Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- Google Scholar
- SHERPA ROMEO
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2021) Volume 9, Issue 5
Detection of Asymptomatic Peripheral Vascular Disease in Healthy Male Smokers between 21 to 60 years Attending Tertiary Care Hospital using Ankle Brachial Pressure Index in Urban Chennai: An Observational Study
Jayakanthan Saravanan*Received: 23-Aug-2021 Published: 13-Sep-2021, DOI: 10.35248/2329-6925.21.9.424
Abstract
Background: PAD affects 10%-15% of the population and about 20% of people aged over 60 years. Worldwide, the incidence of PAD has increased from 164 million in 2000 to 202 million in 2010. 50% of population who have PVD are asymptomatic and therefore do not seek medical assistance, or are not screened by clinicians in the absence of symptoms. Therefore it becomes necessary to screen the individuals who have asymptomatic PVD at early stage as they have the equal risk of morbidity and mortality like those who have obvious symptoms.
In the 1950's, Winsor described the Ankle Brachial Index (ABI), a good and simple non-invasive method for assessing arterial perfusion. It remains a primary clinical diagnostic test for detection of asymptomatic PAD. The lower the ABPI (Ankle–Brachial Pressure Index) value, the higher the risk of all-cause and cardiac mortality in patients with peripheral vascular disease. The predictive value of ABPI in cardiovascular morbidity and mortality is similar to that of traditional Framingham risk factors. McKenna and colleagues evaluated a low ABPI as an independent risk factor for mortality.
Objective:
• Detect the presence of PVD in 300 healthy smokers using the ABPI index
• To find out the association between the No. of pack years of smoking and the severity of PVD
Methods: In our tertiary institute we conducted a study from April 2021 to June 2021 in which we recorded the ABPI index of healthy male smokers between 20 to 60 years and statistical analysis was done to see if there is a positive correlation between the number of pack years of smoking and the duration of smoking with the occurrence of peripheral vascular disease.
Results: Healthy smokers mean age is 49.61 years and standard deviation is 7.49 years. There is a significant, negative, moderate correlation between healthy smokers Age and ABPI index. It means as age increases their ABPI index score decreases moderately. The relationship between the number of pack years and the severity of PVD showed that as the number of pack years and duration of smoking increased, the severity of PVD also increased.
Conclusion: Asymptomatic smokers also have significant peripheral vascular disease and it is positively correlated to the duration, age and the number of pack years of smoking. So it is very essential to screen the smokers though asymptomatic for the peripheral vascular diseases. This can be done by a very effective non-invasive cost effective Ankle brachial pressure index.
Keywords
Peripheral vascular disease; Ankle–brachial pressure index; Smokers; Pack years; Asymptomatic
Introduction
Peripheral Vascular Disease (PVD), which includes Peripheral Arterial Disease (PAD), Chronic Venous Disease (CVD), Chronic Venous Insufficiency (CVI) and Deep Vein Thrombosis (DVT), are major causes of morbidity worldwide [1,2]. They cause significant financial burden globally. These diseases occur either due to damage, occlusion and/or inflammation of arteries and/or veins [3,4].
Peripheral Arterial Disease (PAD) occurs when there is a deposition of fat or plaque in the vessel. Ultimately it leads to narrowing of the vessel and blockage. The body area that is supplied by the damaged artery undergoes hypoxic changes and ultimately leads to pain, numbness and impaired sensation in the affected segments [3]. PAD also increases the risk of infection in the affected area. If it goes undiagnosed it leads to severe occlusion increasing the risk of gangrene and ultimately amputation. There are studies which show that risk of coronary heart disease and cerebral vascular disease is far higher in population with PAD than in normal population [2,3].
In general, PAD affects 10%-15% of the population and about 20% of people aged over 60 years. Worldwide, the incidence of PAD has increased from 164 million in 2000 to 202 million in 2010 [2,4,5].
Smoking is a very important modifiable risk factor for every atherosclerotic disease especially Peripheral Artery disease. Atleast about 80% to 85% of the population who have PAD have been found to be former or current smokers [6].
