Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Euro Pub
- Google Scholar
- Quality Open Access Market
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2023) Volume 9, Issue 1
Comparison of Cooled Radiofrequency Ablation and Genicular Nerve Blockade for the Treatment of Osteoarthritic Knee Pain: A Prospective Randomized Double-Blind Study
Samer Khojah1, Eyad Mitwali1, Osama AlAhdal2 and Abdullah Kaki3*2Department of Pain Medicine, International Medical Center, Jeddah, Saudi Arabia
3Department of Anesthesiology and Pain management, King Abdulaziz University Hospital, Jeddah, Saudi Arabia
Received: 24-Dec-2022, Manuscript No. JPMME-22-19450; Editor assigned: 26-Dec-2022, Pre QC No. JPMME-22-19450 (PQ); Reviewed: 09-Jan-2023, QC No. JPMME-22-19450; Revised: 16-Jan-2023, Manuscript No. JPMME-22-19450 (R); Published: 26-Jan-2023, DOI: 10.35248/2684-1320.23.9.190
Abstract
Background: Osteoarthritis is a chronic degenerative disease that can represent a source of significant pain. When conservative therapies fail to relief the pain and surgery is not an option. Other choices like Genicular Nerve Blockade (GNB) using a mixture of local anesthetic agents and steroids or genicular nerve ablation using a Cooled Radio Frequency Ablation (CRFA) will be the option.
Methods: In this prospective randomized double-blind study, 41 patients with chronic osteoarthritic knee pain were randomly assigned to either CRFA (n=21) of genicular nerves or GNB (n=20) at the superomedial, superolateral, and inferomedial aspects of the knee. Pain status and patient function were assessed using numerical pain score and Sfax Western Ontario McMaster Universities Osteoarthritis (WOMAC) index respectively, at 3, 6, 9, and 12 months after the intervention.
Results: The mean age of the patients was 71.2 ± 9.5 (mean ± SD) years, with marked female dominance (73.2%). Severity of pain, WOMAC score, or the used medications were not significantly different between the groups (p>0.05). Reduction in the average pain score and WOMAC index (p<0.05) after the intervention was significantly different within the groups but not between the groups (p>0.05). Pain relief lasted for a significantly longer duration in CRFA patients (6.8 ± 4.61 months) than in GNB patients (2.9 ± 1.17 months) (p<0.05). There were no reported complications.
Conclusions: Both CRFA and GNB were significantly effective in reducing pain and improving the function of knee osteoarthritis; however, CRFA is superior to GNB regarding the duration of pain relief.
Keywords
Knee pain; Osteoarthritis; Cooled radiofrequency; Genicular nerve blockade; Pain relief
INTRODUCTION
Osteo-Arthritis (OA) is a chronic degenerative disease that can represent a source of significant pain, disability, and reduced quality of life [1]. Osteoarthritic knee pain is an independent risk factor for early mortality and thus, reducing pain due to knee OA is a global health concern [2]. When conservative therapies fail to solve the problem, Total Joint Replacement (TJR) surgery is the last resort for severe OA of knee joints. Not all patients are candidates for such a procedure. Comorbidities, age, or other factors could discourage the orthopedic surgeon from proceeding with TJR [3].
There is a limited number of treatment options available for patients who are not candidates for TJR and/or for whom pharmacological therapy is either ineffective or interferes with their quality of life. Intra-Articular Steroid (IAS) injection provides notable short-term pain relief but requires multiple treatments to maintain efficacy, which in turn increases the risk for serious adverse events such as septic arthritis and may exacerbate cartilage destruction [3-5]. Visco-supplementation, which shows moderate effectiveness, is not recommended in the treatment paradigm for knee OA by most societies due to limited supporting data [4,6].
The knee is innervated by branches of several nerves, including the tibial, femoral, saphenous, obturator, and common peroneal nerves. These nerve branches surround the knee from all directions and are called the genicular nerves [7].
Generally, a diagnostic Genicular Nerve Block (GNB) using local anesthetic agents with or without steroids is performed before Radio-Frequency Ablation (RFA) of genicular nerves of the knee, and a positive response to GNB is considered as a good indicator for RFA. However, one study suggested that GNB, when administered together with a corticosteroid, is as effective as RFA of genicular nerves in controlling the pain after knee arthroplasty [8]. Despite this and other reports in which adjuvant corticosteroid therapy could contribute to and prolong the analgesic effect of the local anesthetic, the analgesic effect of corticosteroids on a peripheral nerve block remains controversial [9-12].
