Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- Google Scholar
- SHERPA ROMEO
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2020) Volume 8, Issue 7
Behçet Disease Revealed by an Isolated Brachial Artery Aneurysm
Sara Mokhtari1,2*, Oussama Anane1,2, Abdellah Rezziki1,2, Khalid Andaloussi Serraj1,3, Adnane Benzirar1,2 and Omar El Mahi1,22Vascular Surgery Department, Mohammed VI University Hospital Center, Oujda, Morocco
3Internal Medicine Department, Mohammed VI University Hospital Center, Oujda, Morocco
Received: 05-Oct-2020 Published: 27-Nov-2020, DOI: 10.35248/2329-6925.20.8.400
Abstract
Behçet disease is a vasculitis whose diagnosis is essentially clinical. It is often revealed by so-called bipolar oral and genital lesions. Those lesions are dominated by recurrent aphthous ulcerations. During this pathology, vascular involvement is mostly presented by venous thrombosis while arterial pathologies are rarely reported. Management of arterial aneurysms in patients with Behçet disease represent a serious challenge for the physicians as the posttreatment complications are heavy to handle. Through this case report, we aim to present a rare presentation of a young male patient diagnosed with Behçet disease revealed by an isolated brachial artery aneurysm.
Keywords
Aneurysm; Brachial artery; Behçet disease; Complications; Surgery
Introduction
Behçet Disease (BD) is a multisystemic inflammatory vasculitis of unknown etiology. Young men; in the Mediterranean, Middle East and Japan; are the mainly concerned. Venous lesions are the most frequent during this pathology while the arterial involvement is considered a serious complication with a grim prognosis. Treatment of this entity, in patients with BD, is a vexing problem which requires a frequent repetitive controls in order to detect eventual post-treatment complications and vascular diseases. Herein, we report a rare case of an isolated brachial artery aneurysm occurring in a young patient revealing BD.
Case Report
A 25 years old Moroccan man without pathological history was admitted to our vascular surgery consultation. The patient complained of a painful mass located in front of the axillary region associated with sensation of numbness and tingling in the ipsilateral limb. The anamnesis revealed that the swelling had a sudden onset and rapid development within just 4 days. The physical examination of the limb showed a 3 cm pulsatile and expansive mass at the level of the proximal tiers of the left arm (Figure 1). The sensitivity of the limb in the course of the median and ulnar nerves was reduced. The mobility of the upper limb was limited. The humeral, radial and ulnar pulses were well perceived and the limb was warm without signs of ischemia. No other aneurysmal localization was found. In addition, bipolar aphthoid lesions have been revealed at the examination of the genital and oral systems (Figure 2). Otherwise, there was no concept of family history plus the ophthalmic and neurological examination were without abnormalities.The radiological couple doppler ultrasound-angio -CT scan revealed a false aneurysm of brachial artery in its proximal part just after passing through the axillary fossa. The aneurysmal mass compressed essentially the median nerve which was partially invaded (Figure 3).
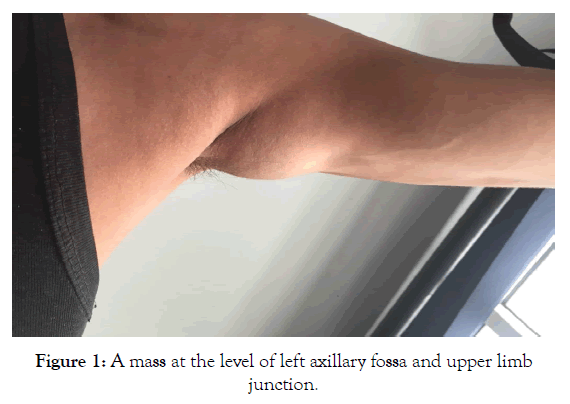
Figure 1: A mass at the level of left axillary fossa and upper limb junction.
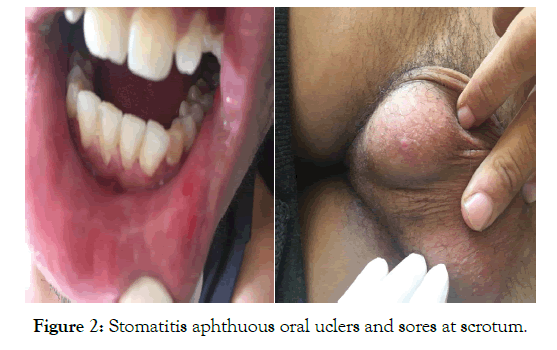
Figure 2: Stomatitis aphthuous oral uclers and sores at scrotum.