50% of population who have PVD are asymptomatic and therefore do not seek medical assistance, or are not screened by clinicians in the absence of symptoms. Therefore it becomes necessary to screen the individuals who have asymptomatic PVD at early stage as they have the equal risk of morbidity and mortality like those who have obvious symptoms. A variety of both invasive and non-invasive diagnostic devices have been developed since the 1670s to facilitate accurate diagnosis and address the prevalence and socioeconomic impacts of PVDs [6-9].
Four primary invasive methods are angiography, venography, ambulatory venous pressure, and intravascular ultrasound. These invasive methods although highly accurate, they are costly, uncomfortable and time consuming. They are mostly reserved for detailed assessment prior to surgical procedures [7,8,10,11].
Moreover these expensive and invasive methods are not feasible for routine screening especially in developing countries like India, but screening the at risk population is crucial for early disease diagnosis when preventive care could have the greatest benefit.
So non-invasive methods are an alternative and can be used more routinely for diagnosis and follow-up of subsequent treatment [6]. Three primary validated non-invasive technologies are plethysmography, Doppler ultrasound and blood pressure methods [7].
Ankle Brachial Index (ABI) in the 1950′s, Winsor described the Ankle Brachial Index (ABI), a good and simple non-invasive method for assessing arterial perfusion. It remains a primary clinical diagnostic test for detection of asymptomatic PAD [11]. The ABI is measured by calculating the blood pressure at the ankle and dividing by the higher of two brachial systolic blood pressures. A normal ABI is between 1 and 1.3, with 0.91-0.99 acceptable. An ABI lower than 0.8 indicates the presence of PAD with ratios below 0.4 indicating the presence of severe PAD and problems for healing. A single ABI measurement may not be sufficient for diagnosis even in symptomatic cases. In such cases, the patient is asked to perform a standardized exercise, after which an ABI is recalculated [6,12,13].
Decreases in post exercise ankle pressure of 20 mmHg or more is indicative of severe PAD. While the ABI is a simple cost effective test, it can be time consuming and requires training and experience.
The lower the ABPI value, the higher the risk of all-cause and cardiac mortality in patients with peripheral vascular disease. The predictive value of ABPI in cardiovascular morbidity and mortality is similar to that of traditional Framingham risk factors. McKenna and colleagues evaluated a low ABPI as an independent risk factor for mortality [7,6,13].
Doobay and Anand found that low ABPI was highly specific for predicting future cardiovascular events. Recent meta-analysis found that low ABPI is an independent risk factor for cardiovascular mortality alongside the traditional Framingham risk factors, and having an ABPI of <0.8 resulted in a doubling of cardiovascular mortality and morbidity across all of the Framingham risk categories; furthermore, combining ABPI with traditional Framingham risk assessment would re-classify 19% of men and 36% of women into more appropriate treatment categories (Table 1) [14-16].
| Resting ABPI | Severity of disease |
|---|---|
| >1.4 | Calcification may be present |
| >1.0 | Probably no arterial disease |
| 0.81–1.00 | No significant arterial disease, or mild/insignificant disease |
| 0.5–0.80 | Moderate disease |
| <0.5 | Severe disease |
| <0.3 | Critical ischemia |
Table 1: Severity of disease.
There are a few disadvantages of ABPI. For example, in elderly, diabetic and renal patients (and also other groups with rarer systemic diseases, like systemic sclerosis, or rheumatic diseases) calcification of the peripheral arteries can make the arteries incompressible, and therefore the test becomes very inaccurate. But the estimated prevalence of PVD is as high as 33% to 59% in these groups. Therefore, for a group of patients with long-standing diabetes, or renal failure, presenting with peripheral vascular symptoms, and in whom ABPI is non-diagnostic, there is a need for a non-invasive, clinical alternative to ABPI for assessing the presence of significant arterial disease.
There are numerous studies available outside India especially in European countries, [12,17] which prove the occurrence of PVD in asymptomatic healthy smokers. But as there are only very few studies available in Indian population, this study is conducted in our Tertiary Institute [6].