On the other hand, Cooled Radio-Frequency Ablation (CRFA) has been introduced to the medical field in the last few years and has shown good pain relief in spine-related conditions for at least 12 months [13-16]. Recently, the use of CRFA as a minimally invasive treatment option for pain relief of knee OA has emerged [17]. CRFA of the genicular nerves seems to be a safe and effective therapy for managing intractable knee OA pain. The procedure is performed using a thermal probe that is directed using fluoroscopy or ultrasound guidance to well-described and validated bony landmarks in the paths of the genicular nerves. A current is applied through the probe to induce a thermal injury to the targeted nerve, which in turn disrupts the nerve signals of pain sensation arising from the knee capsule [18].
We conducted this prospective randomized double-blind study to compare the analgesic effect of CRFA of genicular nerves to GNB using a mixture of local anesthetic agents and methylprednisolone on knee osteoarthritic pain.
Material and Methods
Following the principles of the declaration of Helsinki, a prospective randomized double-blind study was conducted at two tertiary care centers in Jeddah, Saudi Arabia: King Abdulaziz University Hospital, and the International Medical Center. After approval from the Research and Ethics Committee (approval number 214- 20, dated April 20, 2020), 41 patients with knee OA provided written informed consent to participate in this randomized double-blind study. Patients aged 40 years or above with signs and symptoms of knee OA presenting with pain for 6 months or longer that is unresponsive to conservative therapy (oral medications, physical therapy, and IAS injection or visco-supplementation) and confirmed by physical examination and radiological examinations were included in the study. Patients with causes of knee pain besides OA, those with a bleeding tendency or allergy to the study medications, those with diabetes and polyneuropathy of lower limbs, those with previous knee RFA therapy, and those undergoing TJR were excluded from the study.
Study design
Forty one patients with confirmed osteoarthritic knee pain were included in the study. Patients were randomized into two groups using computer-generated randomization. Patients were blinded to the treatment option. CRFA of genicular nerves and GNB were performed for group I and group II, respectively. The intensity of pain at rest was measured with a Numerical Rating Scale (NRS) with 11 points from 0 to 10 (0=no pain, 10=most severe pain ever experienced). The use of NRS to assess the severity of pain was described to the subjects. Sfax modified Western Ontario and McMaster’s Universities Osteoarthritis (WOMAC) index was used to assess the function of the knee and reflect the patient satisfaction after the intervention. It was explained to the patient prior to the procedure. In group I, CRFA utilizing the coolief system (Halyard Inc, Alpharetta, Georgia) was performed at the superomedial and inferomedial genicular branches of the saphenous nerve and the superolateral branch of the femoral nerve after the patient was placed in the supine position and the skin and soft tissue were anesthetized with 1% lidocaine. A 75 mm or 100 mm, 17-gauge radiofrequency needle was inserted in the proper locations. Needle position was confirmed with a true lateral fluoroscopic examination showing the accurate position of the probe at depth correlated with the middle of the femur and tibia shaft on lateral views at the diaphyseal-metaphyseal junction. An internally cooled 4 mm, 18-gauge active tip electrode was introduced through the needle and position was confirmed with anteroposterior and lateral fluoroscopic views.
Motor stimulation at 2 V was performed to exclude any muscular twitch and sensory stimulation at 0.5 V or less was initiated to ensure proximity of the probe to the aimed nerves in all three points. Three milliliters of 2% lidocaine were injected at each point via the inserted needle prior to CRFA at 60°C for 2.5 min. Then, the needle was removed, and the study subjects were observed for 30 min in the post anesthesia care unit before being discharged home. No local anesthetic agent or steroid was injected at the end of the procedure to ensure the proper comparison between the two techniques. Patients were instructed to continue their current medication (either Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) or weak opioids) for any post-procedure pain as a rescue medicine.
In group II, the patients underwent fluoroscopically guided GNB. A 22-gauge spinal needle was used to inject 3 ml of bupivacaine 0.5% mixed with 12 mg of methylprednisolone acetate in the middle of the femur and tibia shaft, at each point of the superomedial, inferomedial, and superolateral aspects. Similar to the positioning of CRFA needles. Aspiration of blood was checked before the injection of the study medication.
NRS score and WOMAC questionnaire was completed by a blind observer to assess the reduction of pain and the improvement in the function at 3, 6, 9, and 12 months after the intervention. In addition to demographic data, clinical data were reported on a data collection sheet.
We adapted a validated Arabic version of the WOMAC index to evaluate the limitation of physical function, but we excluded the questions related to pain intensity and specific joint stiffness. This scale consists of nine questions for the assessment of physical function. All items are rated on a four-point score (0 to 4) for a total of 36 points, developed to help in the assistance of the subject’s functionality post procedures [19]. Complications related to the procedure were reported. All patients were approached via phone call for 9 and 12-month assessments without any dropouts.