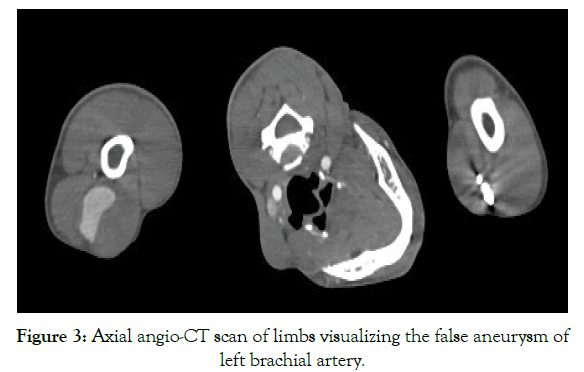
Figure 3: Axial angio-CT scan of limbs visualizing the false aneurysm of left brachial artery.
Along with these clinical data found (aphthous stomatitis and genital ulcers), biological test results (Leukocytes: 11130/ul;CRP: 30 mg/l; ESR: 65 mm; inflammatory state in serum protein electrophoresis test) and radiological aspect, the diagnosis of an active BD;revealed by an aneurysm of brachial artery; was retained. A rare location of arterial aneurysms in patients with BD.
Our management tactic was based on the actual clinical situation compromising the prognosis of the limb. Indeed, Behçet vasculitis was in its active phase complicated by an acute aneurysm of brachial artery compressing nerves associated with high risk of rupture. Thus, the patient was primarily put on corticosteroid therapy and antiplatelet for 3 days before performing the surgical treatment. The surgical repair consisted of the aneurysm excision and ensuring vascular continuity by means of a venous bypass taken from the great saphenous vein at the level of the ipsilateral thigh (Figure 4). Post-procedural course was simple and the histological result of the aneurysm returned in favor of BD. The patient was discharged under medical treatments at the 3rd day postoperatory. 3 weeks later, he was readmitted to the emergency room, for an infected false aneurysm at the axillary fossa, treated by resection of the false aneurysm and ligation of the humeral artery. No complications were objected at 12 months of follow-up.
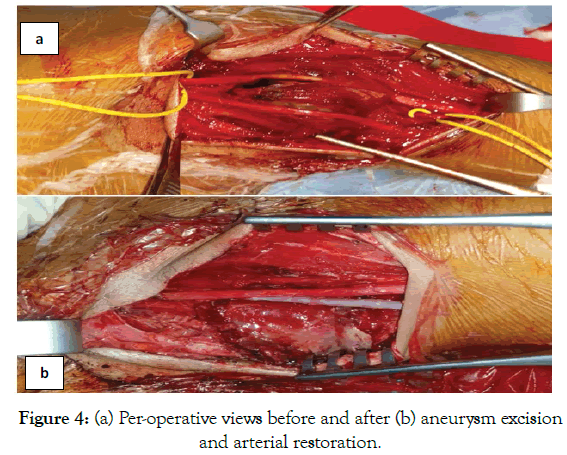
Figure 4:(a) Per-operative views before and after (b) aneurysm excision and arterial restoration.
Discussion
Been described for the first time in 1937 by Hulusi Behçet; a Turkish dermatologist; Behçet disease is defined as a chronic multi systemic inflammatory pathology. It is a vasculitis that may affect vessels from different sizes [1].The diagnosis is essentially established on clinical findings. A symptomatic triad is concerned pathognomonic, it includes recurrent oral and genital aphthuous ulcers, ocular manifestations and skin lesions.
Vascular involvement during BD is dominated by venous disorders represented by thromboembolic pathology while Arterial Aneurysms (AA), rather than occlusions, are uncommon [2,3] and it account for 10%-15% of the vascular complications [4]. The latter are the main cause of death since the principal arteries affected, by decreasing frequency, are the abdominal aorta followed by pulmonary and femoral arteries. Incrimination of other arteries is rare [5]. As for brachial artery involvement, only scanty case reports have been reported in the literature [6,7].