Aim and objective
Detection of asymptomatic Peripheral vascular disease in healthy smokers between 20 to 60 years attending tertiary care hospital using ABPI index in urban Chennai.
Objective
• To detect the presence of PVD in healthy smokers using the ABPI index
• To find out the association between the No. of pack years of smoking and the severity of PVD
Materials and Methods
Study design: Observational study.
Study period: April 2021 to June 2021.
Study place: Outpatient department of Sree Balaji Medical College & Hospital, Chromepet, Chennai.
Study population: Healthy Smokers from 20 to 60 years.
Sample size: Prevalence of PVD in general population in India is 3.2% based on the study by Premalatha, et al. Diabetes care, [6].
Based on this prevalence, sample size is calculated by the formula
n=Z2Pq/d2
1.96 × 1.96 × 3.2 × 96.8/262 (P=3.2, q=96.8, z=1.96, d=2 absolute precision)
N=297
Sample size: 300.
Inclusion criteria
Smokers from 20 to 60 years with no other comorbidities.
Exclusion criteria
• Rest pain
• Claudication pain
• Diabetics
• Ulcer
• Immunocompromised status
• Patients diagnosed previously with coronary artery disease
• Patients with features of Multi Organ Dysfunction Syndrome
• Renal disease
• Other systemic vascular diseases like scleroderma
Procedure
Procedure is explained and after a written informed consent it is preceded. Patient is ensured to be lying flat and is comfortable, relaxed and with no pressure on the proximal vessels.
Measurement of the brachial systolic blood pressure
• Place an appropriately sized cuff around the upper arm
• Ensure that the equipment and the arm are at heart level
• Locate the brachial pulse and apply ultrasound contact gel
• Angle the Doppler probe at 45° and move the probe to obtain the best signal
• Inflate the cuff until the signal is abolished then deflate the cuff slowly and record the pressure at which the signal returns being careful not to move the probe from the line of the artery
• Repeat the procedure for the other arm
• Use the highest of the two values as the best non-invasive estimate of central systolic pressure and use this figure to calculate the ABPI
Measurement of the ankle systolic pressure
• Place an appropriately sized cuff around the ankle immediately above the malleoli having first protected any ulcer or fragile skin that may be present
• Examine the foot, locating the dorsalis pedis pulse and apply contact gel
• Continue as for the brachial pressure, recording this pressure in the same way again with equipment at heart level
• Repeat this for the posterior tibial and if required the peroneal and anterior tibial arteries
• Use the highest reading obtained to calculate the ABPI for that leg
• Repeat for the other leg
• Calculate the ABPI for each leg using the formula below or look up the ABPI using a reference chart
ABPI: Ankle systolic blood pressure/Brachial systolic blood pressure
ABPI>1.0 Normal
ABPI<0.92 Indicates arterial disease
ABPI>0.5 and <0.9 can be associated with claudication
ABPI<0.5 indicates severe arterial disease and may be associated with gangrene, ischaemic ulceration or rest pain and warrants urgent referral for a vascular opinion (Figure 1).
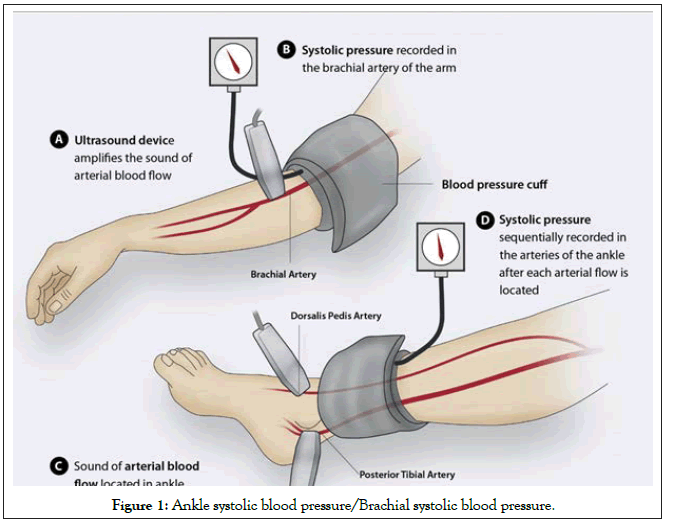
Figure 1: Ankle systolic blood pressure/Brachial systolic blood pressure.
