Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2022) Volume 13, Issue 2
Complications of Perimenopause and Postmenopausal Women and Treatment Patterns
Chillara Tejaswi*Received: 02-Feb-2022, Manuscript No. JCRB-22-11520; Editor assigned: 04-Feb-2022, Pre QC No. JCRB-22-11520 (PQ); Reviewed: 18-Feb-2022, QC No. JCRB-22-11520; Revised: 22-Feb-2022, Manuscript No. JCRB-22-11520 (R); Published: 28-Feb-2022, DOI: 10.35248/2155-9627.22.13.400
Abstract
Menopause is a normal part of aging. Women generally spend their half of the life in menopause after their reproductive hormone years have been ended. During this time, in menopause they experience a lot and variety of symptoms and conditions, it related to sexual changes and age. And symptoms include irregularity of menstrual cycle and they may have hot flashes and night sweats and vaginal dryness depression and some experience headaches and joint pains. The common age of menopause is 51. And menopause and post menopause and perimenopause are stages when women monthly period stops. Perimenopause is the first stage in this stage and it can start 8-10 years before menopause and menopause is a condition when women cannot get period for 12 months and post menopause is after the menopause. And menopause it is occurred when the age of 45-55, when women get menopause before the age of 45 and it is called premature menopause. Menopause is a natural condition they may not need any type of treatments. But to control the symptoms they may have lot of treatments available. Hormonal therapy and nonhormonal therapy are available. In hormone therapy they give estrogen therapy and estrogen progesterone therapy they decrease the many symptoms. Some risks also include in this treatments. In non-hormonal treatments they suggest the maintain diet and vitamin D supplements and calcium supplements they given. Complications include: osteoporosis and osteopenia, coronary heart diseases and menstrual problems.
Keywords
Menopause; Osteoporosis; Depression; HRT
Introduction
include the major functions. One is production of eggs and hormone secretion [2-4]. They both change when women get aged. Menopause is considered when severe amenorrhea occurs after 12 months of your last period, so permanent loss of ovarian function occur. The common age of menopause is 51 years and it is discovered as the menopausal transition a period when, endocrine, and biological, and clinical features of appearing of menopause. Women mostly having their last third of their lifetime and 25% of their life in menopause and, after the reproductive have been ended. Menopause changes having few or less or no symptoms meanwhile some women have significant and even disabling symptom. Natural menopause is identified to having after 12 months of amenorrhea and there is no exact cause as pathological or physiological. Menopause is started when the final menstrual period occurs after 1 year or 12 months of your last menses cycle. Most of the menopause women will experience small and even changes in sexual function during the before and after the menopause condition. Menopause women experience common sexual complications in this include loss of desire and decreasing the sexual responsiveness and dysfunctions in the male partners also. Osteoporosis in menopause is a disease condition decreasing of skeletal mass and micro architectural deterioration of skeleton and it leads to osteoporotic fractures and risk of spine and hip fractures. Decreased levels of ovarian hormone production may have risk for the osteoporotic fractures, so that causing the skeletal reabsorption and decreased bone formation. The most prevalent menopausal symptoms were joint pain and muscular discomfort, physical mental exhaustion, and hot flashes. Natural menopause occurred at age of 48 years. During menopause, women experience different symptoms like hot flashes, night sweats [5]. Menopause is common event for women. The most severe and dangerous symptoms are having women in menopause stage and these symptoms will effect women and their overall quality of life.Hormone replacement therapy is most effective and useful treatment for menopausal women and it is known to be useful and maintain quality of life and control the symptoms in menopausal women. And another is exercise it has been offered an alternative treatment option for alleviating menopausal symptoms, including physiological vasomotor (like hot flashes) and somatic sexual symptoms. And the menopausal and hormonal changes are associated with variety of symptoms, which can affect the morbidity. Generally vasomotor symptoms are most commonly reported, but vaginal dryness/dyspareunia, sleep difficulties, poor sleep and mood changes have been all are severe in women approach or entered in menopause. At the stage of menopause women are having many changes like, they having hormone changes and sexual responsiveness and decreases the orgasms and these changes are reason for many health conditions like women menstrual cycle and urinary disturbances and postmenopausal osteopenia and osteoporosis [6]. In preventing menopausal disease is only with estrogen hormone replacement therapy and the use of EHRT is has been well documented. Decreases in ovarian hormones that occur with menopause have been implicated in these. Systemic vasomotor symptoms are classic cluster affecting 80% of perimenopause and postmenopausal women. Menopause can be distressing and disruptive time for many women, with variety of symptoms. Menopause is considered as three stages: perimenopause and menopause and post menopause. Perimenopause starts from 8-10 years before the menopause and menopause is considered when periods have been stopped and post menopause is not having period after 12 months or more.
