Citations : 2345
Dentistry received 2345 citations as per Google Scholar report
Indexed In
- Genamics JournalSeek
- JournalTOCs
- CiteFactor
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2023) Volume 13, Issue 5
Attitude of the Dental Staff towards Radiation Safety in Georgia-Radiation Protection of Patients and Staff
Ana Maisuradze1,2*, Ketevan Kiguradze-Gogilashvili3,4, Flavien Fettak5, Zurab Alkhanishvili6,7, Ketevan Oghiashvili8, Madona Akhobadze9 and David Nadareishvili102Selarl IMAGIX, Radiological Center, Tourcoing, France
3Department of Therapeutic Dentistry, Ivane Javakhishvili Tbilisi State University, Chavchavadze Ave. Tbilisi, Georgia
4Georgian Dental Association, Tbilisi, Georgia
5Department of Dentistry, “Dental center”, Mouvaux, France
6Department of Public Health, UNA Georgia, Tbilisi, Georgia
7Department of Dentistry, “Albius” Dental Center, Tbilisi, Georgia
8Department of Dentistry, “Odontos” Dental Center, Tbilisi, Georgia
9Department of Neuroscience, Georgian-Dutch Hospital, Tbilisi, Georgia
10Beritashvili Center of Experimental Biomedicine, Tbilisi, Georgia
Received: 19-Sep-2023, Manuscript No. DCR-23-23113; Editor assigned: 22-Sep-2023, Pre QC No. DCR-23-23113 (PQ); Reviewed: 06-Oct-2023, QC No. DCR-23-23113; Revised: 13-Oct-2023, Manuscript No. DCR-23-23113 (R); Published: 20-Oct-2023, DOI: 10.35248/2161-1122.23.13.659
Abstract
Objectives: Dentists use radiographic imaging methods in the diagnosis and treatment of dental diseases, more often than any other health professional, but exposure to ionizing radiation does not come without risk. The aim of this study was to survey the attitude of Georgian operators (dentists, dental assistants, radiographers and other medical staff) regarding oral radiology safety standards.
Methods: 402 questionnaires were given to dental staff working in different dental clinics in Tbilisi, who perform dental intraoral imaging. The participants were asked about radiation protection of patients and dental staff, attitudes and behaviors regarding radiation protection. The questionnaire also included questions about the socio- demographic characteristics of the participants and management of radiographic waste. Descriptive statistics of data were performed using the Statistical Package for the Social Sciences (SPSS) software program.
Results: Only 39.43% of the participants followed radiation protection and radiation safety course. 26.76% of operators use the position and distance rules correctly for their own protection. 39.43% of operators always take their dosimeters. 25.36% of the patients hold imaging receptors with hand during intraoral radiography procedure. 61.97% of professionals hold imaging receptors with their own hand and only 12.68% of professionals use film holder. 73.24% of practitioners use the same exposure parameters for adult and pediatric patients. 35.21% of operators use lead aprons and 32.39% of operators use thyroid collar for their patients during exposition. 26.76% of participants maintain exposure history. 67.61% of cases traceability of X-ray dose is not performed. 71.83% of participants don’t keep any X-ray source quality control management Journal.
Conclusion: The present study has revealed a lack of knowledge on the part of dental staff about the rules and guidelines for the practice of radiology and radioprotection, emphasizing the need for operators to improve their knowledge. There is a definite need to reinforce the importance of radiation protection in the dental curriculum in Georgia.