Results
In the sample population of 300, all were males because of ethical concern.
The population were subdivided based on the following criteria and analysed for the ABPI
• Age wise distribution
• ABPI in different age groups
No. of pack years smoked and its relationship with the grade of PVD in different age groups.
Statistical analysis
Demographic variables in categorical/dichotomous were given in frequencies with their percentages. Age and ABPI index score were given in mean and standard deviation. Association between age and pack years was calculated using chi square test. Association between age and ABPI index level was calculated using chi square test. Difference of <1 pack year and >1 pack year of ABPI score was analyzed using student independent t-test. Correlation between Age and ABPI index score were analyzed using Karl Pearson correlation coefficient method.
Simple bar diagram, Multiple bar diagram, simple bar with 2 standard Error bar, and Scatter diagram with regression estimate were used to represent the data. A p-value of ≤ 0.05 was considered statistically significant, and two-tailed tests were used for testing significance. Statistical analysis was carried out using the Statistical Package for Social Sciences (SPSS, version 16) and STATA (version 10) and Epi info (Version 3.5.1) statistical software’s.
Discussion
Healthy smokers mean age is 49.61 years and standard deviation is 7.49 years
In our study, a total of 300 smokers who did not have any comorbidity were divided into 4 age groups. 20 to 30 years, 31 to 40 years, 41 to 50 years and 51 to 60 years (Table 2) (Figures 2 and 3).
| Age | No of patients | Percentage |
|---|---|---|
| 20-30 years | 4 | 1.33% |
| 31-40 years | 19 | 6.33% |
| 41-50 years | 121 | 40.34% |
| 51- 60 years | 156 | 52.00% |
| Total | 300 | 100.00% |
Table 2: Distribution of various age groups.
Only men were taken as sample population due to ethical reasons.
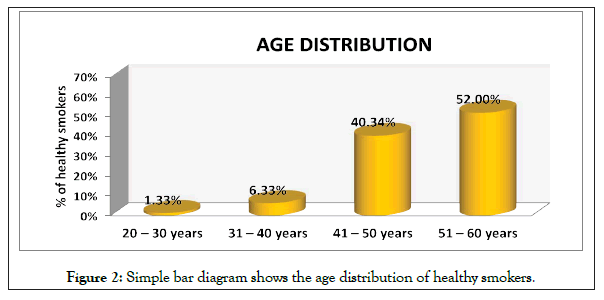
Figure 2: Simple bar diagram shows the age distribution of healthy smokers.
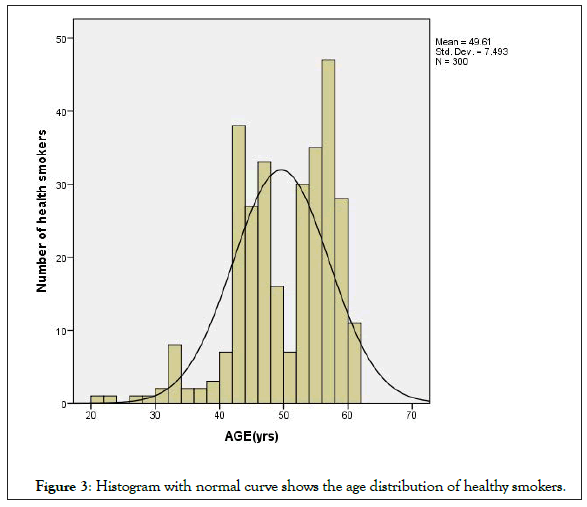
Figure 3: Histogram with normal curve shows the age distribution of healthy smokers.
