Indexed In
- Open J Gate
- Genamics JournalSeek
- ResearchBible
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
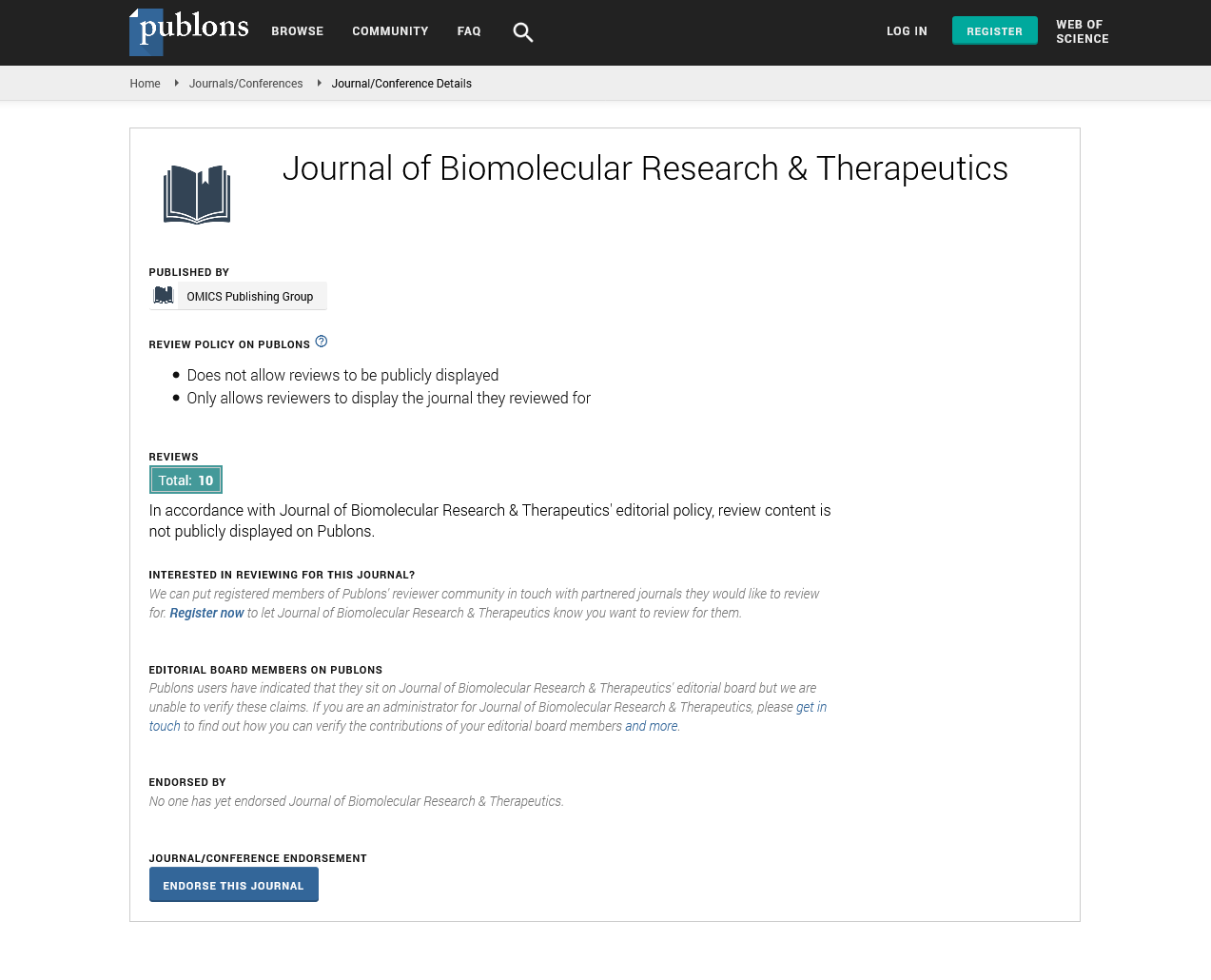
- Publons
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Opinion Article - (2025) Volume 14, Issue 3
Biomarkers in Early Detection and Treatment Monitoring
Rachel Johnson*Received: 29-May-2025, Manuscript No. BOM-25-29600; Editor assigned: 31-May-2025, Pre QC No. BOM-25-29600; Reviewed: 14-Jun-2025, QC No. BOM-25-29600; Revised: 20-Jun-2025, Manuscript No. BOM-25-29600; Published: 28-Jun-2025, DOI: 10.35248/2167-7956.25.22.445
Description
Biomarkers are measurable indicators of biological activity that play a crucial role in the early detection of diseases and in tracking treatment effectiveness. By providing objective and quantifiable data, they supplement clinical assessments and inform decisions related to diagnosis, prognosis and therapy. In oncology, biomarkers have revolutionized early cancer detection and patient classification. Specific molecular markers, such as HER2 in breast cancer and EGFR mutations in lung cancer, guide the use of targeted therapies, ensuring treatments are tailored to the patient’s specific tumour profile. In addition, liquid biopsies, which detect circulating tumour DNA in blood, are emerging as non-invasive tools to diagnose cancer in its early stages and to monitor treatment response. In cardiovascular medicine, biomarkers are equally impactful. Cardiac troponins are the gold standard for diagnosing heart attacks, while natriuretic peptides like BNP are essential in assessing and managing heart failure. These biomarkers enable prompt diagnosis and timely medical intervention, thereby improving patient outcomes. Advances in fields like proteomics and metabolomics are continually uncovering novel biomarkers with the potential to refine cardiovascular disease management even further.