Hormone replacement therapy
For several or years early observational studies on Hormone replacement therapy is having many benefits include reduces the cardiac diseases and mortality. Much number of women should select HRT for their menopausal status and it is the beneficial treatment. HRT also decreases the various symptoms of the menopause and risk of osteoporotic fractures estrogen remains the most effective treatment for the vasomotor symptoms and genitourinary syndrome of for osteoporosis prevention. For women who are contraindicated for hormone replacement Therapy and personally reject then, non-hormonal, treatments will be given for to treat both systemic and local menopausal symptoms. HRT: has been shown to be effective in controlling the symptoms of menopause. Many serious adverse effects are associated with this treatment experimental studies tell that black cohosh may be alternative treatment for menopause, and its biologically possible treatment [7-9]. Recent studies suggest that HRT is cardio protective when injected early and after menopause. It is generally having benefits of menopausal hormone therapy outweigh risks but there are still some concerns about the administration of menopausal HT, also introduced alternative treatment. If there are any contraindications in HR, alternative treatments are also solving the symptoms. HRT: various types doses as well different combinations will offer different advantages in different age group of women and the most favorable benefits from HRT is in symptomatic younger women (50-59) within 10 years since menopause. Beside the effect on symptoms patient additional benefits of reduce risk of CVD and Osteoporotic fractures. In older women HRT is better safety than oral combinations. Currently does not support use of HRT for the osteoporosis or CVD and cognition decline prevention. In 1960 first hormonal treatment of menopause is estrogen therapy. Estrogen therapy can decrease in the postmenopausal bone loss, where they take in the early postmenopausal time. Some women will experience premenopausal to postmenopausal without any symptoms at all [10]. Most of the women may experience after the menopause is lowers the sexual function during before and after the menopausal condition. Main symptoms of menopause is irregular menstrual periods, and mostly classic symptom is hot flashes most of the women experience this symptom and most of women (1/3) get serious problem, and night time sweating, sleep disturbances, There is lack of estrogen in menopause so they have numerous symptoms. There is no exact mechanism for that.
Complications: Low sexual desire, genitourinary syndrome of menopause; (atrophic vaginitis) this comprising the many atrophic symptoms and signs so they having vulvovaginal symptoms and urinary bladder symptoms. Because of the losing sex steroids, osteoporotic fractures, depression (women who are having these hot flashes and night sweats, they most likely having depressive symptoms). Poor sleep is a complication mostly seen in menopause. Excessive menopausal bleeding, Endometriosis, chronic kidney disease osteoporosis, cardiovascular diseases, insomnia these are the complications of menopause.
There are three different types of menopause:
• Natural menopause (estrogen and progesterone levels were declines).
• Premature menopause (period stops when women get 40).
• Post menopause and perimenopause.
Management of menopause
Hot flashes and a sleep disorders all symptoms are not go without treatment. Mainly prefer Hormone replacement therapy for this condition and the dose and drug delivery to the system will should be different [11]. And aged people like 50-60 age group people will not having any high risk of HRT treatment. And for vasomotor symptoms they take selected antidepressants and gaba agonists. Genitourinary symptoms should be treated with estrogen therapy. Vitamin D supplements should be most useful drugs for the osteoporotic patients [12,13].