Keywords
Radiation protection; Ionizing radiation; Dental imaging; Safety; Georgia
Introduction
Dentists use radiographic imaging methods in the diagnosis and treatment of dental diseases, more often than any other health professional [1]. A report by the European Commission estimates that dental X-ray procedures make up 32% of all plain radiography procedures in Europe, with a mean value of 352 dental procedures per 1000 population per year [2,3]. There are three basic principles of radiation protection: justification, optimization, and dose limitation. All diagnostic imaging should adhere to these three principles [3]. All radiation exposure must be based on the principle ALARA (As Low As Reasonably Achievable). In 2014, at the National Council on Radiation Protection and Measurements (NCRP) USA Annual Meeting, Bushberg introduced the term ALADA (As Low As Diagnostically Acceptable) as a variation of the acronym ALARA to stress the value of optimization in medical imaging, which means that the radiograph should be of acceptable diagnostic quality, with the minimum dose to the patient [4]. Radiology in dentistry has significant diagnostic benefits when indicated and used appropriately, but exposure to ionizing radiation does not come without risk [5]. Intraoral or extraoral radiography procedures used in dentistry yield relatively lower radiation doses to patients. However, there is still a risk of the development of stochastic effects due to these imaging procedures [6]. Stochastic effects are thought to have no dose threshold for occurrence (the ‘linear, non-threshold theory’). The probability of occurrence of stochastic effects is considered to be proportional to the imparted dose, no matter how low the dose might be. The probability of occurrence of stochastic effects is assumed to be additive and is proportional to the dose, whereas the severity of the damages does not depend on the amount of imparted dose [3]. Biological damage to Deoxyribonucleic Acid (DNA) directly or indirectly may give rise to a risk of cancer. The anatomic position and the relatively high radiosensitivity of the thyroid gland make it an organ of concern in dental radiography. Given the high lifetime prevalence and frequency of exposure to dental X-rays, even a small increase in thyroid cancer risk would be of considerable public health importance [7]. Dental radiography during pregnancy is associated with low birth weight, specifically with term low birth weight [8]. The greatest risk to the fetus for chromosomal abnormalities and subsequent mental retardation is between 8 and 15 weeks of pregnancy [9]. The knowledge of radiation safety and the behavior of dental staff can affect patients’ exposure to radiation. Lead aprons reduce 98% of scattered radiation and thyroid collar attenuate 92% of scattered radiation. So, it should be made mandatory to use thyroid collars and lead aprons before any exposure. Film holders avoid unnecessary exposure to the patient’s fingers. Patient’s exposure history must be maintained and updated after every exposure. Each operator has a responsibility to justify medical exposure and to optimize the radiation protection of patients. Dental staff should follow radiation protection and radiation safety principles as long as they keep up their profession. In 2014, Georgia enacted a new law of ‘Nuclear and radiation safety’, which was adopted in order to provide consistency with the new International and European Radiation Basic Safety Standards (BSS) [10]. In Georgia dental radiography is performed by dentists or dental assistants and radiographers under the supervision of a dentist. In most dental institutions, dentists are responsible for radiography and radiation management. Georgian Dental Association (GSA) is committed to the training of dentists in the field of radiation protection. The annual Dental International Congress of Georgian Dental Association was held in Batumi and many dentists participated from different parts of the country. This year the congress program included radiation protection training. The aim of this study was to survey the attitude of Georgian operators (dentists, dental assistants, radiographers and other medical staff) regarding oral radiology safety standards.
Materials and Methods
Statistics plays an essential role in dental practice and research. This survey was carried out with dental staff (dentists, dental assistants, radiographers and other medical staff) working in different dental clinics in Tbilisi (Capital of Georgia).
A questionnaire with 15 questions was given to the dentists, dental assistants, radiographers and other medical staff who participate in dental intraoral imaging. To prepare this questionnaire a review of the literature was performed. We conducted this study in accordance with ethical standards and our questionnaire was validated by the Georgian Dental Association (GDA).