Statistical analysis
Data were coded and analyzed using SAS version 9.4 (SAS Institute Inc.). Qualitative variables are summarized and presented as frequency distribution using bar charts. For quantitative data, a test for normality was initially carried out using the one-sample Kolmogorov Smirnov test. Normally distributed variables are presented in mean and standard deviation, while non-normally distributed variables are presented as median and Inter-Quartile Range (IQR), with boxplot graphs for distribution of data. The chi- square test was used to test the significance of categorical variables. For normally distributed quantitative variables, an independent sample t-test was used to find the differences in mean and standard deviation between the two groups; the Mann Whitney test was used for non-normally distributed quantitative variables. Wilcoxon test was used to test for significance in the pre and post-intervention changes. p<0.05 was considered statistically significant.
Results
Forty-one patients with knee OA were randomly assigned to one of two arm interventions, either CRFA (n=21) or GNB (n=20), the pre and post-intervention clinical features and the outcome of the intervention in the patients were assessed.
Table 1 show that the mean age of the patients was 71.2 ± 9.5 years, with marked dominance of female (73.2%), Saudi (82.9%), married (73.2%), unemployed (65.9%) and non-smoker (82.9%) patients. Overall, there was no significant difference between the two groups regarding socio-demographic characteristics (p>0.05).
| Variables | Study group intervention | P values | ||
|---|---|---|---|---|
| CRFA (n=21) | GNB (n=20) | Total | ||
| Gender* | 0.095 | |||
| Male | 8 (38.1%) | 3 (15.0%) | 11 (26.8) | |
| Female | 13 (61.9%) | 17 (85.0%) | 30 (73.2%) | |
| Age** | 0.102 | |||
| Mean ± SD | 74.0 ± 7.54 | 69.2 ± 10.82 | 71.2 ± 9.5 | |
| Nationality* | 0.053 | |||
| Saudi | 15 (71.4%) | 19 (95.0%) | 34 (82.9%) | |
| Non Saudi | 6 (28.6%) | 1 (5.0%) | 7 (17.1%) | |
| Education level* | 0.51 | |||
| Elementary | 9 (42.9%) | 6 (30.0%) | 15 (36.6%) | |
| High school | 7 (33.3%) | 6 (30.0%) | 13 (31.7%) | |
| University & postgraduate | 5 (23.8%) | 8 (40.0%) | 13 (31.7%) | |
| Marital status* | 0.796 | |||
| Married | 15 (71.4%) | 15 (75.0%) | 30 (73.2%) | |
| Single/divorced/widowed | 6 (28.6%) | 5 (25.0%) | 11 (26.8%) | |
| Employment* | 0.44 | |||
| Employed | 6 (28.6%) | 8 (40.0%) | 14 (34.1%) | |
| Unemployed | 15 (71.4%) | 12 (60.0%) | 27 (65.9%) | |
| Smoking status* | 0.24 | |||
| Non smoker | 16 (76.2%) | 18 (90.0%) | 34 (82.9%) | |
| Ever smoker | 5 (23.8%) | 2 (10.0%) | 7 (17.1%) | |
| Note: *Based on chi-square test; **Based on independent samples test. Abbreviation: CRFA: Cooled Radio-Frequency Ablation; GNB: Genicular Nerve Block. |
||||
Table 1: Comparison of demographic characteristics of patients according to type of intervention.
Clinically, most patients were either obese (41.5%) or morbidly obese (31.7%), and almost half of them were in a wheelchair (48.8%). Regarding comorbidities, 75.6% of patients were diagnosed as hypertensive, and one third as diabetic (31.7%). Rheumatological illness and joint injury were reported in 73% of patients. There was no significant difference between the two study groups regarding clinical characteristics (p>0.05) as shown in Table 2.
| Variables | Study group intervention | P*values | ||
|---|---|---|---|---|
| CRFA (n=21) | GNB (n=20) | Total | ||
| Mobilization | 0.866 | |||
| Walking but in pain | 4 (19.0%) | 5 (25.0%) | 9 (22.0%) | |
| Using walking aids | 6 (28.6%) | 6 (30.0%) | 12 (29.3%) | |
| Using wheelchair | 11 (52.4%) | 9 (45.0%) | 20 (48.8%) | |
| BMI categories | 0.328 | |||
| Normal & overweight | 5 (23.8%) | 6 (30.0%) | 11 (26.8%) | |
| Obese | 11 (52.4%) | 6 (30.0%) | 17 (41.5%) | |
| Morbid obesity | 5 (23.8%) | 8 (40.0%) | 13 (31.7%) | |
| Hypertensive | 0.484 | |||
| Yes | 17 (81.0%) | 14 (70.0%) | 31 (75.6%) | |
| No | 4 (19.0%) | 6 (30.0%) | 10 (24.4%) | |
| Diabetic | 0.819 | |||
| Yes | 7 (33.3%) | 6 (30.0%) | 13 (31.7%) | |
| No | 14 (66.7%) | 14 (70.0%) | 28 (68.3%) | |
| Rheumatological illness | 0.519 | |||
| Yes | 2 (9.5%) | 1 (5.0%) | 3 (7.3%) | |
| No | 19 (90.5%) | 19 (95.0%) | 38 (92.7%) | |
| Joint injury | 0.107 | |||
| Yes | 0 (0.0%) | 3 (15.0%) | 3 (7.3%) | |
| No | 21 (100.0%) | 17 (85.0%) | 38 (92.7%) | |
| Other comorbidities | 0.558 | |||
| Yes | 10 (47.6%) | 9 (45.0%) | 19 (46.3%) | |
| No | 11 (52.4%) | 11 (55.0%) | 22 (53.7%) | |
| Note: *Based on chi-square test. Abbreviation: CRFA: Cooled Radio-Frequency Ablation; GNB: Genicular Nerve Block. |
||||
Table 2: Comparison of clinical characteristics of patients according to type of intervention.