Healthy smokers were found to be having a mean age of 49.61 years with a standard deviation of 7.49 years (Table 3 and Figure 4).
| Age | >1 | 0.8 to 1 | 0.5 to 0.8 | <0.5 | Total |
|---|---|---|---|---|---|
| 20-30 | 4 (100%) | 0 | 0 | 0 | 4 |
| 31-40 | 17 (89.47%) | 2 (10.53%) | 0 | 0 | 19 |
| 41-50 | 20 (16.53%) | 97 (80.17%) | 4 (3.30%) | 0 | 121 |
| 51-60 | 6 (3.84%) | 99 (63.46%) | 48 (30.77%) | 3 (1.93%) | 156 |
Table 3: ABPI in the above age groups.
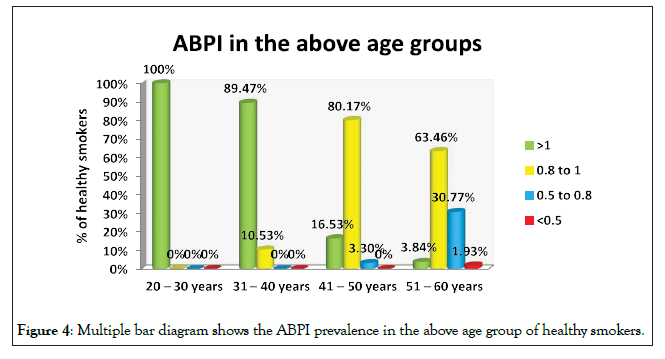
Figure 4: Multiple bar diagram shows the ABPI prevalence in the above age group of healthy smokers.
χ2=142.20 p ≤ 0.001 very high significant
0.0-0.2 poor correlation
0.2-0.4 fair correlation
0.4-0.6 moderate correlation
0.6-0.8 substantial correlation
0.8-1.0 strong correlation
In the study we correlated the relationship between the ages of the healthy smokers with the ABPI index. From the Table 4, we can see that applying the Karl Pearson correlation coefficients, it is evident that there is a significant, negative, moderate correlation between the age of healthy and ABPI index. It means as age increases their ABPI index score decreases moderately (Figure 5).
| Correlation between | Mean score | Karl pearson Correlation coefficients | Interpretation |
|---|---|---|---|
| Mean ± SD | |||
| Age vs ABPI index score | 49.61 ± 7.49 | r= -0.54 P=0.001*** | There is a significant, negative, moderate correlation between healthy smokers Age and ABPI index. It means as age increases their ABPI index score decreases moderately |
| 0.94 ± 0.23 |
Table 4: Correlation between healthy smokers Age and ABPI index.
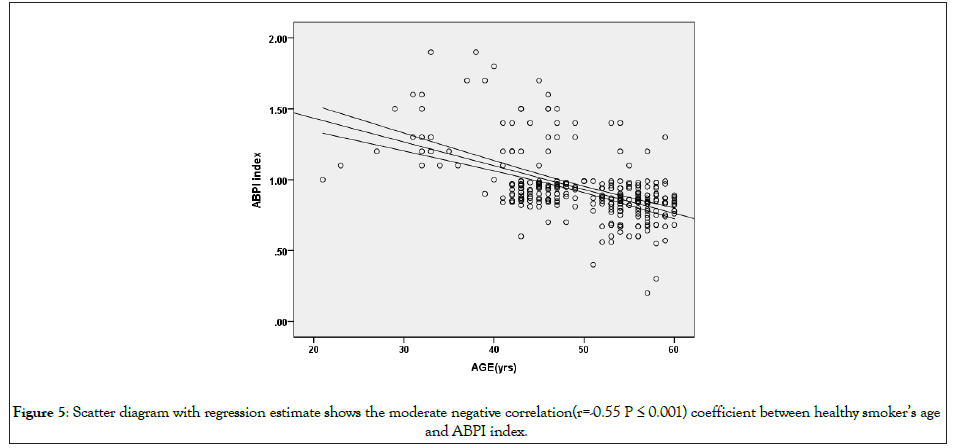
Figure 5: Scatter diagram with regression estimate shows the moderate negative correlation(r=-0.55 P ≤ 0.001) coefficient between healthy smoker’s age and ABPI index.