Otherwise, it has been noted that the interval period between the diagnosis of BD and the onset of arterial manifestation is about 5-9 years [8-10]. In other rare cases, the arterial complication may reveal BD. This was the case of our patient who was admitted for brachial artery aneurysm of a sudden onset associated with neuropathies in the ipsilateral limb. An exhaustive anamnesis and a munitious physical examination helped to exclude other etiologies (lipoma, traumatism, atherosclerosis…) and to orient towards BD etiology. As for radiological investigations, the Angio- CT scan permitted, in one hand, to guide the diagnosis of BD by visualizing a thickening arterial wall without calcifications, and in another hand to characterize the aneurysm (unique or multiple, true or false type, size, site, …) and its complications. Rupture is the main complication of arterial aneurysms [11]. The evolution towards this complication, during BD, is inevitable [12], aim of an early diagnosis of this devastating disease for an appropriate treatment to avoid fatal consequences.
AA treatment, in the context of BD, has dual purpose firstly cooling the systemic inflammatory disease and secondly resolving the arterial complication itself. For that it is necessary to administrate immunosuppressive therapy before and after AA management. This administration should benefit from adjustments in the dosage and duration of treatment [13]. Indeed, the instauration of steroid and immunosuppressive drugs before surgical repair of arterial aneurysms had shown beneficial post-operative outcomes [14]. In that sense, Desbois insists on the importance of operating these patients in "cold" phase that is to say after initiation of immunosuppressive therapy and with perioperative anticoagulation [15].
Treatment options of AA to date include surgical bypass and stent graft release. It has been set indications for open surgery including rupture or pre-rupture of the aneurysm, acute ischemia or neuropathy of the homolateral limb and rapid increase in aneurysm size. Despite positive aspects of surgical option, it has also soma negatives such anastomosis complications, suture line dehiscence, bypass occlusion or infection, development of new aneurysms and thromboembolic events [5,16,17]. Otherwise, it has been reported that aneurysms at the level of brachial and axillary arteries are associated with high risk of blood loss and neurological incidents [18,19].
High rates of pseudo-aneurysm complications of anastomotic sites have been observed. Therefore, several authors turned to the use of endovascular therapeutic option. Kim et al. propose endovascular treatment as a valid alternative in the management of BD arterial complications [12]. The use of stent grafts has proved to be effective and safe as it induces less pseudoaneurysms than conventional surgery. (14.3%-22.2% versus 30%-50%) [20-22], in addition, it has a much higher survival rate [23,24]. Although these excellent results and its recent widespread use, the current experience with endovascular treatment in this entity remains a limiting factor for definitive conclusions and requires large case series and prospective multicenter studies to confirm or deny the utility of this therapeutic option in long term.
Conclusion
AA in BD patients is a limb and life threatening condition. Even with proper treatment, the prognosis is bad.Increasing awareness by early detection of this pathology is mandatory in order to prompt treatment with immunosuppressive drugs to improve the disease outcome.
Conflicts of interests: All authors affirm they have no conflict of interests and there were no financial support for this work.
Informed consent: Consent was obtained from patient who participated in this study.
REFERENCES
- Lie J. Vascular involvement in Behçet’s disease: Arterial and venous and vessels of all sizes. J Rheumatol. 1992;19(3):341-343.
- Shuang Li, Ai-Jun Chen, Kun Huang, Hui Li. Successful Treatment of Vasculor Behcet’s Disease Presenting as Recurrent Pseudoaneurysms: The Importance of Medical Treatment. Dermatol Ther. 2013;3(1):107-112.
- Kwon TW, Park SJ, Kim HK, Yoon HK, Kim GE, Yu B. Surgical treatment result of abdominal aorticaneurysm in Behçet’sdisease. Eur J Vasc Endovasc Surg. 2008;35:173-180
- Watanabe H, Oda H, Yoshida T, Yamaura M, Takahashi K, Miida T, et al. Endovascular stent-grafting for recurrent aneurysm in Behcet's disease. Int Heart J. 2005;46(4):745-749.
- Calamia KT, Schirmer M, Melikoglu M. Major vessel involvement in Behcet’s disease: an update. Curr Opin Rheumatol. 2011;(1):24-31.