Table 3 demonstrates that almost one-half of the patients were categorized as having severe OA (stage IV), either on the right (53.7%) or left knee (46.3%). The median WOMAC index was 25 (IQR:19.5-28) and the pain score in right and left knee was 4 (IQR: 4;4-5) with no significant difference between the two groups. The duration of pain ranged from less than 1 year up to more than 10 years, which was constant in 39.0% of patients and worsened with activities to the extent that 82.9% of patients expressed that pain was limiting their activities. In 46.3% of patients, the pain was waking them up from sleep, with no statistical significance between the two groups (p>0.05).
| Variables | Study group intervention | P values | ||
|---|---|---|---|---|
| CRFA (n=21) | GNB (n=20) | Total | ||
| Severity of osteoarthritis (right) | NA | |||
| Minimal (Stage I) | 0 (0.0%) | 3 (15.0%) | 3 (7.3%) | |
| Mild (Stage II) | 1 (4.8%) | 0 (0.0%) | 1 (2.4%) | |
| Moderate (Stage III) | 11 (52.4%) | 4 (20.0%) | 15 (36.6%) | |
| Severe (Stage IV) | 9 (42.9%) | 13 (65.0%) | 22 (53.7%) | |
| Severity of osteoarthritis (left) | NA | |||
| Minimal (Stage I) | 0 (0.0%) | 1 (5.0%) | 1 (2.4%) | |
| Mild (Stage II) | 2 (9.5%) | 2 (10.0%) | 4 (9.8%) | |
| Moderate (Stage III) | 10 (47.6%) | 7 (35.0%) | 17 (41.5%) | |
| Severe (Stage IV) | 9 (42.9%) | 10 (50.0%) | 19 (46.3%) | |
| WOMAC score; median (IQR) | 24 (17-26.5) | 25.5 (23.3-28.8) | 25 (19.5-28) | 0.182 |
| Pain scale right; median (IQR) | 4 (4-4.5) | 4 (4-6) | 4 (4-5) | 0.089 |
| Pain scale left; median (IQR) | 4 (4-5) | 4 (3-5) | 4 (3-5) | 0.715 |
| Duration of pain | NA | |||
| ≤ 1 year | 2 (9.5%) | 4 (20.0%) | 6 (14.6%) | |
| 3 years | 7 (33.3%) | 1 (5.0%) | 8 (19.5%) | |
| 5 years | 7 (33.3%) | 6 (30.0%) | 13 (31.7%) | |
| 7-10 years | 1 (4.8%) | 6 (30.0%) | 7 (17.1%) | |
| >10 years | 4 (19.0%) | 3 (15.0%) | 7 (17.1%) | |
| Frequency of pain | 0.606 | |||
| Constant | 9 (42.9%) | 7 (35.0%) | 16 (39.0%) | |
| Episodic | 12 (57.1%) | 13 (65.0%) | 25 (61.0%) | |
| Worsening of pain with activity | 0.272 | |||
| Strongly agree | 12 (57.1%) | 8 (40.0%) | 20 (48.8%) | |
| Somewhat agree | 9 (42.9%) | 12 (60.0%) | 21 (51.2%) | |
| Pain limits activities | 0.687 | |||
| Yes | 18 (85.7%) | 16 (80.0%) | 34 (82.9%) | |
| No | 3 (14.3%) | 4 (20.0%) | 7 (17.1%) | |
| Pain interferes with sleep | 0.867 | |||
| Sleep comfortably | 11 (52.4%) | 11 (55.0%) | 22 (53.7%) | |
| Wake up because of pain | 10 (47.6%) | 9 (45.0%) | 19 (46.3%) | |
| Abbreviation: CRFA: Cooled Radio-Frequency Ablation; GNB: Genicular Nerve Block. | ||||
Table 3: Comparison of pre-intervention clinical assessment of patients according to type of intervention.
