Influenza Vaccine (IIV) develop adequate antibody responses [8]. Inactivated influenza vaccine administered in HIVinfected adults did not result in potential adverse events [9]. In a large study from 1990-2016, there were no adverse reactions or vaccine safety concerns among HIV-positive persons [10]. This study is limited as a single-center, small sample size.
Conclusion
This study highlights the need for further efforts to increase influenza vaccine acceptance amongst the HIV population in the MCG. Further efforts to educate and persuade HIV patients to receive the influenza vaccine are needed to prevent the morbidity and mortality associated with influenza.
REFERENCES
- Lin JC, Nichol KL. Excess mortality due to pneumonia or influenza during influenza seasons among persons with acquired immunodeficiency syndrome. Arch Intern Med. 2001; 161(3):441-446.
[Crossref], [Google Scholar], [PubMed]
- Safrin S, Rush JD, Mills J. Influenza in patients with human immunodeficiency virus infection. Chest. 1990; 98(1):33-37.
[Crossref], [Google Scholar], [PubMed]
- Radwan HM, Cheeseman SH, Lai KK, Ellison III RT. Influenza in human immunodeficiency virus-infected patients during the 1997–1998 influenza season. Clin Infect Dis. 2000; 31(2):604-606.
[Crossref], [Google Scholar], [PubMed]
- Fine AD, Bridges CB, De Guzman AM, Glover L, Zeller B, Wong SJ, et al. Influenza A among patients with human immunodeficiency virus: an outbreak of infection at a residential facility in New York City. Clin Infect Dis. 2001; 32(12):1784-1791.
[Crossref], [Google Scholar], [PubMed]
- Klein MB, Lu Y, DelBalso L, Coté S, Boivin G. Influenza virus infection is a primary cause of febrile respiratory illness in HIV-infected adults, despite vaccination. Clin Infect Dis. 2007; 45(2):234-240.
[CrossRef], [Google Scholar], [PubMed]
- Goodman K, Mossad SB, Taksler GB, Emery J, Schramm S, Rothberg MB. Impact of Video Education on Influenza Vaccination in Pregnancy. J Reprod Med. 2015, 60:471-479.
[Google Scholar], [PubMed]
- Cohen C, Moyes J, Tempia S, Groom M, Walaza S, Pretorius M, et al. Severe influenza-associated respiratory infection in high HIV prevalence setting, South Africa, 2009-2011. Emerging infectious diseases. 2013; 19(11):1766.
[Crossref], [Google Scholar], [PubMed]
- Chadwick EG, Chang GO, Decker MD, Yogev R, Dimichele DO, Edwards KM. Serologic response to standard inactivated influenza vaccine in human immunodeficiency virus-infected children. Pediatr Infect Dis J. 1994; 13(3):206-211.
[Crossref], [Google Scholar], [PubMed]
- Hajiabdolbaghi M, Jam S, Seyed Alinaghi S, Jafari S, Badie BM, Sabzvari D. Adverse reactions of trivalent influenza vaccine in HIV-infected individuals. Acta Medica Iranica. 2010:95-100.
[Crossref], [Google Scholar], [PubMed]
- John S, Carmen N, Paige. Adverse events after vaccination among HIV-positive persons, 1990-2016. 2018.
[Crossref], [Google Scholar], [PubMed]
Citation: Siddiqui B (2022) Does Educating and Debunking Myths Concerning the Influenza Vaccine Improve Vaccination Rates in HIV Patients at the Medical College of Georgia? J Vaccines Vaccin. 13:472.
Copyright: © 2022 Siddiqui B. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.