Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Euro Pub
- Google Scholar
- Quality Open Access Market
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Short Communication - (2022) Volume 8, Issue 2
Continuous Erector Spinae Plane Block as Effective Opioid Sparing Technique in Robotic-Assisted Thoracic Surgery
Marco Cavaleri*Received: 17-Jan-2022, Manuscript No. JPMME-22-15484; Editor assigned: 21-Jan-2022, Pre QC No. JPMME-22-15484 (PQ); Reviewed: 04-Feb-2022, QC No. JPMME-22-15484; Revised: 11-Feb-2022, Manuscript No. JPMME-22-15484 (R); Published: 18-Feb-2022, DOI: 10.35248/2684- 1320.22.8.166
Description
Erector Spinae Plane Block (ESPB) is a newly described fascial plane block, reported both for intra- and post-operative pain management indications. Thoracic surgery is among the most painful surgical procedures, even when conducted with minimally invasive approach. A cornerstone of thoracic pain management for several years has been the epidural analgesia alongside the growth of paravertebral block and recently with fascial plane block. In the last decade, Robotic-Assisted Thoracoscopic Surgery (RATS) has emerged as a further development of minimally invasive surgery. As far as is thought that minimally invasive procedures and thus robotic surgery is associated with lower pain-related morbidity, it must be noted that even the most minimally invasive procedures on the chest can be painful. Perioperative thoracic pain is deemed to be related to a significant increase of postoperative complications linked both to the negative impact of Postoperative Pain (PP) itself on pulmonary function and cardiovascular system but also to the higher doses of systemic drugs needed, with the opioids as the most prescripted, with drug related side effects like over-sedation, delirium, Postoperative Nausea and Vomiting (PONV) or urinary retention. Thus PP may results in worsening outcomes and longer Lenght of Stay (LOS) of major surgical patients. Enhanced Recovery after Surgery (ERAS) protocols have established a paradigmal shift in the surgical pain management with the implementation of regional analgesic techniques aimed to reduce systemic opioid’s use during minimally invasive thoracic surgery [1]. In order to improve the pain management, intravenous pain medications have been combined with regional analgesic techniques such as thoracic epidural blockade and different regional block techniques, leading to a so called multimodal analgesic approach. Regional blocks offer advantages for PP management compared to other strategies, complementing paramount ERAS indications, reducing the prescription of systemic opioid and overall complication rates. Among the regional blocks the ESPB is a novel fascial plane block recently spreading worldwide with promising results. The first description of ESPB dates from the 2016 by Forero and colleagues [2] as innovative analgesic technique for the acute and chronic thoracic pain. The ESPB is provided with ultrasound guide injecting the Local Anesthetic (LA) mixture preferably between the erector spinae muscle plane and the transverse process. An injection in this plane is deemed to allow the block of both the dorsal and ventral rami as they arise from the homolateral thoracic roots to innervate the chest wall (Figure 1). Moreover the decrease of visceral pain reported with ESPB is thought to be linked with the migration of LA through the costo-transverse foramen towards the paravertebral space [3]. Recent studies have shown that this analgesic technique can be safely and effectively used both in cardio- thoracic as well in spine and chest trauma surgery. The ESPB is technically simpler as compared to thoracic epidural anesthesia or paravertebral block and a significant cranial-caudal spread occurs from a single injection point, which is an additional advantage compared to multi injection techniques like intercostal block. Given the high rate of reabsorption of the LA mixture in several analgesic blocks particularly in paravertebral and epidural spaces, the systemic absorption of LA might be a contributing factor limiting the effectiveness of the ESPB to a shorter than expected duration. Therefore the analgesic duration may be prolonged with the placement of an indwelling ESP catheter in all the patients scheduled for surgical procedures with expected high-level of PP as emerging in literature with evidence of several case reports. In line with this preliminary results it has been reported a significant reduction of postoperative pain medication, and particularly the prescription of systemic opioids, in a small but promising case series during RATS with continuous ESPB for 48 h in the postoperative phase. In those patients receiving continuous ESPB compared to patients scheduled for RATS but with no ESPB the reported Mean Morphine Equivalent (MME) was lower with 15 vs. 28 MME [4]. It is fair that it must be cautious with claiming any conclusions given these preliminary data, still derived from a small and retrospective case series. Although the ESPB is gaining popularity as analgesia in thoracic surgery, there has been limited study of its clinical efficacy compared with the current gold standard of thoracic epidural analgesia. Nevertheless, in conjunction with several data recently stemming from ESPB implementation in different surgical scenarios and in well-designed settings as randomized controlled trials [5], it must be reasonable taking into account the ESPB as safe and effective analgesic technique with proven opioid sparing effects during minimally invasive thoracic procedures.
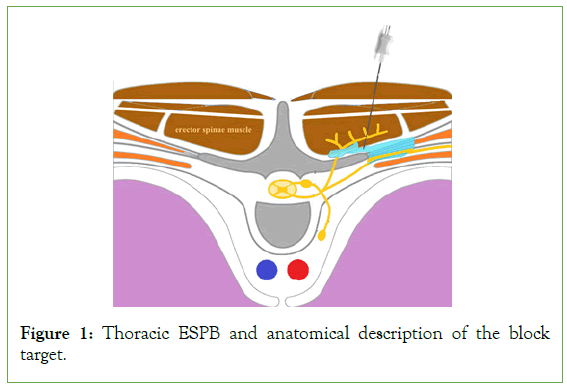
Figure 1: Thoracic ESPB and anatomical description of the block target.
REFERENCES
- Thompson C, French DG, Costache I. Pain management within an enhanced recovery programs after thoracic surgery. J Thorac Dis. 2018;10(32):3773-3780.
[CrossRef] [GoogleScholar] [PubMed]
- Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41(5):621-627.
[CrossRef] [GoogleScholar] [PubMed]
- Saadawi M, Layera S, Aliste J, Bravo D, Leurcharusmee P, Tran DQ. Erector spinae plane block: A narrative review with systematic analysis of the evidence pertaining to clinical indications and alternative truncal blocks. J Clin Anesth. 2021; 68:110063.
[CrossRef] [GoogleScholar] [PubMed]
- Cavaleri M, Tigano S, Nicoletti R, La Rosa V, Terminella A, Cusumano G, et al. Continuous Erector Spinae Plane Block as Postoperative Analgesic Technique for Robotic-Assisted Thoracic Surgery: A Case Series. J Pain Res. 2021;14:3067-3072.
[CrossRef] [GoogleScholar] [PubMed]
- van den Broek RJ, Koopman JS, Postema JM, Verberkmoes NJ, Chin KJ, Bouwman RA, et al. Continuous erector spinae plane block versus thoracic epidural analgesia in video-assisted thoracic surgery: A study protocol for a prospective randomized open label non-inferiority trial. Trials. 2021;22(1):1-3.
[CrossRef] [GoogleScholar] [PubMed]
Citation: Cavaleri M (2022) Continuous Erector Spinae Plane Block as Effective Opioid Sparing Technique in Robotic-Assisted Thoracic Surgery. J Pain Manage Med. 8:166.
Copyright: © 2022 Cavaleri M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