The overwhelming majority of the patients (97.6%) were using pain medications, mostly NSAIDs (61.0%), acetaminophen (46.3%) and tramadol (48.8%) with no significant difference between the two groups (p>0.05). On the other hand, while a significantly higher proportion of the patients in group II were using opioids (60.0%), a significantly higher proportion of patients who underwent CRFA (66.7%) were using topical medications (p<0.05). Only seven patients reported that they had attempted other treatment modalities such as IAS injection (9.8%), intra-articular platelet- rich plasma injection (4.9%), and intra-articular hyaluronic acid injection (2.4%) (Table 4).
| Medications and treatment modalities | Study group intervention | P*values | ||
|---|---|---|---|---|
| CRFA (n=21) | GNB (n=20) | Total | ||
| Medications | ||||
| Pain medications | 21 (100.0%) | 19 (95.0%) | 40 (97.6%) | 0.488 |
| Tramadol | 12 (57.1%) | 8 (40.0%) | 20 (48.8%) | 0.272 |
| Opioid | 4 (19.0%) | 12 (60.0%) | 16 (39.0%) | 0.007 |
| NSAIDs | 10 (47.6%) | 15 (75.0%) | 25 (61.0%) | 0.071 |
| Acetaminophen | 9 (42.9%) | 10 (50.0%) | 19 (46.3%) | 0.647 |
| Antidepressant | 8 (38.1%) | 4 (20.0%) | 12 (29.3%) | 0.203 |
| Anticonvulsant | 12 (57.1%) | 7 (35.0%) | 19 (46.3%) | 0.155 |
| Topical | 14 (66.7%) | 5 (25.0%) | 19 (46.3%) | 0.006 |
| Transdermal patch | 2 (9.5%) | 2 (10.0%) | 4 (9.8%) | 0.678 |
| Other attempted modalities | NA | |||
| Intra-articular hyaluronic acid injection | 0 (0.0%) | 1 (5.0%) | 1 (2.4%) | |
| Intra-articular platelet rich plasma injection | 1 (4.8%) | 1 (5.0%) | 2 (4.9%) | |
| Intra-articular steroid injection | 3 (14.2%) | 1 (5.0%) | 4 (9.8%) | |
| None | 17 (81.0%) | 17 (85.0%) | 34 (82.7%) | |
| Note: *Based on chi-square test. Abbreviation: CRFA: Cooled Radio-Frequency Ablation; GNB: Genicular Nerve Block. | ||||
Table 4: Comparison of study patients according to medications used before intervention and treatment modalities.
There was no significant difference between the two study groups regarding their demographic and clinical characteristics, which might indicate a good matching between the two groups. The differences in the outcome between the two groups might be attributed to the type of intervention.
Figure 1 illustrates that the interventions were performed mainly bilaterally in the two groups. Table 5 and Figure 2 show that there was a significant reduction in the average pain score after the intervention within the two groups either on the right or left knee, with a significant reduction in the WOMAC index (p<0.05). The comparison for the magnitude of reduction in pain and WOMAC index (difference between pre and post-intervention scores) revealed that there was no significant difference between the two study groups (p>0.05). Most patients expressed that there was an improvement in their function and a decrease or no change in intake of pain medication. Almost three-quarters of them reported that they were satisfied, with no significant difference between the two groups (p>0.05).
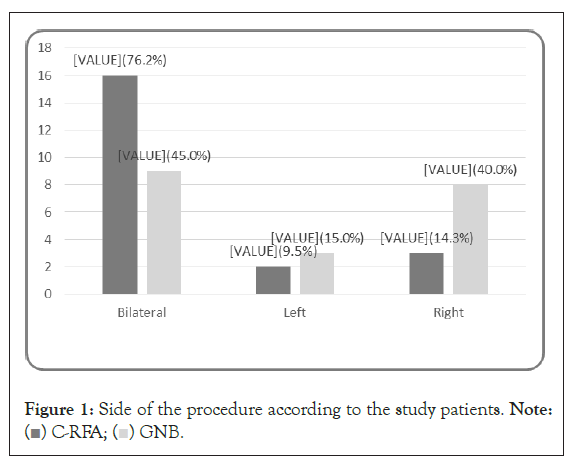
Figure 1: Side of the procedure according to the study patients. Note:
( ) C-RFA; (
) C-RFA; ( ) GNB.