This is in accordance with the study done by Premalatha, et al. in Kerala which showed PVD was uncommon until middle-age and then the prevalence rate increased dramatically. Univariate regression analysis showed at age >50 years odds ratio (OR) was 6.3, 95% CI 2.1-20.6, P<0.001 [6].
The entire study population was categorised by calculating the pack years meticulously, into two groups as less than one pack year and more than one pack year <1 pack years are having 1.12 ABPI index score and >1 pack years are having 0.87 ABPI index score. Difference is 0.25 score, this difference is large and it is statistically significant, it was confirmed using student independent t-test.
From the Table 5, which shows the pack year and ABPI, it is seen that smokers having <1 pack years are having 1.12 ABPI index score and >1 pack years are having 0.87 ABPI index score. Difference is 0.25 index score, this difference is large and it is statistically significant, it was confirmed using student independent t-test (Figure 6).
| No. of pack years | >1 | 0.9 to 1 | 0.5 to 0.9 | <0.5 |
|---|---|---|---|---|
| <1 | 4 | 0 | 0 | 0 |
| >1 | 0 | 0 | 0 | 0 |
Table 5: Pack year and ABPI index.
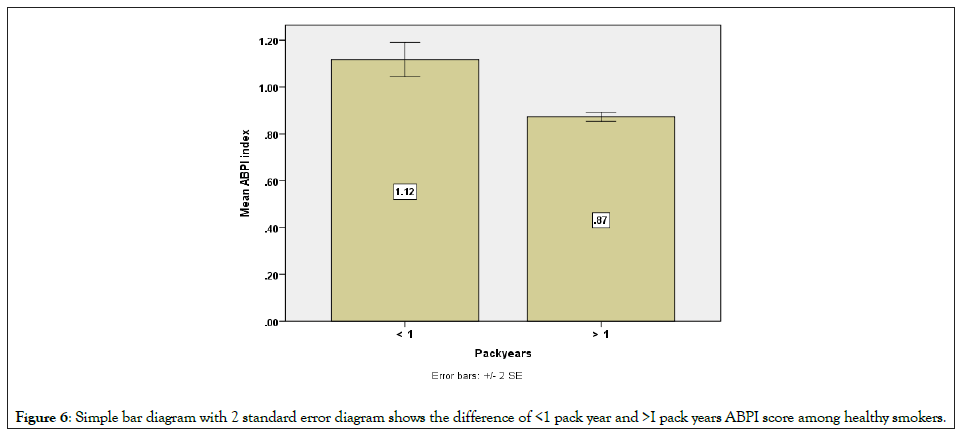
Figure 6: Simple bar diagram with 2 standard error diagram shows the difference of <1 pack year and >I pack years ABPI score among healthy smokers.
This is in accordance with the study by Ingolfsson, et al. which showed the smokers who smoked more cigarettes had higher risk of PVD (1-14 cigarettes/day RR, 2.6 p=.001, 15-24 cigarettes/day RR, 7.7 p=.001, 25 cigarettes/day RR, 10.2 p=.01 Pipe or cigars RR, 3.6 p=.001) (Table 6) [10].
| Packyears | N | Mean | SD | Student independent t-test | |
|---|---|---|---|---|---|
| ABPI | < 1 | 79 | 1.12 | 0.33 | t=6.45 p ≤ 0.001 |
| > 1 | 221 | 0.87 | 0.15 |
Table 6: No. of packyears and ABPI in 20 to 30 year age group.
In the younger age population (age 20 to 30 years), all the four had <one pack year and ABPI was normal (Table 7).
| No. of pack years | >1 | 0.9 to 1 | 0.5 to 0.9 | <0.5 |
|---|---|---|---|---|
| <1 | 16 | 0 | 0 | 0 |
| >1 | 1 | 2 | 0 | 0 |
Table 7: No. of pack years and ABPI in 31 to 40 year age group.S
Yates corrected χ2=5.89 p ≤ 0.02 significant
Less than 1 pack years are having more ABPI index score.
More than 1 pack years are having less ABPI index score.