Perimenopause
Many women experience erratic periods before final permanent cessation of periods due to decrease levels of ovarian estrogen levels these stage is called perimenopausal stage. Perimenopause is defined as before and after 1 year of last menstrual period. Conception is possible in perimenopause. Perimenopausal changes begin in women age 40s. In this stage periods will vary and irregular and skipped. Fluctuations in estrogen levels begin in 1 year before menopause. And symptoms can last from 6 months to 10 years range and do not exist to severe. Perimenopause is classified as early and late menopause transition stages and as well as early post menopause as a window of develop depressive symptoms. Perimenopause and also called as menopausal transition is associated with different hormonal changes. Perimenopause not only causes vasomotor symptoms but also causes migraine incidence. Migraine is closely linked to perimenopause. And also many women report this condition during this period. But it increased the menstrually related migraine. Treatment options are control the hormone fluctuations with hormone therapy. Many women and other realize that menopause hormone therapy is most effective for menopause women and their quality of life. Abnormal uterine bleeding is the most common complication in perimenopausal women. In worldwide uterine fibroids are most commonly seen in perimenopausal women and also uterine fibroids are mostly associated with abnormal uterine bleeding and may affect fertility [14]. Endometriasis is considered as perimenopausal disease due decreased levels of estrogen levels.
Symptoms
And most common symptom of perimenopause is poor sleep and also depression moods and anxiety these are the common symptoms of perimenopause. And also vaginal and sexual changes and altered mood swings and sleep and irregularities in bleeding patterns and menorrhagia. These are the symptoms will affect the women quality of life. Depression is the most common thing during perimenopause. There are many evidences that changing the hormones and developing the perimenopausal depression [15]. Women may develop more depressive symptoms in perimenopausal stage. And we see that vasomotor symptoms are more related to depressive symptoms during perimenopause. The perimenopause is considered as higher risk of getting depressive symptoms and depressive episodes.
Depression
Depression is presents with physical symptoms like sleep disturbances and fatigue and pain. Supportive counseling and pharmacotherapy also may effective in depression. Depression is a chronic disease.
Migraine
Migraine is a most common neurological headache because of excitability of CNS. Diagnosis based on symptoms. Migraine effects people’s quality of life and work and all. Treatment options are: calcitonin gene related peptide antagonist has been approved. High estrogen levels to be given to the patients.
Contraception in perimenopausal women; women getting aged they fecundity should be decreased and they don’t know until their menopause. Many safety and effective contraception’s are present in perimenopausal women and we are trying to preventing the perimenopausal pregnancies may develops the abnormal uterine bleeding and hot flashes and menopausal irregularities may also develop.
Diagnosis
Diagnosis of perimenopause is identifying the menopause stage and assesses the psychiatric conditions and observes the symptoms. Clinical evaluation and observe the FSH levels.
Therapy: For depressive symptoms give the anti-depressants and psychotherapy-these are the first line therapy for perimenopausal women. And estrogen therapy is not approved for perimenopausal women.
Surgery: However surgery is the main method of choice for uterine fibroids and in the best cure rates. For uterine fibroids aromatase inhibitors and selective estrogen receptor modulators and selective progesterone modulators were given.
Premature menopause: Menopause occurs before 40 is called premature menopause. Premature menopause is prevention of menses due to non-atriogenic ovarian failure before age 40. Risk factors include smoking, under nutrition, chemotherapy, pelvic radiation; these are impairs the ovarian blood supply.
Complications: Hot flashes: hot flashes are rapid heat producing stage. They produce sweating, internal heating. Hot flashes are triggered by temperature in thermos neutral zone.
Irregular period: Also called as oligo menorrhea change in perimenopausal women, because of fluctuations in hormones.
Abnormal uterine bleeding: Patients with heavy bleeding treated with oral estrogens and progestin. The most effective treatment is this is hysterectomy.
Uterine fibroids: Fibroids neoplasms of the uterus, this is treated with the surgery. Most of the fibroids are asymptomatic.
Post menopause
The presents of last menstrual period can be diagnosed as and usually being final if it is followed by 12 months of bleed free interval this stage is called postmenopausal women [16-18]. The average weight of postmenopausal women is 54 years.
Symptoms
The most common symptom is hot flashes in postmenopausal women. Subjective complaints are body pain, bruxisum, sleepiness from sleepiness scale, these are the complaints are from late post menopause group. Decreasing memory loss in early post menopause is also frequently seen in women. Time of Perimenopausal stage the quantity and quality of bone declines, then started risk of fractures in postmenopausal women. Hot flashes and vaginal dryness are mostly commonly seen in postmenopausal women. The loss of sexual interest is associated with age and BMI and having pregnancies. In postmenopausal women osteoporosis fractures are most common and women getting old their bone density will be deviating [19,20].