) GNB.
| Variables | Study group intervention | P values | ||
|---|---|---|---|---|
| CRFA (n=21) | GNB (n=20) | Total | ||
| Pain scale right; median (IQR) | 0.66 | |||
| Pre-intervention | 4 (4-4.5) | 4 (4-6) | 4 (4-5) | |
| Post-intervention | 2 (1.5-3) | 2 (1.25-3) | 2 (1.5-3) | |
| P | <0.001 | 0.001 | <0.001 | |
| Average reduction | 2 (0.5-3) | 3 (0-3) | 2 (0-3) | |
| Pain scale left; median (IQR) | 0.595 | |||
| Pre-intervention | 4 (4-5) | 4 (3-5) | 4 (3-5) | |
| Post-intervention | 2 (1-3.5) | 2 (1.25-4) | 2 (1-4) | |
| P | <0.001 | 0.003 | <0.001 | |
| Average reduction | 2 (05-3) | 1.5 (0-2.75) | 2 (0-3) | |
| WOMAC score; median (IQR) | 0.785 | |||
| Pre-intervention | 24 (17-26.5) | 25.5 (23.3-28.8) | 25 (19.5-28) | |
| Post-intervention | 13 (8-19.5) | 15.5 (11.25-26.75) | 14 (9-24.5) | |
| P | <0.001 | 0.001 | <0.001 | |
| Average reduction | 7 (4-11) | 7 (9-12.75) | 7 (2.5-12) | |
| Patient functionality | NA | |||
| Improved | 15 (71.4%) | 13 (65.0%) | 28 (68.2%) | |
| No change | 5 (23.8%) | 4 (20.0%) | 9 (22.0%) | |
| Worsened | 1 (4.8%) | 3 (15.0%) | 4 (9.8%) | |
| Pain medication | NA | |||
| Decreased | 10 (47.6%) | 6 (30.0%) | 16 (39.0%) | |
| No change | 11 (52.4%) | 9 (45.0%) | 20 (48.8%) | |
| Increased | 0 (0.0%) | 5 (25.0%) | 5 (12.2%) | |
| Satisfaction | 0.796 | |||
| Satisfied | 15 (71.4%) | 15 (75.0%) | 30 (73.2%) | |
| Not satisfied | 6 (28.6%) | 5 (25.0%) | 11 (26.8%) | |
| Abbreviation: CRFA: Cooled Radio-Frequency Ablation; GNB: Genicular Nerve Block. | ||||
Table 5: Comparison of outcome of patients according to type of intervention.
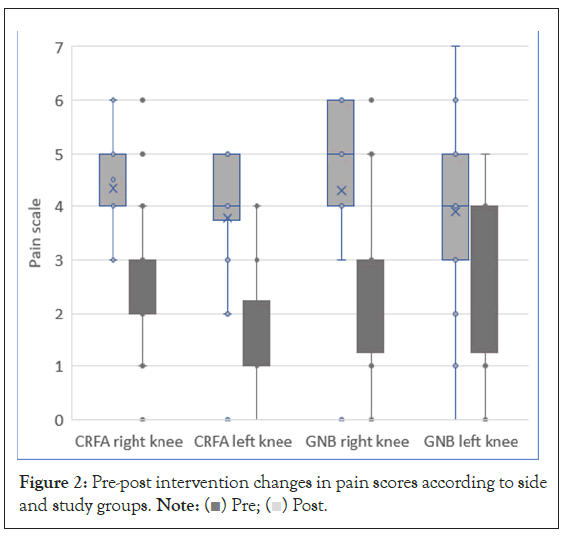
Figure 2: Pre-post intervention changes in pain scores according to side
and study groups. Note: ( ) Pre; (
) Pre; ( ) Post.
) Post.
Figure 3 displays the average duration of pain relief in months after the intervention. Pain relief lasted for a significantly longer duration in CRFA patients (mean ± SD; 6.8 ± 4.61 months) than in GNB patients (2.9 ± 1.17 months) (p<0.05).
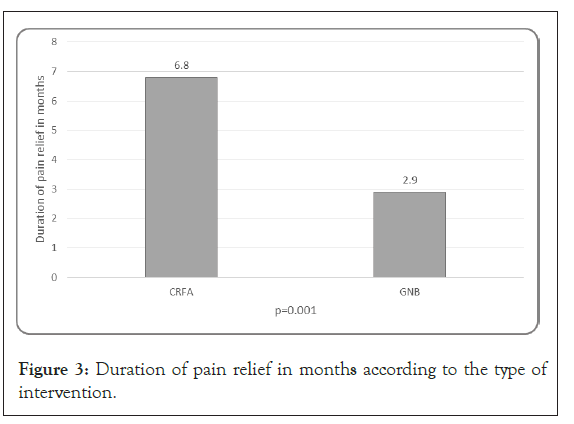
Figure 3: Duration of pain relief in months according to the type of intervention.
None of the patients in either group reported any post procedure complications such as muscle weakness, paresthesia, or neuralgia.
Discussion
The main finding of our study is the comparative effect of both CRFA and GNB on pain reduction and function improvement, but with a significantly longer duration of effect of CRFA. The ability of CRFA to decrease pain and improve daily function in patients with OA of the knee has been well established in previously published studies [16,17]. Qudsi-Sinclair et al. reported a reduction in pain and improvement of function during the first 3-6 months in patients with chronic pain post total knee arthroplasty, using both the conventional RFA of genicular nerves and GNB with local anesthetic and steroid [8]. However, we reported a longer duration of pain relief in the CRFA group, which might be related to bigger lesion size resulting from CRFA, documented in a previously published study [20].
