Indexed In
- Open J Gate
- Cosmos IF
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
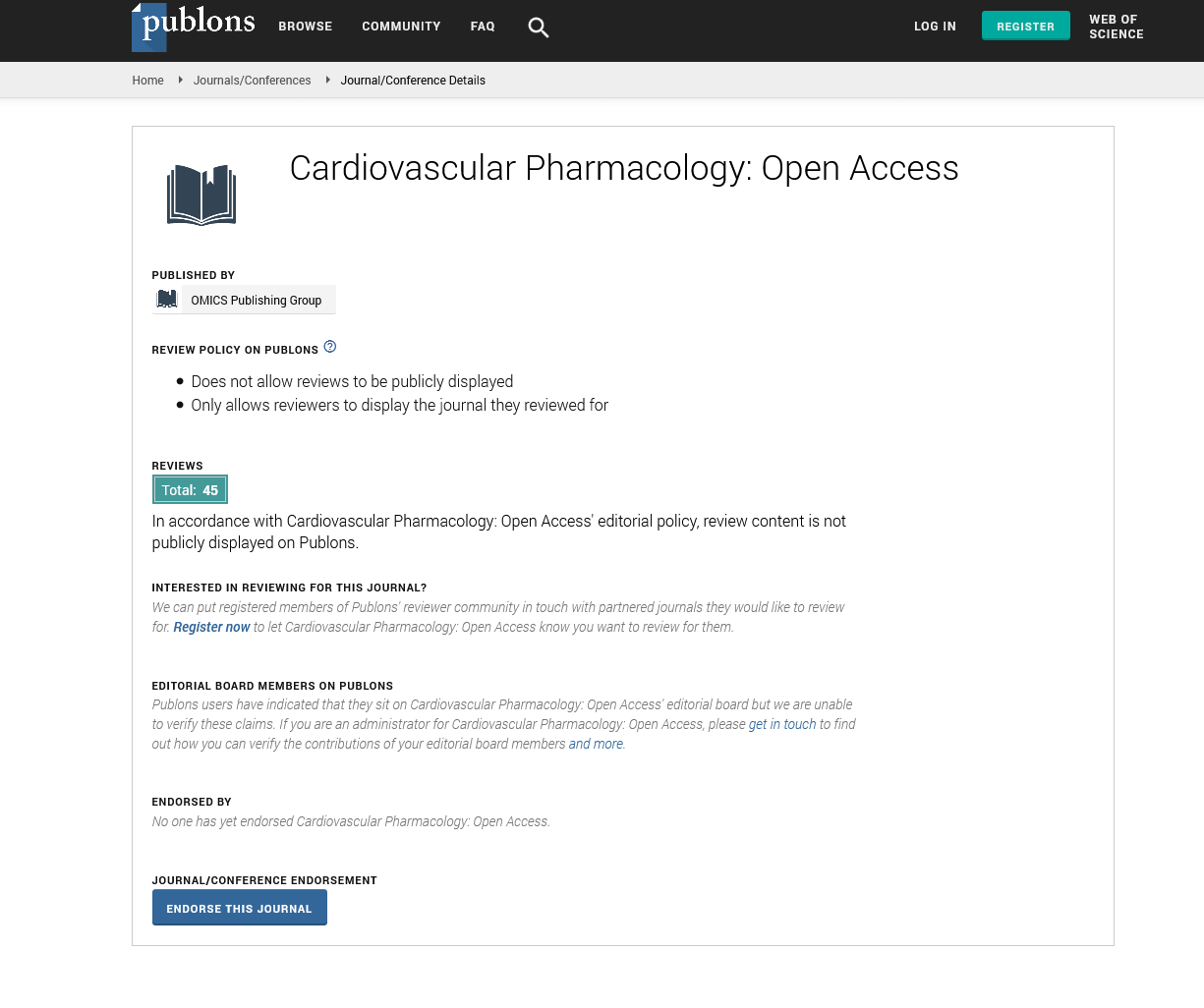
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
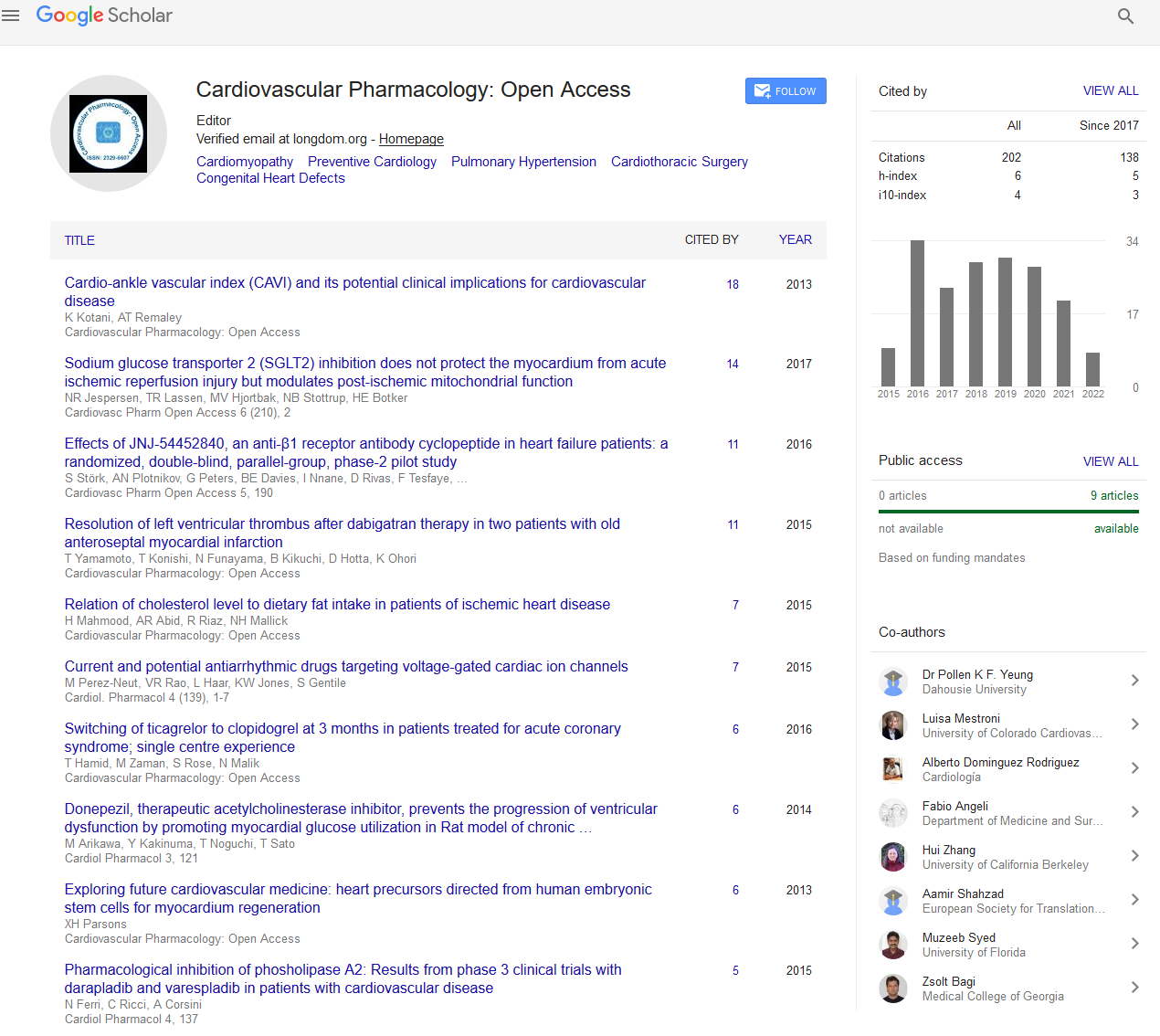
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Commentary - (2022) Volume 11, Issue 4
Cardiac Arrest Management in the Postoperative Cardiac Surgery Patients
Gregory Davies*Received: 05-Apr-2022, Manuscript No. CPO-22-16554; Editor assigned: 08-Apr-2022, Pre QC No. CPO-22-16554 (PQ); Reviewed: 22-Apr-2022, QC No. CPO-22-16554; Revised: 29-Apr-2022, Manuscript No. CPO-22-16554 (R); Published: 06-May-2022, DOI: 10.35248/2329-6607.22.11.277
Description
The rate of perioperative cardiac arrest following open-heart surgery ranges from 0.7% to 2.9% and has decreased in recent years. The discharge survival rates for these patients, although higher than in other hospital settings, are variable, ranging from 17% to 79%. Extracorporeal Life Support (ECPS), to improve survival during Cardiopulmonary Resuscitation (CPR), was introduced more than three decades ago by Mattox and Beall. To be effective, ECPS must be initiated early, as the results of CPR lasting more than 10 minutes are dismal [1].
• Usually precedes physiological deterioration, but may occur in previously stable patients.
• There are often discrete causes such as compression, hypovolemia, myocardial ischemia, tension pneumothorax, or pacing failure.
• Survival rate is about 80%.
• Urgent vein ablation should be an integral part of the discontinuation procedure until the 10th day after surgery.
To perform surgery, the patient is usually placed with a "pump" or Cardiopulmonary Bypass (PCP). This involves shrinking the right atrium and aorta (and subsequently aortic cross clamping), allowing all cardiac output to pass through the patient's heart and lungs. Blood flow is maintained using a pump and the blood is oxygenated through an integrated membrane oxygenator in the vessel. Several myocardial-sparing techniques are used to protect the heart from ischemic damage during this time. Cardiac arrest is induced using a hyperkalemia solution to induce asystole and thereby reduce myocardial metabolism and oxygen consumption. The heart is usually cooled. Patients are also usually cooled to less than 32°C to minimize peripheral oxygen consumption [2].