As the age advances and as the number of pack years increases, the risk of moderate to severe PAD increases. This is well shown in the systematic review published by Willigendael, et al. in Journal of vascular surgery [18].
Our study also shows in age group of 31 to 40 years, Less than 1 pack years are having more ABPI index,more than 1 pack years are having less ABPI index score, Yates corrected χ2=5.89 p ≤ 0.02 significant (Table 8).
| No. of pack years | >1 | 0.9 to 1 | 0.5 to 0.9 | <0.5 |
|---|---|---|---|---|
| <1 | 16 | 23 | 1 | 0 |
| >1 | 4 | 74 | 3 | 0 |
Table 8: No. of pack years and ABPI in 41 to 50 year age group.
χ2=23.86 p ≤ 0.01 highly significant
In the age group of 41 to 50 years it is again seen that those smokers with less than 1 pack years are having more ABPI index score, more than 1 pack years are having less ABPI index score.
This fact is shown in many studies done outside India like Clark, et al. smokers had increased risk of ankle-brachial index <1 (odds ratio, 2.2, 95% CI, 1.5-3.3) [17].
He, et al. the odds ratios and 95% confidence intervals of PAD for current smokers vs. never smokers were 1.54 (1.12 to 2.11) and 1.28 (0.91 to 1.79) for former smokers (stopped smoking for at least 2 years) (Table 9) [19].
| No. of pack years | >1 | 0.9 to 1 | 0.5 to 0.9 | <0.5 |
|---|---|---|---|---|
| <1 | 5 | 21 | 12 | 1 |
| >1 | 1 | 78 | 36 | 2 |
Table 9: No. of pack years and ABPI in 51 to 60 year age group.
χ2=11.75 p ≤ 0.01 highly significant
Less than 1 pack years are having more ABPI index score.
More than 1 pack years are having less ABPI index score.
This is in accordance with the study by Svein, et al. which showed both current (OR men 3.8, confidence interval (CI) 2.1-6.7, OR women 2.2, CI 1.4-3.4) and former smokers (OR men 1.7, CI 0.9- 3.2, OR women 1.7, CI 1.1-2.7) had a higher prevalence of PVD compared with those who had never smoked [20].
Conclusion
ABPI index is a simple, non-invasive cost effective and yet powerful method to screen the population for Peripheral vascular diseases.
Smokers from the very young age group of 30 years itself have evidence of peripheral vascular disease, although asymptomatic. This is proved by the decrease in ABPI index which was statistically significant.
As the number of pack years increased, the risk of moderate to severe peripheral vascular disease increases.
So even if the smokers are asymptomatic it becomes imperative to screen the population for the early signs of peripheral vascular disease.
This screening is particularly effective with increasing age, duration and the number of pack years.
Screening the smokers for the early signs of peripheral vascular diseases will enable the health care providers to objectively guide and advice the importance of stopping smoking which would definitely prevent the catastrophic effect on cardiovascular, central nervous system and renal system. This can go a long way to help a nation to cut short the financial burden on health care system.
REFERENCES
- Artazcoz AV, Ruiz-Garcí J, Alegria-Barrero E, Navarro ACR, Santiago MC, Blázquez MA, et al. Diagnosis of peripheral vascular disease: Current perspectives. J Anesth Clin Res. 2015; 6: 1-7.
- Brass EP, Hiatt WR, Green S. Centre National Clinical Guideline. Lower limb peripheral arterial disease: Diagnosis and management. London: Natl Clin Guidel Cent. 2012.
- Brass EP, Hiatt WR, Green S. Skeletal muscle metabolic changes in peripheral arterial disease contributes to exercise intolerance: A point-counterpoint discussion. Vasc Med. 2004; 9: 293-301.
- Gornik HL, Beckman JA. Peripheral arterial disease. Circulation. 2005; 111: e169-172.
- Criqui MH, Fronek A, Barrett-Connor E, Klauber MR, Gabriel S, Goodman D. The prevalence of peripheral arterial disease in a defined population. Circulation. 1985; 71 (3): 510-515
- Premalatha G, Shanthirani S, Deepa R, Markovitz J, Mohan V. Prevalence and risk factors of peripheral vascular disease in a selected South Indian population: The Chennai Urban Population Study. Diabetes Care. 2000; 23 (9): 1295-300.