- Robbs JV, Naidoo KS. Nerve compression injuries due to traumatic false aneurysm. Ann Surg. 1984;200:80-82.
- Kemp K, Radwan R, Shingler G, Davies C. Brachial arterypseudoaneurysm. BMJ Case Rep. 2014.
- Hamza M. Large artery involvement in Behcet’s disease. J Rheumatol 1987;14:554e9.
- Le ThiHuong D, Wechsler B, Papo T, Piette JC, Bletry O, Vitoux JM, et al. Arteriallesions in Behcet’s disease. A studyin 25 patients. J Rheumatol 1995;22:2103e13.
- Kural-Seyahi E, Fresko I, Seyahi N, Ozyazgan Y, Mat C, Hamuryudan V, et al. The long-termmortality and morbidity of Behcet syndrome: a 2-decade outcomesurvey of 387 patients followedat a dedicated center. Medicine 2003;82:60e76.
- Zhang SH, Zhang FX. Behcet's disease with recurrent thoracic aortic aneurysm combined with femoral artery aneurysm: A case report and literature review. J Cardiothoracic Surgery 2017;12:79.
- Freyrie A, Paragona O, Cenacchi G, Pasquinelli G, Guiducci G, Faggioli GL. True and false aneurysms in Behcet’ s disease: case report with ultrastructural observations. J Vasc Surg 1993;17:762-767.
- Kim SW, Lee DY, Kim MD, Won JY, Park SI, Yoon YN, et al. Outcomes of endovascular treatment for aortic pseudo aneurysm in Behcet’s disease. J Vasc Surg 2014;59:608-614.
- Hasanaghaei T, GhoddusiJohari H, Shenavandeh S. Huge femoral artery pseudoaneurysm in a patient with Behçet’s disease. Egypt Rheumatol 2017;39:267-270
- Desbois A-C, Wechsler B, Cluzel P, Helft G, Boutin D, Piette JC, et al. Atteintes cardiovasculaires de la maladie de Behcet. Rev Med Interne 2014;35:103-111.
- Mercan S, Sarigul A, Koramaz I, Demirturk O, Boke E. Pseudoaneurysm formation in surgically treated Behçet's syndrome-a case report. Angiology 2000;51:349e53.
- Schneider F, Gouny P, Van Laere O, Duedal V, Nussaume O. Vascular complications after surgical repair of aneurysms in Behcet’s disease. J Cardiovasc Surg 2002;43:501e5.
- Kristen R, Schmitz-Rixen T, Huber P, Erasmi H. Aneurysm of the brachial artery- a rare complication of Behçet disease: Case report. Vasa. 1988;17(3):229-232.
- Aggarwal A, Dabadghao S, Roy S, Agarwal S, Misra R. Brachial artery aneurysm and peripheral gangrene in a patient with Behçet disease. Clin Exp Rheumatol. 1993;11(5):579-580.
- Liu CW, Ye W, Liu B, Zeng R, Wu W, Dake MD. Endovascular treatment of aortic pseudo aneurysm in Behcet’s disease. J Vasc Surg 2009;50:1025-1030.
- Park JH, Chung JW, Joh JH, Song SI, Shin SJ, Chung KS, et al. Aortic and Arterial Aneurysms in Behçet Disease: Management with Stent-Grafts—Initial Experience. Radiology 2001;220:745-750.
- Kwon koo B, Shim WH, Yoon YS, Kwon Lee B, Choi D, Jang Y, et al. Endovascular therapy combined with immunosuppressive treatment for pseudoaneurysms in patients with Behçet's disease. J Endovasc Ther 2003;10:75-80.
- Kasirajan K, Marek JM, Langsfeld M. Behçet's disease: endovascular management of a ruptured peripheral arterial aneurysm. J Vasc Surg 2001;34:1127e9.
- Kim WH, Choi D, Kim JS, Ko YG, Jang Y, Shim WH. Effectiveness and safety of endovascular aneurysm treatment in patients with vasculo-Behçet disease. J Endovasc Ther 2009;16(5):631e6.
Citation: Mokhtari S, Anane O, Rezziki A, Serraj KA, Benzirar A, El Mahi O (2020) Behçet Disease Revealed by an Isolated Brachial Artery Aneurysm. J Vasc Med Surg. 8:400
Copyright: © 2020 Mokhtari S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