In contrary to conventional radiofrequency, CRFA is a novel technology that utilizes thermal ablative mechanisms to create a greater neuronal lesion and increase the chance of effective denervation [21]. The effectiveness and safety of CRFA in relieving pain and improving function in patients with symptomatic knee OA has been demonstrated in a randomized clinical trial [17,21].
In several systematic reviews and meta-analyses, the addition of steroids to local anesthetic agents during peripheral nerve blockade provided a better quality of postoperative analgesia and lower pain scores [22-24].
Carlone et al. reported that patients with self-reported psychological comorbidities, smoking history, and diabetes mellitus were significantly more likely to not respond to GNB. They suggested that these failures are not related to technical factors, but rather patient-specific peripheral and central pain processing [25]. This is in conflict with the finding of our study in which patients with diabetes had a good response to GNB. Selection bias cannot be ruled out, particularly in studies with small sample sizes, which requires further studies for clarification.
Conclusion
Targeting the genicular nerve branches has had a profound clinical benefit in controlling knee osteoarthritic pain. Both CRFA and GNB are significantly effective in reducing pain and improving the function of knee OA; however, CRFA is superior to GNB regarding the duration of pain relief. Both techniques provide novel promising treatment options for patients not responding to conservative therapies and not suitable for surgical treatment.
Limitations of Study
The small sample size is one of the limitations of our study. Furthermore, power analysis was not performed as we could not estimate the prevalence of patients who would respond to the block or ablation. Despite these limitations, this is the first publication comparing CRFA to GNB among knee OA patients.
References
- Altman RD, Lozada CJ. Clinical features of osteoarthritis. In: Hochberg MC, Silman AJ, Smolen JS, Weinblatt ME, Weisman MH, editors. Rheumatology 4th ed. 2008;1703–1710.
- Cleveland RJ, Alvarez C, Schwartz TA, Losina E, Renner JB, Jordan JM, et al. The impact of painful knee osteoarthritis on mortality: A community-based cohort study with over 24 years of follow-up. Osteoarthr Cartil. 2019;27(4):593-602.
[Crossref] [Google Scholar] [Pub Med]
- Arroll B, Goodyear-Smith F. Corticosteroid injections for osteoarthritis of the knee: Meta-analysis. BMJ. 2004;328(7444):869.
- Conrozier T, Jerosch J, Beks P, Kemper F, Euller-Ziegler L, Bailleul F, et al. Prospective, multi-center, randomized evaluation of the safety and efficacy of five dosing regimens of viscosupplementation with hylan GF 20 in patients with symptomatic tibio-femoral osteoarthritis: A pilot study. Arch Orthop Trauma Surg. 2009;129(3):417-423.
[Crossref] [Google Scholar] [Pub Med]
- Raynauld JP, Buckland-Wright C, Ward R, Choquette D, Haraoui B, Martel-Pelletier J, et al. Safety and efficacy of long-term intraarticular steroid injections in osteoarthritis of the knee: A randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2003;48(2):370-377.
[Crossref] [Google Scholar] [Pub Med]
- Jevsevar DS, Jones DL, Matzkin EG, Manner PA, Mooar P, Schousboe JT. Treatment of osteoarthritis of the knee: Evidence based guideline 2nd Edition. American academy of orthopaedic surgeons. 2013;95(20):1885-1886.
- Ikeuchi M, Ushida T, Izumi M, Tani T. Percutaneous radiofrequency treatment for refractory anteromedial pain of osteoarthritic knees. Pain Med. 2011;12(4):546-551.
[Crossref] [Google Scholar] [Pub Med]
- Qudsi-Sinclair S, Borrás-Rubio E, Abellan-Guillén JF, Padilla del Rey ML, Ruiz-Merino G. A comparison of genicular nerve treatment using either radiofrequency or analgesic block with corticosteroid for pain after a total knee arthroplasty: A double-blind, randomized clinical study. Pain Pract. 2017;17(5):578-588.
[Crossref] [Google Scholar] [Pub Med]
- Patel N. Twelve-month follow-up of a randomized trial assessing cooled radiofrequency denervation as a treatment for sacroiliac region pain. Pain Pract. 2016;16(2):154-167.
[Crossref] [Google Scholar] [Pub Med]
- Stelzer W, Aiglesberger M, Stelzer D, Stelzer V. Use of cooled radiofrequency lateral branch neurotomy for the treatment of sacroiliac joint-mediated low back pain: A large case series. Pain Med. 2013;14(1):29-35.
