Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
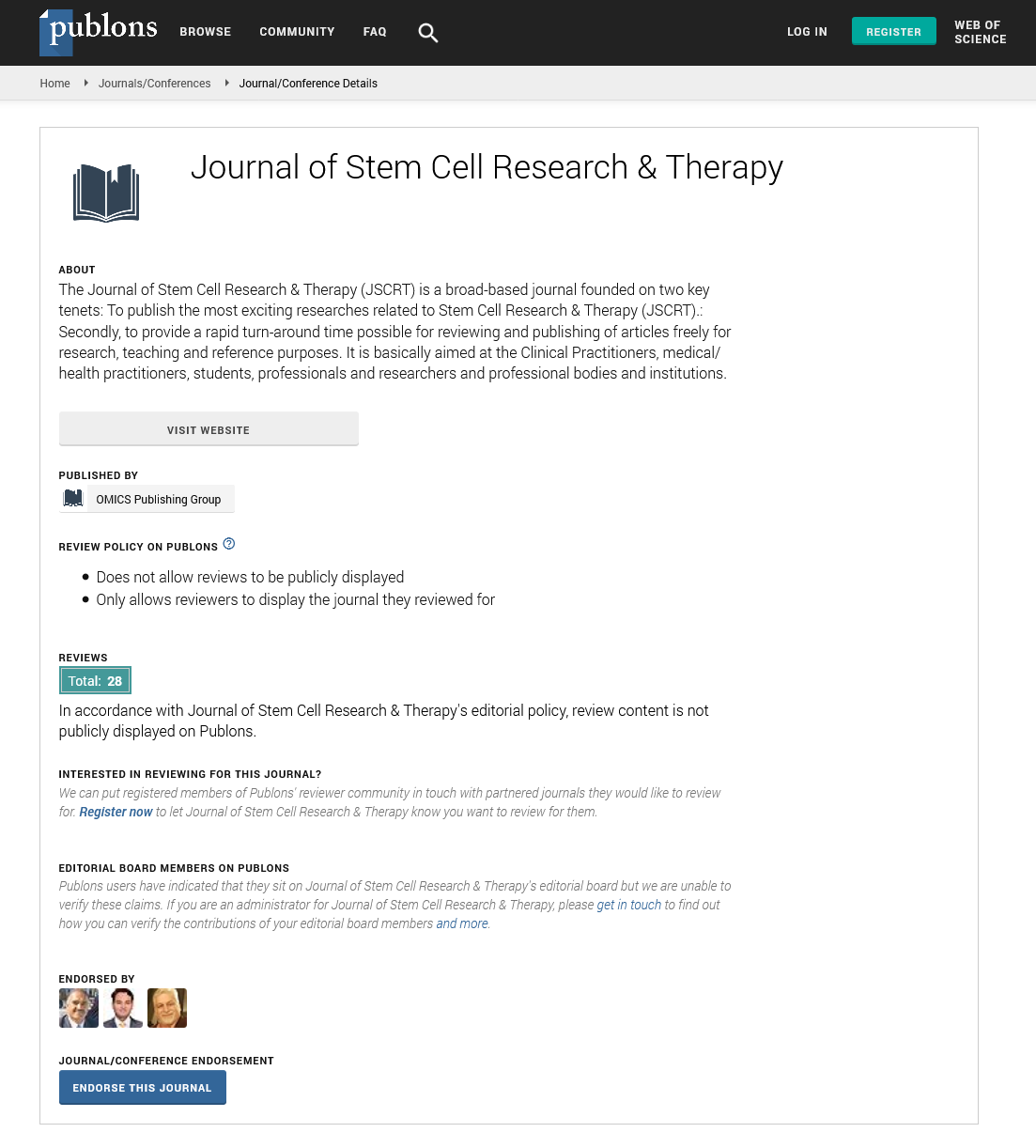
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Editorial - (2021) Volume 11, Issue 12
Current Practices in Liver Cirrhosis Management and Future Prospects: Stem Cell Therapy in Adults
Baskar Subramani*Published: 26-Dec-2021
Introduction
Liver cirrhosis is a leading cause of mortality worldwide. Although treatable by liver transplantation, quality of life is unlikely to drop in all the patients after five years. The shortage of matching donors and the high risk of surgical-associated complications further limits the therapeutic potential of transplantation. Since adult stem cells can be effectively differentiated into hepatocyte-like cells, the potential to translate this utility as a therapeutic alternative has been considerably explored. The bone marrow serves as an ideal source of Hematopoietic Stem Cells (HSCs) and Mesenchymal Stem Cells (MSCs). Although both of these cells have in vivo ability to generate hepatocytes-like cells, MSCs are more potent. Autologous and allogeneic adult stem cell-based therapies have shown promising results in restoring liver function in cirrhosis patients. However, there is still a lack of consensus with regards to the optimum standardization of stem cell source, type, dosage, and mode of transplantation. Many variations exist across the different clinical studies conducted and this hampers the mainstream clinical realization of adult stem cell-based therapy for liver cirrhosis. Thus, this article attempts to review and consolidate the various cellular source, type, dose, and mode of delivery permutations across the various clinical studies published to date.
Liver cirrhosis is an end-stage pathological condition that results from a range of chronic liver diseases. Many chemicals, viruses and toxic substances have been associated with the development of cirrhosis. It is usually characterized by hepatocyte necrosis, defenestration, collagen deposition contributes to fibrosis that ultimately lead to the cumulative loss of liver function. In addition, liver cirrhosis is also characterized by the formation of regenerative nodules that eventually replace the entire liver architecture, leading to decreased blood flow throughout the liver. Besides reduced quality of life, individuals with liver cirrhosis also have an increased risk of liver cancer. As a result, liver cirrhosis