Treatment
When women having t-score below 2.5 or 2.5 then treatments should be recommended and bisphosphates are most commonly used treatments. Postmenopausal hormone therapy and vitamin D Supplements should be suggested to the patients [21]. Spine and hip fractures are most common in postmenopausal women. Once you diagnosed as osteoporosis, that time to take adequate vitamin D supplements and doing weight bearing exercise. And screening is most important in postmenopausal women and elderly people with additional risk factors for osteoporosis and fractures. Increased vitamin D supplements may increase the low bone mineral density. Risk factors for osteoporosis are diet and life styles and having any other diseases. And also decreasing ovarian function is also main cause for bone loss. Postmenopausal who is having osteoporosis and who is willing to accept any intervention about the condition, bone mass measurement allows the clinician to determine the risk of fractures and to provide interventions if required. And estrogen treatment should reduce the osteoporotic fractures with safety measures and prevents the heart attacks in the age group of 40-50 in postmenopausal women.
Complications
Postmenopausal bleeding: It is the first sign of the endometrial cancer 3% to 7% of women in this condition to get a chance of cancer. And in that endometrial sampling is to detect endometrial cancers. The postmenopausal bleeding is generally considered as bleeding from the uterus and the only bleeding of importance at post menopause. The postmenopausal bleeding cause is benign [22,23].
Postmenopausal women are associated with upper back pain is not well understood. Pain in the area of thoracic spine. Exact mechanisms are unknown but trunk strength and spine morbidity is limited this upper back pain.
Osteoporosis: Osteoporosis is most commonly seen in olderly people. And it is a skeletal muscle disorder. Diagnosis based on the BMD test. Patients with osteoporosis may do physical activities and daily intake of vitamin D and calcium are important for bone health.
Sleep disturbances and pain are closely linked. Insomnia affects the pain interference.
Review of Literature
• Hormones, lifestyles, and optimizing aging. Mary Jane minkin. Obstetrics and gynecology clinics 46 (3), 501-514, 2019.
• PHILIP M
• an overview. Sonja M. minlay: In this study we illustrate that the natural menopause occurs at age of 50-51 years, no other factor appears to have an independent effect on menopause.
• MBCHB, PH D, FRCP Robert Lindasay
• Gergesene Thromb Res, 2019 Dec in this study a strong effect of HRT on atherogenic lipids with a large reduction in the pro-thrombic LP. This study shows that after HRT in postmenopausal women risk at VT.
• Kutlesic Med Pregl.2016 Oct: This study shows that if any contraindications to this HRT then patients may take alternative treatments for the symptomatic relief.
• David T Felson, Yuqing Zhang, Marian T Hannam, Douglas P Kiel, Peter Wilson, J ANDERSON New England journal of medicine 329(16),1141-1146,1993: For long term preservation of bone mineral density, women should take estrogen for at least seven years after menopause.
• This study shows that numerous symptoms can attributed by lack of estrogen at the time of menopause.
• EMAS position statement: Stutu et al. Maturitas. 2020 Jan: Menopausal hormone therapy may improve depressive symptoms in perimenopausal not postmenopausal women.
• E Anne MacGregor. Post Report Health, 2018 Mar: This study shows migraine with or without aura, using lowest doses of transdermal estrogen may control the vasomotor symptoms.
• A systematic review: Gemmell et al. Hum Reproud Update 2017: This study suggests that women should not be reject HRT treatment because of history of endometriasis.
• Differences between early and late post-menopause: Helena Hachul: this study shows that early menopause associated with symptoms and complications related to sleep higher in postmenopausal women.
• Juan Manuel Malaara, Thelma canto de Cetina, Susana Bassol Nancv Gonalez, Leticia Cacique: This study shows frequencies of symptoms are having similar ranges to other countries. Ethic and environmental factors should involve in the appearing vasomotor symptoms
• This study summarizes the diagnosis of the postmenopausal osteoporosis
• This study shows the diagnostic and operative hysteroscopy was effective in controlling postmenopausal bleeding.
• Upper back pain postmenopausal women and associated physical characteristics pence, Luanda McKenna, Robyn Fary Angela Jacques, Kathy Biffa: A modifiable as physical characteristics of postmenopausal women with upper back pain, wooer back extensor muscle endurance is worth considering clinically.
Need for the study
• To assess the complications in perimenopausal women and postmenopausal women.