Eligibility criteria
In our study 402 questionnaires (Table 1), were given to the dental staff, who perform dental intraoral imaging (dentists, dental assistants, radiographers and other medical staff). A questionnaire including 15 questions was completely anonymous to give participants more freedom. The participants were asked about radiation protection of patients and dental staff, attitudes and behaviors regarding radiation protection. The questionnaire also included questions about the socio-demographic characteristics of the participants and the management of radiographic waste. The participants were asked to choose one between the options: Yes or No. While the correct attitude and behavior were given one point and the wrong one was given zero points.
| Questionnaire (Translated from Georgian) | Answers | Number of participants N % |
|---|---|---|
| Do you follow radiation protection and radiation safety course? | Yes | 39.43% |
| No | 60.37% | |
| Do you wear a lead apron when you are performing dental intraoral radiography? | Yes | 33.80% |
| No | 66.20% | |
| Do you wear a thyroid collar when you are performing dental intraoral radiography? | Yes | 30.98% |
| No | 69.02% | |
| Is there a barrier (shielding) between you and the X-ray source? | Yes | 26.76% |
| No | 73.24% | |
| Do you use a personal passive dosimeter when you are performing dental intraoral radiography? | Yes | 39.43% |
| No | 60.37% | |
| When you are performing dental intraoral radiography | Film holder | 12.68% |
| Patient’s hand | 25.35% | |
| Your own hand | 61.97% | |
| Do you give a leaded apron to the patient to wear before dental imaging? | Yes | 35.21% |
| No | 64.79% | |
| Do you give a thyroid collar to the patient to wear before dental imaging? | Yes | 32.39% |
| No | 67.61% | |
| Do you use the same parameters (kV. mA. s) for dental imaging of adult and pediatric patients? | Yes | 26.76% |
| No | 73.24% | |
| Do you maintain and update patients᾿ X-ray exposure history after every exposure? | Yes | 26.76 |
| No | 73.24% | |
| Do you give the card to the patient where you marked the effective dose? | Yes | 14.08% |
| No | 85.92% | |
| Do you have ionizing radiation warning signboards in your workplace? | Yes | 33.80% |
| No | 66.20% | |
| Do you have an indicator light on the door where there is the RX source? | Yes | 28.17% |
| No | 71.83% | |
| Do you maintain an RX source quality control management journal? | Yes | 28.17% |
| No | 71.83% | |
| Do you know who is «Radiation protection officer» of your clinic? | Yes | 39.44% |
| No | 60.56% |
Table 1: Distribution of answers from participants in management of radiographic waste.
Data was entered into an electronic database and analyzed using SPSS (Statistical Package for the Social Sciences for Windows). The level of statistical significance was set at P ≤ 0.05.
Results
402 persons of the dental staff participated in this study. Of the 402 respondents 46.47% were dentists, 22.53% were dental assistants and radiographers, 8.45% were dental residents, and 22.55% were other dental staff (Figure 1). The respondents were aged 22-66 years.
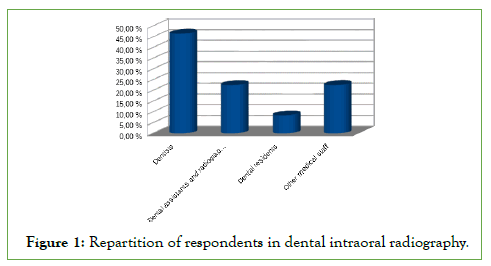
Figure 1: Repartition of respondents in dental intraoral radiography.
Protection of personnel
In our study only 39.43% of the participants followed the radiation protection and radiation safety course. 66.2% of participants declared that it is unnecessary for the person performing the dental intraoral imaging procedure to wear a lead apron. Only 33.8% of participants always wear lead apron. As for the use of thyroid collars 30.98% of the participants wear a thyroid collar during dental intraoral radiography. A large number of respondents don’t use any protection.
26.76% of operators use the position and distance rules correctly for their own protection. It has been observed that the number of participants don’t use personal passive dosimeters when they are performing dental intraoral radiography. Only 39.43% of operators always take their dosimeters. These findings indicate that 60.37% of participants neglect the importance of radiation monitoring for radiation protection measures.