accounts for more than one million worldwide deaths annually and an even greater disease-associated morbidity burden. The treatment of cirrhosis is designed to hinder further liver damage, treat cirrhotic complications and prevent liver cancer. Unfortunately various therapeutic-associated limitations have led to the increase in fatality rates over the years. At present the only effective therapeutic option is Orthotopic Liver Transplantation (OLT). OLT for liver cirrhosis result in a 5-year survival rate of about 70%. However, the efficacy and widespread application of OLT is hampered by the shortage of matching donors, surgery-associated morbidities and risk of graft-rejection. These limitations have driven researchers and clinicians to develop novel therapeutic strategies to reduce the morbidity and mortality burden of the disease.
Stem cell therapy has emerged as an attractive therapeutic approach for a myriad of life-threatening diseases in recent years. Specifically, cell-based therapies for liver cirrhosis have successfully progressed from preliminary laboratory and pre-clinical evaluations. Several studies have demonstrated that residential and non-residential liver stem cells have the ability to differentiate into hepatocyte-like cells or bile duct epithelial cells, and more pertinently restore liver function. The mechanistic action of stem cell-mediated restoration of liver function in liver cirrhosis has not been fully defined. However, several mechanisms have been proposed. Some studies suggest the presence of autocrine signalling, whereby the transition of stem cells into hepatocytes-like cells is induced by the secretion of Hepatocyte Growth Factor (HGF). In contrast, some studies postulate that paracrine signaling mediates liver regeneration through revascularization and enhancing repopulation of endogenous cells in necrotic tissue through the secretion of various cytokines and growth factors. Stem cells may also attenuate liver fibrogenesis by inhibiting the activation of hepatic stellate cells (cells responsible for the secretion of extracellular matrix components that include collagen and adhesive glycoproteins) via stem cell-derived cytokines and growth factors such as IL6, IL10, TNFα and HGF. For example, HGF directly suppresses hepatic stellate cell activation by blocking the Extracellular Signal-Regulated Kinase (ERK) and Transforming Growth Factor (TGF-β) signaling pathways.