• To assess the symptoms occurrence in both perimenopausal and postmenopausal women.
• To provide the patient counselling
• To assess the medical management in perimenopausal and postmenopausal women
• To assess the medication compliance and noncompliance in patients
• To assess the severity of symptoms.
Aim and objectives
• To assess the medical management in perimenopausal and postmenopausal complications
• Providing effective patient counseling for obtaining medication adherence and symptomatic relief
• This study is to determine complications in perimenopausal and postmenopausal women
• To assess the occurrence of symptoms in premenopausal and postmenopausal women.
Materials and Methods
Study Site: Laxmi Narasimha Hospital, Hanamkonda
Study Type: Prospective observational study
Study Period: 6 months
Sample Size: 100
Perimenopausal: 47
Postmenopausal: 53
Medical Management: Perimenopausal women 10% of women take medical management:
Failed medical management patients went for the surgery: TAH: 10
TLH: 40
Drugs given after surgery include Cefpodoxime, Ranitidine, Diclofenac, Ondansetron
Postmenopausal: 50
Premarin, Estran, Ostoford
Inclusion criteria
• Women who are at menopause and after menopause
• Age: 35-65 years
Exclusion criteria
• Women are before 35 years of age and after 65.
• Women who are at perimenopause pregnancies
• Women are having acute kidney failures
Source of data
Patient data records:
• Patient demographic details
• Patient symptoms
• Patient previous health issues
• Past history and management
Patient interview:
• Severity of the condition
• Severity of symptoms
• Regular usage of medication
• Patient menstrual cycle regularity
Forms included in the study:
• Data collection form including patient’s demographic details, set of symptoms, triggering factors, type of complication, and treatment.
• Symptoms questionnaire
Study procedure
• Complications based on inclusion and exclusion criteria
• Demographic data was collected from the patient
• Based on age
1. Group 1: 30-45 years (perimenopausal)
2. Group 2: 46-65 years (postmenopausal)
• Based on symptoms patients were peri and postmenopausal women
• By asking patient symptoms they were suffering peri and postmenopausal complications
• By interviewing patient through prescription mild and severity of the condition was analyzed.
• The data collected throughout 6 months from 100 patients was analyzed.
• The summarized data was entered in Microsoft excel
• Patients were separated based on age, complications, symptoms and treatment
• Based on patient medication adherence were divided into:
1. Medication non-adherence
2. Regular medication
The total number of Perimenopausal patients and postmenopausal patients taken for the study are given in Figure 1.
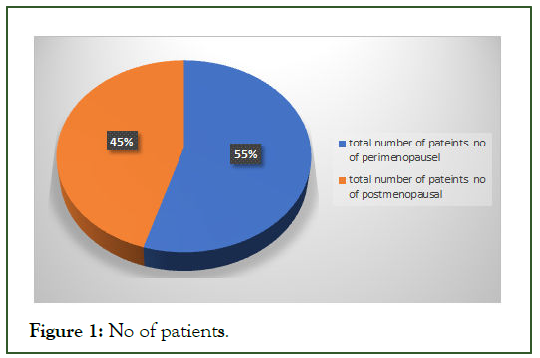
Figure 1: No of patients.
The age wise distribution was given in Table 1 and depicted in Figure 2.
| Age wise distribution | ||
| Age | 35-45 | 46-65 |
| Female | 52 | 43 |
Table 1: Age wise distribution.
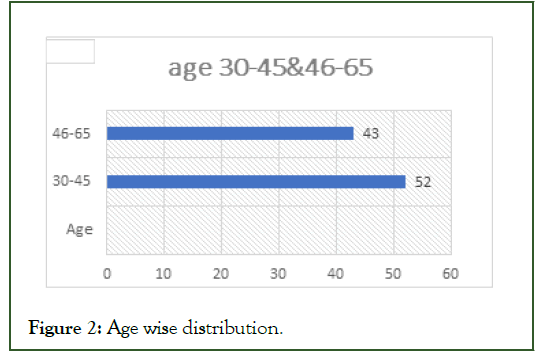
Figure 2: Age wise distribution.