[Crossref] [Google Scholar] [Pub Med]
- Johansson A, Hao J, Sjölund B. Local corticosteroid application blocks transmission in normal nociceptive C-fibres. Acta Anaesthesiol Scand. 1990;34(5):335-338.
[Crossref] [Google Scholar] [Pub Med]
- An K, Elkassabany NM, Liu J. Dexamethasone as adjuvant to bupivacaine prolongs the duration of thermal antinociception and prevents bupivacaine-induced rebound hyperalgesia via regional mechanism in a mouse sciatic nerve block model. PLoS One. 2015;10(4):e0123459.
[Crossref] [Google Scholar] [Pub Med]
- Ho KY, Hadi MA, Pasutharnchat K, Tan KH. Cooled radiofrequency denervation for treatment of sacroiliac joint pain: Two-year results from 20 cases. J Pain Res. 2013;6:505-511.
[Crossref] [Google Scholar] [Pub Med]
- Desai MJ, Kapural L, Petersohn JD, Vallejo R, Menzies R, Creamer M, et al. Twelve-month follow-up of a randomized clinical trial comparing intradiscal biacuplasty to conventional medical management for discogenic lumbar back pain. Pain Med. 2017;18(4):751-763.
[Crossref] [Google Scholar] [Pub Med]
- Kapural L, Vrooman B, Sarwar S, Krizanac-Bengez L, Rauck R, Gilmore C, et al. Radiofrequency intradiscal biacuplasty for treatment of discogenic lower back pain: A 12-month follow-up. Pain Med. 2015;16(3):425-431.
[Crossref] [Google Scholar] [Pub Med]
- Oladeji LO, Cook JL. Cooled radio frequency ablation for the treatment of osteoarthritis-related knee pain: Evidence, indications, and outcomes. J Knee Surg. 2019;32(01):65-71.
[Crossref] [Google Scholar] [Pub Med]
- Menzies RD, Hawkins JK. Analgesia and improved performance in a patient treated by cooled radiofrequency for pain and dysfunction postbilateral total knee replacement. Pain Pract. 2015;15(6):54-58.
[Crossref] [Google Scholar] [Pub Med]
- Yasar E, Kesikburun S, Kılıç C, Güzelküçük Ü, Yazar F, Tan AK. Accuracy of ultrasound-guided genicular nerve block: A cadaveric study. Pain Physician. 2015;18:899-904.
[Crossref] [Google Scholar] [Pub Med]
- Guermazi M, Poiraudeau S, Yahia M, Mezganni M, Fermanian J, Elleuch MH, et al. Translation, adaptation and validation of the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) for an Arab population: The Sfax modified WOMAC. Osteoarthritis Cartilage. 2004;12(6):459-468.
[Crossref] [Google Scholar] [Pub Med]
- Lorentzen T. A cooled needle electrode for radiofrequency tissue ablation: Thermodynamic aspects of improved performance compared with conventional needle design. Acad Radiol. 1996;3(7):556-563.
[Crossref] [Google Scholar] [Pub Med]
- Rojhani S, Qureshi Z, Chhatre A. Water-cooled radiofrequency provides pain relief, decreases disability, and improves quality of life in chronic knee osteoarthritis. Am J Phys Med Rehabil. 2017;96(1):5-8.
[Crossref] [Google Scholar] [Pub Med]
- de Oliveira GS, Castro Alves LJ, Nader A, Kendall MC, Rahangdale R, McCarthy RJ. Perineural dexamethasone to improve postoperative analgesia with peripheral nerve blocks: A meta-analysis of randomized controlled trials. Pain Res Treat. 2014;2014:179029.
[Crossref] [Google Scholar] [Pub Med]
- Albrecht E, Kern C, Kirkham KR. A systematic review and meta-analysis of perineural dexamethasone for peripheral nerve blocks. Anaesthesia. 2015;70(1):71-83.
[Crossref] [Google Scholar] [Pub Med]
- Knezevic NN, Anantamongkol U, Candido KD. Perineural dexamethasone added to local anesthesia for brachial plexus block improves pain but delays block onset and motor blockade recovery. Pain Physician. 2015;18(1):1-14.
[Crossref] [Google Scholar] [Pub Med]
- Carlone AG, Grothaus O, Jacobs C, Duncan ST. Is cooled radiofrequency genicular nerve block and ablation a viable option for the treatment of knee osteoarthritis? Arthroplast Today. 2021;7:220-224.
[Crossref] [Google Scholar] [Pub Med]
Citation: Khojah S, Mitwali E, AlAhdal O, Kaki A (2023) Comparison of Cooled Radiofrequency Ablation and Genicular Nerve Blockade for the Treatment of Osteoarthritic Knee Pain: A Prospective Randomized Double-Blind Study. J Pain Manage Med. 9:190.
Copyright: © 2023 Khojah S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