Concerning imaging receptors holding, 25.36% of the patients hold imaging receptors with their hand during intraoral radiography procedure. 61.97% of professionals hold imaging receptors with their own hand and only 12.68% of professionals use film holders. This is due to the lack of film holders in the dental clinics.
Patient’s protection
The selection of exposure parameters such as tube voltage (kV), tube current (mA), and exposure time (s) depends not only on the patient but also on the type and properties of the image receptor used. In our study 73.24% of practitioners use the same exposure parameters for adult and pediatric patients.
In our study 35.21% of operators use lead aprons and 32.39% of operators use thyroid collars for their patients during exposition. According to our findings, the most patients have no protection during intraoral radiography procedures.
Patient’s exposure history must be maintained and updated after every exposure. Only 26.76% of participants maintain exposure history. 67.61% of cases traceability of X-ray dose is not performed. 14.08% of practitioners give the card to the patient where is marked the effective dose.
Management of radiographic workplace and equipment
33.80% of the participants stated that they have ionizing radiation warning signboards in their workplace and 28.17% of operators have an indicator light on the door where there is the X-ray source. In our study 71.83% of participants don’t keep any X-ray source quality control management journal. 60.56% of respondents were unable to say, who is the radiation protection officer of their clinic.
Discussion
Since the introduction of the X-ray and its uses in dental radiology, it has been a very important diagnostic method, especially in modern dentistry [11]. Radiology is a diagnostic test, and in dentistry, this test always involves the use of ionizing radiation. Therefore, oral and maxillofacial radiology should be performed thoughtfully and responsibly, minimizing radiation dose, but maximizing diagnostic benefit. Nevertheless, ionizing radiation could be biologically damaging to living tissues. It may directly damage the DNA of living cells and indirectly by creating free radicals. It has been postulated that repeated exposure to cytotoxic materials can result in chronic cell injury, compensatory cell proliferation, hyperplasia, and, ultimately, tumor development [12]. Understanding the potential risks and applying the precautions and preventive measures correctly is very important. Dentists and their staffs have a responsibility to ensure patient safety from the effects of radiation exposure during all dental radiography procedures.
Our study aimes to assess Georgian practitioner’s compliance with safety standards in oral radiology. The results showed that the awareness of radiation danger among dental practitioners was not completely sufficient.
The results of the study revealed that 35.21% of operators use lead aprons and 32.39% of operators use thyroid collars for patient’s protection. Hoogeveen et al. concluded that the thyroid shield helps in reduction of the dose to the thyroid when imaging the upper anterior teeth [13]. Schueler showed that a 0.5 mm thickness apron constricted 90% of the scatter radiation [14].
On the other hand, Hyun et al. quantified the level of 0.5 mm thick lead apron in blocking radiation, and they found that it blocked just over one-third of it [15]. Several studies show that repeated exposures to dental X-rays might be associated with a risk of thyroid cancer [16,17].
Lee et al. showed that more than 50% of the patients hold imaging receptors with their hands during intraoral radiography procedures [18]. In our study, the percentage of patients holding the imaging receptor themselves was 25.36%, while 61.97% of professionals held themselves and 12.68% used film holders. This is due to the lack of film holders in the dental clinics. E S Halboub et al. documented the harmful effect of holding the film in patient’s mouth during exposure [19].
Personal radiation monitoring devices or dosimeters are badges that detect various forms of radiation a worker may be exposed to. Workers are required to wear the dosimeters for periods of up to 3 months. The accumulated dose from the various types of radiation is measured by the dosimetry service provider and reported to the employer [20]. It was revealed that 39.43% of operators wore their dosimeters.
The best method for operator protection is to use a protective barrier or to leave the room during radiographic exposure. However, if it is not possible, the operator should stand in the proper position and at a distance. The operator should stand at least 6 feet from the patient at the angle of 90° to 135° to the central ray of X-ray beam. On application, this rule not only takes advantage of the inverse square law of reduce X-ray exposure to the operator but also take the advantage of the fact that in this position, the patient’s head absorbs most scattered radiation [21]. In our study only 26.76% participants were know about the correct position and distance rule.