The perimenopausal complications were given in Table 2 and Figure 3.
| Complications | No. of women |
|---|---|
| Hot flashes | 14 |
| Irregular period | 26 |
| Abnormal uterine bleeding | 15 |
| Adenomyosis | 5 |
| Endometriasis | 10 |
| Fibroid uterus | 11 |
| White discharge | 11 |
| Abdomen pain | 35 |
| Urinary disturbances | 11 |
| sleeplessness | 4 |
Table 2: Perimenopausal complications.
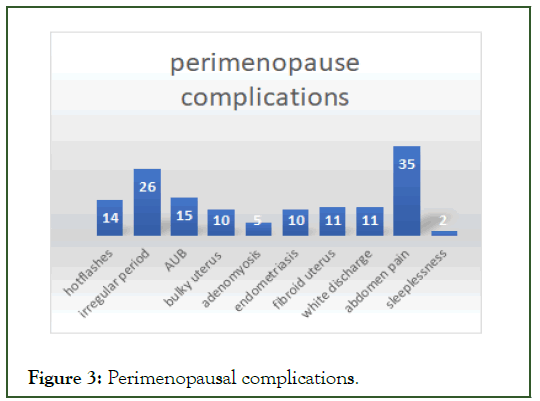
Figure 3: Perimenopausal complications.
The postmenopausal complications were given in Table 3 and Figure 4.
| Complication | No. of women |
|---|---|
| Abdomen pain | 18 |
| Osteopenia | 10 |
| Back pain | 11 |
| Depression | 0 |
| PM bleeding | 30 |
| Burning micturition | 10 |
| White discharge | 25 |
| Osteoporosis | 5 |
Table 3: Post-menopausal complications. 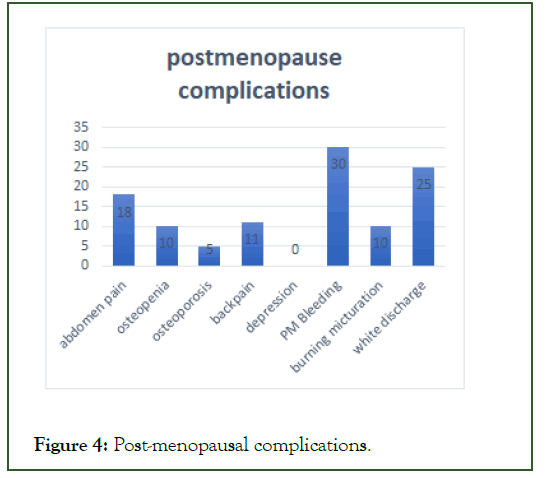
Figure 4: Post-menopausal complications.
The treatment pattern for Perimenopause was given in Table 4 and Figure 5.
| TAH | TLH | Medical managament |
|---|---|---|
| 10 | 40 | 20 |
Table 4: Treatment pattern (Perimenopausal).
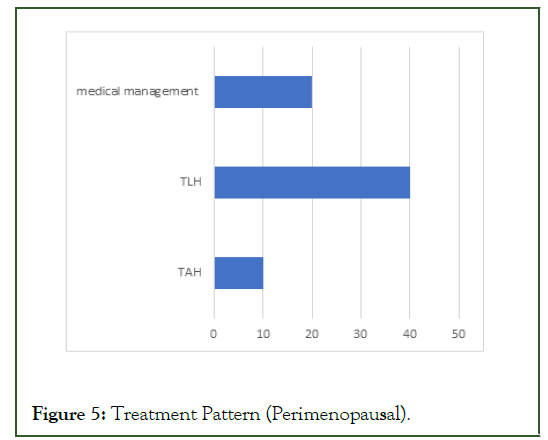
Figure 5: Treatment Pattern (Perimenopausal).
The treatment pattern for Perimenopause was given in Table 5 and Figure 6.
| HRT | Medical management |
|---|---|
| 0 | 50 |
Table 5: Post-menopausal.
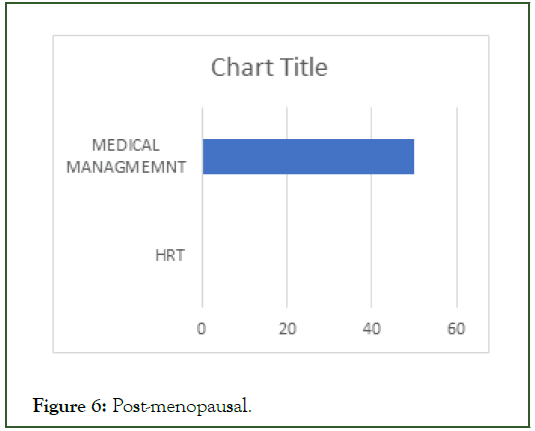
Figure 6: Post-menopausal.