Neurological conditions such as Alzheimer’s disease, Parkinson’s disease and multiple sclerosis are also seeing rapid progress in biomarker research. For example, elevated or abnormal levels of amyloid-beta and tau proteins in cerebrospinal fluid serve as early indicators of Alzheimer’s, often before symptoms manifest. Imaging biomarkers, including PET scans that visualize amyloid plaque deposition, are also being used to monitor disease progression and evaluate treatment effectiveness. Early detection of neurodegenerative conditions through such biomarkers opens the door for earlier therapeutic interventions, potentially delaying or mitigating disease progression. In drug development, biomarkers are becoming indispensable tools for evaluating not only the safety and effectiveness of medications but also for optimizing treatment strategies. Pharmacodynamics biomarkers, which monitor the biological effects of a drug on its target, provide crucial feedback on how well a treatment is working at a molecular level. For example, in cancer therapy, markers that track tumour shrinkage or changes in biomarkers like circulating tumour DNA (ctDNA) can directly indicate how a patient is responding to chemotherapy, immunotherapy, or targeted therapy. This helps clinicians make timely adjustments to treatment regimens, ensuring that patients receive the most effective care throughout the course of their treatment.
Predictive biomarkers go one step further by identifying patients who are likely to respond favourably to specific therapies. These biomarkers can assess genetic or molecular features that make certain treatments more or less effective for an individual. A notable example is the use of genetic testing to detect mutations in the EGFR gene in lung cancer patients. If a patient is found to have an EGFR mutation, targeted therapies like Tyrosine Kinase Inhibitors (TKIs) can significantly improve outcomes compared to traditional chemotherapy. This form of precision medicine tailors therapy based on the patient's unique genetic makeup, reducing unnecessary side effects and increasing the likelihood of treatment success. While biomarkers hold immense potential in advancing personalized medicine, there are significant challenges that still hinder their widespread clinical adoption. One major obstacle is the lack of standardized testing methods. For biomarkers to be used reliably in clinical settings, consistent and reproducible testing protocols are necessary. Variability in laboratory techniques, differences in patient demographics and biological diversity among individuals can all lead to discrepancies in biomarker measurement, which could ultimately affect treatment outcomes. Standardizing these tests across different healthcare systems and ensuring their reproducibility across diverse populations is a critical area of focus for researchers and regulatory agencies.
The complex nature of biomarkers also poses challenges in their validation. A biomarker must be rigorously tested to confirm that it accurately reflects disease presence or progression and is not influenced by other variables. This validation process often involves extensive clinical trials and collaborations between pharmaceutical companies, academic institutions and regulatory bodies to ensure that the biomarkers meet regulatory standards and can be used safely in clinical practice. Technological advancements continue to pave the way for more precise and effective biomarker applications. High-throughput sequencing technologies, for example, allow for the identification of a wide range of genetic alterations that might have previously gone undetected. Mass spectrometry and next-generation imaging techniques further enhance our ability to detect and analyse biomarkers at an unprecedented scale and resolution. As a result, biomarkers can now be utilized not only to diagnose diseases but also to predict treatment outcomes and monitor patients for signs of relapse or recurrence.
Looking forward, the future of biomarkers in clinical practice is extremely promising. As new biomarkers are discovered and validated, they will likely expand the scope of precision medicine, enabling doctors to detect diseases at even earlier stages and tailor treatments more effectively. Beyond cancer and cardiovascular diseases, biomarkers hold promise in fields such as autoimmune disorders, infectious diseases and rare genetic conditions, offering new avenues for targeted treatments and improved patient management. In conclusion, biomarkers represent a transformative force in the field of medicine. Their role in drug development and clinical care is rapidly expanding, offering a pathway toward more personalized, effective and efficient healthcare. With continued advancements in technology, data analysis and collaborative research, biomarkers are poised to shape the future of medicine, improving patient outcomes while also making healthcare more accessible and cost-effective globally.
Citation: Johnson R (2025). Biomarkers in Early Detection and Treatment Monitoring. 22:445
Copyright: © 2025 Johnson R. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.