An important consideration with dental radiography is the X-ray spectral sensitivity of dental X-ray film and the image quality at different kilo voltages. Use of 60 kV-70 kV for intraoral radiography is considered to be a reasonable choice in terms of limiting dose and diagnostic efficacy [22]. The tube current is usually 3.5 mA to 8 mA, and the exposure time can be set depending on the image receptor, patient age and anatomical area [3]. Selecting an appropriate exposure time is very important in minimizing patient’s radiation exposure. We emphasized that fact that 73.24% of practitioners use the same exposure parameters whether the patient is adult or child. The process of optimizing protection in work procedures should be emphasized since it directly influences the quality and safety of patient care.
Georgian Dental Association (GDA) organizes radiation protection and radiation safety courses including information on the levels of radiation exposure to which dental patients are subjected; X-ray dose optimization, educational material on radiation risks and radiation safety for both patients and employees. Most of the respondents in the present study didn’t participate in the radiation safety program. As we saw above 39.43% of the participants were trained in radation protection.
Several studies shows that radiographers do not need to use radiation protection equipment such as lead aprons and thyroid collars if they are not exposed to direct radiation, 2 m from the source of scattered radiation [22]. In our study 33.8% of participants always wear a lead apron and 30.98% of the participants wear a thyroid collar during dental intraoral radiography. In a study carried out in Belgium, it is reported that 88% of the radiographers do not wear a lead apron, while female radiographers are found to use this equipment more frequently than male radiographers. This difference was referred to as possible pregnancy and a higher level of radiation protection awareness of female workers [23].
The quality assurance of the radiographic system should be performed to ensure the optimum exposure conditions. The quality assurance is X-ray machine maintenance, and regular check-ups of the equipment are a necessity. In our study 71.83% of participants don’t maintain RX source quality control.
Conclusion
The present study has revealed a lack of knowledge on the part of dental staff about the rules and guidelines for the practice of radiology and radioprotection the need to reinforce the importance of radiation protection in the dental curriculum in Georgia. Special attention should be paid to justification and optimization to minimize unnecessary radiation exposure in dental practices. Many steps can be taken to reduce patient exposure to radiation. The training of dental practitioners must be mandated prior to the use of ionizing radiation in dental practice. Therefore, the education, training, qualification and competence of the health professionals involved are of the utmost importance with respect to the safe use of ionizing radiation in dentistry.
Acknowledgment
We thank the dental staff-respondents, who kindly took time to answer the survey. We also thank Georgian Dental Association and Especially President of GSA Ketevan Kiguradze-Gogilashvili for assistance, support and guidance in our research.
References
- Shahab S, Kavosi A, Nazarinia H, Mehralizadeh S, Mohammadpour M, Emami M. Compliance of Iranian dentists with safety standards of oral radiology. Dentomaxillofac Radiol. 2012;41(2):159-164.
[Crossref] [Google Scholar] [PubMed]
- Medical Radiation Exposure of the European Population, Radiation Protection. Publications Office of the European Union. 2015.
- IAEA Safety reports Series No. 108. Radiation protection in dental radiology.2022.
- WER Berkhout Ned Tijdschr Tandheelkd. 2015;122(5):263-270
- Crane GD, Abbott PV. Radiation shielding in dentistry: An update. Aust Dent J. 2016;61(3):277-281.
[Crossref] [Google Scholar] [PubMed]
- Yurt A, AyrancıoÄ?lu C, Kılınç G, Ergönül E. Knowledge, attitude, and behavior of Turkish dentists about radiation protection and radiation safety. Dentomaxillofac Radiol. 2021;51(1).
[Crossref] [Google Scholar] [PubMed]
- Memon A, Godward S, Williams D, Siddique I, Al-Saleh K. Dental X-rays and the risk of thyroid cancer: A case-control study. Acta Oncol. 2010;49(4):447-453.