Results and Discussion
Menopause is a normal part of aging and it affects the women quality of life based on the severity of symptom. And menopause having three stages, perimenopause, and menopause and, post menopause. This study provides the information about the symptoms, complication and treatment patterns for both symptoms and complications. In six months of study, complications were analyzed based on the patient’s response, symptoms and treatments in 100 samples. According to our study 10% of the women are go with medical management and failed medical management women are go with the laparoscopic and open surgeries, they do not have any further complications.
And their biopsy reports are all non-cancerous. And postmenopausal women all go with the medical management.
Age: The mean age of our study population was for perimenopause is 40 years and post menopause was after 50 years. And estimation age of menopause was 51. In our study the most effected women are about 40-55 years, because of hormonal fluctuations (estrogen).
Complications
Hot flashes: Hot flashes are a rapid heat producing response, along with sweating, internal heating. Hot flashes are linked to some, not all of the sleep disturbances during menopause. In our study 14.7% of hot flashes were seen in perimenopausal women.
Abnormal uterine bleeding: In our study AUB is most common symptom in perimenopausal women our results are similar to Noah wouk, 2019. Up to 35% of women are taking medication for this problem during this reproductive year have been ending. 15.7% of women are suffering this AUB in their perimenopausal age.
Fibroid uterus: Fibroids may be asymptomatic and symptomatic with heavy menorrhagia, mass, pain. Uterine fibroids also called as leiomyoma. Current treatments are primarily surgery. In our study 13% of women are suffered with this condition, we concluded that via ultrasound scans.
Osteoporosis: At menopause women go with accelerated bone loss. Osteoporosis is reduction of bone tissue, leading to loss of bone strength.in our study 15.7% of women are facing fractures during menopause, we concluded that via BMD test in that T-score is above (-2.5).
Abdomen pain: In this study anxiety, depression, are associated with abdomen pain severe in menopausal transition. In our study 19.8% of women are effected abdomen pain,via ultrasound scans. Our results are similar with Nine G 2019.
Postmenopausal bleeding: In our study 31.5% of women are experience the PM bleeding. PM bleeding is most common presentation in gyneic unit.
Depression: Depression impacts the women quality of life. In our study 2% of women will effect by this condition, via depression scale. Our results are similar to Bathsheba Anwari 2017.
Leucorrhea: In our study 25% of women are suffering this condition and this is the indication for hysterectomy for the infection and pain.
Conclusion
Based on our study we concluded that, perimenopausal women are having complications of hot flashes, abdomen pain, bulky uterus, adenomyosis, of irregular menstrual cycle, abnormal uterine bleeding. Postmenopausal women are facing complications of PM bleeding, osteoporosis, leucorrhea, osteopenia, depression. Most of the women under went for the surgery like TAH and TLH are present most effective treatment.
REFERENCES
- Sarrel PM. Sexuality and menopause. Obstet Gynecol. 1990;75(Supplement):31S.
[Google Scholar], [Pubmed]
- Lindsay R. Pathogenesis of postmenopausal osteoporosis. Baillieres Clin Rheumatol. 1993;7(3):499–513.
- Tella SH, Gallagher JC. Prevention and treatment of postmenopausal osteoporosis. J Steroid Biochem Mol Biol. 2014;142:155–170.
[Crossref], [Google Scholar], [Pubmed]
- McKinlay SM, Brambilla DJ, Posner JG. The normal menopause transition. Maturitas. 2008;61(1–2):4–16.
[Crossref], [Google Scholar], [Pubmed]
- Harris AL. Perimenopause and Post menopause. In: Guidelines for Nurse Practitioners in Gynecologic Settings. New York, NY: Springer Publishing Company; 2020.
[Crossref], [Google Scholar]
- Ulin M, Ali M, Chaudhry ZT, Al-Hendy A, Yang Q. Uterine fibroids in menopause and perimenopause. Menopause. 2020;27(2):238–242.