While at the pump, the patient's blood pressure and cardiac output are monitored by the perfusionist and also by the anesthesiologist using a vasopressor and vasodilator. During this time, patients should be anticoagulated with heparin systemically up to an ACT > 400 to prevent branch vessel coagulation. Prolonged pumping time is associated with increased postoperative complications such as bleeding, myocardial shock, and multiple organ failure. CPB also appears to be involved in the onset of Systemic Inflammatory Response Syndrome (SIRS). Sometimes it is difficult to release the patient from CPB or “get them off the pump”. That is, to restart the heart by contracting normally. Squeeze parts or fasteners are often used to help "get out of the pump [3].
The resident must be present in the ICU when the patient arrives from the operating room to be signed by the anesthesiologist and the cardiac surgery team. During this phase, ICU nurses will transfer the patient to the ICU monitors and check all lines and fluids. The nurse will then perform the initial hemodynamic settings. The respiratory technician will place the patient on a ventilator.
Intensive care patients are closely monitored and are often intubated and mechanically ventilated. Therefore, the possibility of cardiac arrest is most likely signalled by monitoring alarm devices. If you are the first to be alerted to the possibility of arrest, you should immediately place your hand on the central pulse (such as the femoral or carotid pulse) for up to 10 seconds. During this time, you should also check the location of the blood vessels and observe other traces on the monitor. During cardiac arrest, not only the arterial line is not pulsating, but the Central Venous Pressure (CVP) line, pulse dosimeter monitoring, and Pulmonary Artery Pressure (PAP) monitoring will also be problems. An ECG trace similar to sinus rhythm in the absence of other monitor impulses should be considered cardiac arrest [4].
• Once the arrest is established, a person will be assigned to the ECM. This should be started immediately at 100/min while monitoring the arterial fistula to assess effectiveness. The only exception to this rule is when defibrillation or pacing is appropriate before the ECM.
• Oxygen should be increased to 100% and the airway and breathing rate checked with each course, especially to rule out pneumothorax, pneumothorax, or endotracheal tube problem.
• Defibrillators should be connected and shock administered if necessary. This person should also verify pacing and, if an emergency veinectomy is to be performed, should ensure that an internal defibrillator is available and connected at all times.
• This person stops all IVs and syringes and uses atropine, amiodarone, and other medications as needed.
Senior ICU staff coordinating peripheral operations at the patient's bedside. This includes preparing for a possible amputation as soon as an arrest warrant is issued, managing available additional staff, and calling for specialist assistance if not immediately available during the operation. Meanwhile continuously reporting progress to the team leader.
Post-resuscitation care includes multidisciplinary teamwork focused on cardiopulmonary stabilization, identification of CA Etiology, neuroprotection, and prevention of CA recurrence. Initial neurological evaluation after ROSC is clinical and is repeated frequently taking into account the presence of sedation and hypothermia. Initial neurological examination includes: GCS score (modified GCS for intubated patients), pupillary response to light, corneal reflexes, and presence of seizures. Patients who did not achieve complete neurological recovery were initially managed with hypothermic therapy. Neurological prognosis (for comatose patients) using the Brain Performance Classification (CPC) scale was performed 72 h after ROSC and repeated daily [5].
REFERENCES
- Mackay JH, Powell SJ, Osgathorp J, Rozario CJ. Six-year prospective audit of chest reopening after cardiac arrest. European Journal of Cardio-Thoracic Surgery. 2002;22(3):421-425.
- Birdi I, Chaudhuri N, Lenthall K, Reddy S, Nashef SAM. Emergency reinstitution of cardiopulmonary bypass following cardiac surgery: outcome justifies the cost. European Journal of Cardio-Thoracic Surgery. 2000;17(6):743–746.
- Arntz HR, Bossaert L, Filippatos GS. European Resuscitation Council guidelines for resuscitation 2005. Section 5. Initial management of acute coronary syndromes. 2005;67(1):S87-S96.
- Biarent D, Bingham R, Richmond S, Maconochie I, Wyllie J, Simpson S, et al. European R.C. European Resuscitation Council guidelines for resuscitation. Section 6. Paediatric life support, Resuscitation. 2005; 67(1):S97-S133.
- Dunning J, Fabbri A, Kolh PH. Guideline for resuscitation in cardiac arrest after cardiac surgery. European journal of cardio-thoracic surgery. journal of the European Association for Cardio-thoracic Surgery. 2009:36(1):3-28.
Citation: Davies G (2022) Cardiac Arrest Management in the Postoperative Cardiac Surgery Patients. Cardiovasc Pharm. 11:277.
Copyright: © 2022 Davies G. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.