[Crossref] [Google Scholar] [PubMed]
- Hujoel PP, Bollen AM, Noonan CJ, del Aguila MA. Antepartum dental radiography and infant low birth weight. JAMA. 2004;291(16):1987-1993.
[Crossref] [Google Scholar] [PubMed]
- Praveen BN, Shubhasini AR, Bhanushree R, Sumsum PS, Sushma CN. Radiation in dental practice: Awareness, protection and recommendations. J Contemp Dent Pract. 2013;14(1):143.
[Crossref] [Google Scholar] [PubMed]
- Todua F, Nadareishvili D, Ormotsadze G, Sanikidze T. Basic radiation protection education and training for medical professionals; Georgian experience and future perspective. Radiat Prot Dosimetry. 2016;169(4):422-424.
[Crossref] [Google Scholar] [PubMed]
- Jones CG. A review of the history of US radiation protection regulations, recommendations, and standards. Health Phys. 2005;88(2):105-124.
[Crossref] [Google Scholar] [PubMed]
- Ribeiro DA, Oliveira G, Castro GM, Angelieri F. Cytogenetic biomonitoring in patients exposed to dental X-rays: Comparison between adults and children. Dentomaxillofac Radiol. 2008;37(7):404-407.
[Crossref] [Google Scholar] [PubMed]
- Hoogeveen RC, Hazenoot B, Sanderink GC, Berkhout WE. The value of thyroid shielding in intraoral radiography. Dentomaxillofac Radiol. 2016;45(5):20150407.
[Crossref] [Google Scholar] [PubMed]
- Schueler BA. Operator shielding: How and why. Tech Vasc Interv Radiol. 2010;13(3):167-171.
[Crossref] [Google Scholar] [PubMed]
- Hyun SJ, Kim KJ, Jahng TA, Kim HJ. Efficiency of lead aprons in blocking radiation-how protective are they?. Heliyon. 2016;2(5).
[Crossref] [Google Scholar] [PubMed]
- Memon A, Godward S, Williams D, Siddique I, Al-Saleh K. Dental X-rays and the risk of thyroid cancer: A case-control study. Acta Oncol. 2010;49(4):447-453.
[Crossref] [Google Scholar] [PubMed]
- Neta G, Rajaraman P, Berrington de Gonzalez A, Doody MM, Alexander BH, Preston D, et al. A prospective study of medical diagnostic radiography and risk of thyroid cancer. Am J Epidemiol. 2013;177(8):800-809.
[Crossref] [Google Scholar] [PubMed]
- Lee BD, Ludlow JB. Attitude of the Korean dentists towards radiation safety and selection criteria. Imaging Sci Dent. 2013;43(3):179-184.
[Crossref] [Google Scholar] [PubMed]
- Halboub ES, Barngkgei I, Alsabbagh O, Hamadah O. Radiation-induced thumbs carcinoma due to practicing dental X-ray. Contemp Clin Dent. 2015;6(1):116.
[Crossref] [Google Scholar] [PubMed]
- Personal Radiation Monitoring-Information for Employers and Employees. 2013.
- White SC, Pharoah MJ. Radiation safety and protection. Oral radiology principles and interpretation. St Louis. 2009:32-43.
- Radiation Protection 136: European guidelines on radiation protection in dental radiology. 2004
- Jacobs R, Vanderstappen M, Bogaerts R, Gijbels F. Attitude of the Belgian dentist population towards radiation protection. Dentomaxillofac Radiol. 2004;33(5):334-339.
[Crossref] [Google Scholar] [PubMed]
Citation: Maisuradze A, Gogilashvili K, Fettak F, Alkhanishvili Z, Oghiashvili K, Akhobadze M, et al. (2023) Attitude of the Dental Staff towards Radiation Safety in Georgia-Radiation Protection of Patients and Staff. J Dentistry.13:659.
Copyright: © 2023 Maisuradze A, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