- AbuRahma AF, Bergan JJ. Noninvasive peripheral arterial diagnosis. London: Springer. 2010.
- Lin JS, Olson CM, Johnson ES, Whitlock EP. The ankle-brachial index for peripheral artery disease screening and cardiovascular disease prediction among asymptomatic adults: A systematic evidence review for the U.S. preventive services task force. Ann Intern Med. 2013; 159: 333-341.
- Cain LR, Blaha MJ, DeFilippis AP, Mentz RJ, Kamimura D, White WB, et al. Cigarette smoking and subclinical peripheral arterial disease in blacks of the jackson heart study. J Am Heart Assoc. 2019; 8 (3): e010674.
- Ingolfsson IO, Sigurdsson G, Sigvaldason H, Thorgeirsson G, Sigfusson N. A marked decline in the prevalence and incidence of intermittent claudication in Icelandic men 1968-1986: A strong relationship to smoking and serum cholesterol--the Reykjavik Study. J Clin Epidemiol. 1994; 47 (11): 1237-1243.
- Al-Qaisi M, Nott DM, King DH, Kaddoura S. Ankle brachial pressure index (ABPI): An update for practitioners. Vasc Health Risk Manag. 2009; 5: 833-841.
- Federman DG, Trent JT, Froelich CW, Demirovic J, Kirsner RS. Epidemiology of peripheral vascular disease: A predictor of systemic vascular disease. Ostomy Wound Manage. 1998; 44 (5): 58-62.
- Ramos R, Quesada M, Solanas P, Subirana I, Sala J, Vila J, et al. Investigators prevalence of symptomatic and asymptomatic peripheral arterial disease and the value of the ankle-brachial index to stratify cardiovascular risk. Eur J Vasc Endovasc Surg. 2009; 38 (3): 305-311.
- Schroll M, Munck O. Estimation of peripheral arteriosclerotic disease by ankle blood pressure measurements in a population study of 60-year-old men and women. J Chronic Dis. 1981; 34 (6): 261-269.
- Van Kuijk JP, Flu WJ, Bax JJ, Poldermans D. Prevalence of (A) symptomatic peripheral arterial disease: The additional value of ankle-brachial index on cardiovascular risk stratification. Eur J Vasc Endovasc Surg. 2009; 38 (3): 312-313.
- Kubota Y, Higashiyama A, Marumo M, Konishi M, Yamashita Y, Tashiro C, et al. Detection of subclinical peripheral artery ischemia in healthy male smokers by an ankle-brachial index after exercise: Sasayama study. Angiology. 2017; 68 (9): 769-775.
- Donald C, Cain LR, Blaha MJ, DeFilippis AP, Mentz RJ, Kamimura D, et al Cigarette smoking and subclinical peripheral arterial disease in blacks of the jackson heart study. J Am Heart Assoc. 2019; 8: e010674.
- Willigendael EM, Teijink JA, Bartelink ML, Kuiken BW, Boiten J, Moll FL, et al. Influence of smoking on incidence and prevalence of peripheral arterial disease. J Vasc Surg. 2004; 40 (6): 1158-1165.
- China YH, Yong J, Jie W, Li F, XiaoYing L, Frank B Hu. Prevalence of peripheral arterial disease and its association with smoking in a population-based study in Beijing, China. J Vasc Surg. 2006; 44 (2): 333-338.
- Svein AJ, Lars JV, Tom IL N, Pål RR, Hans OM. The association between smoking and the prevalence of intermittent claudication. Vasc Med. 2005; 10: 257-263.
Citation: Saravanan J (2021) Detection of Asymptomatic Peripheral Vascular Disease in Healthy Male Smokers between 21 to 60 Years Attending Tertiary Care Hospital Using Ankle Brachial Pressure Index in Urban Chennai: An Observational Study. J Vasc Med Surg. 9: 424.
Copyright: © 2021 Saravanan J. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