[Crossref], [Google Scholar], [Pubmed]
- Stute P, Spyropoulou A, Karageorgiou V, Cano A, Bitzer J, Ceausu I, et al. Management of depressive symptoms in perimenopausal and postmenopausal women: EMAS position statement. Maturitas. 2020;131:91–101.
[Crossref], [Google Scholar] [Pubmed]
- MacGregor EA. Migraine, menopause and hormone replacement therapy. Post Reprod Health. 2018;24(1):11–18.
[Crossref], [Google Scholar], [Pubmed]
- Van Hanegem N, Prins MMC, Bongers MY, Opmeer BC, Sahota DS, Mol BWJ, et al. The accuracy of endometrial sampling in women with postmenopausal bleeding: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2016; 197:147–155.
[Crossref], [Google Scholar] [Pubmed]
- Townsend DE, Fields G, McCausland A, Kauffman K. Diagnostic and operative hysteroscopy in the management of persistent postmenopausal bleeding. Obstet Gynecol.1993;82(3):419–421. [Google Scholar] [PubMed]
- Spencer L, McKenna L, Fary R, Jacques A, Briffa K. Upper back pain in postmenopausal women and associated physical characteristics. PLoS One. 2019.
[Crossref],[Google Scholar], [PubMed]
- Lindsay R, Cosman F. Pathogenesis of Osteoporosis. In: Treatment of the Postmenopausal Woman. Elsevier; 2007. p. 323–330.
[Crossref], [Google Scholar]
- Vestergaard P. Anti-resorptive therapy for the prevention of postmenopausal osteoporosis: when should treatment begin? Treat Endocrinol. 2005;4(5):263–277.
[Crossref], [Google Scholar], [PubMed]
- Minkin MJ. Menopause: Hormones, lifestyle, and optimizing aging. Obstet Gynecol Clin North Am. 2019;46(3):501–514.
[Google Scholar] [PubMed]
- Baldi S, Becorpi A. Prevention, diagnosis and treatment of osteoporosis following menopause induced due to oncological disease. Clin Cases Miner Bone Metab. 2009;6(3):261–263.
[Google Scholar], [Pubmed]
- Paciuc J. Hormone therapy in menopause. Adv Exp Med Biol. 2020;1242:89–120.
[Crossref],[Google Scholar], [Pubmed]
- Gregersen I, Høibraaten E, Holven KB, Løvdahl L, Ueland T, Mowinckel M-C, et al. Effect of hormone replacement therapy on atherogenic lipid profile in postmenopausal women. Thromb Res. 2019;184:1–7.
[Crossref], [Google Scholar] [Pubmed]
- Kutlesic R M, Popovic J, Stefanovic M, Vukomanovic P, Lukic B, Lilic G. Alternatives of menopausal hormone therapy. Med Pregl. 2016;69(5–6):177–182.
[Crossref],[Google Scholar],[Pubmed]
- Gambacciani M, Levancini M. Hormone replacement therapy: who should be treated? Minerva Ginecol. 2015;67(3):249–255.
[Google Scholar], [Pubmed]
- Felson DT, Zhang Y, Hannan MT, Kiel DP, Wilson PWF, Anderson JJ. The effect of postmenopausal estrogen therapy on bone density in elderly women. Obstet Gynecol Surv. 1994;49(3):201–203.
[Crossref] [Google Scholar], [Pubmed]
- Grossmann M, Ramchand SK, Milat F, Vincent A, Lim E, Kotowicz MA, et al. Assessment and management of bone health in women with oestrogen receptor-positive breast cancer receiving endocrine therapy: Position statement of the Endocrine Society of Australia, the Australian and New Zealand Bone & Mineral Society, the Australasian Menopause Society and the Clinical Oncology Society of Australia. Clin Endocrinol Oxf. 2018;89(3):280–296.
[Crossref], [Google Scholar] [Pubmed]
- Santoro N. Perimenopause: From research to practice. J Womens Health (Larchmt). 2016;25(4):332–339.
[Crossref], [Google Scholar], [Pubmed]
- Brzezinski A. Menopausal symptoms: Not just estrogen deficiency. Menopause. 2018;1.
[Crossref],[Google Scholar], [Pubmed]
Citation: Tejaswi C (2022) Complications of Perimenopause and Postmenopausal Women and Treatment Patterns. J Clin Res Bioeth. 13:400.
Copyright: © 2022 Tejaswi C. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

