Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- Google Scholar
- SHERPA ROMEO
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2026) Volume 14, Issue 1
Application of Shockwave Balloon Intravascular Lithotripsy in the Treatment of Severe Calcification of Aortic Branches: Two Cases Report
Jianli Luan1, Guanzhi Zhou1, Xingyi Tang1, Huibo Ma1, Zhihui Wang2, Huichao Xu1, Yangshuo Liu1, Zhenyuan Zhao1, Yongxin Li1 and Mingjin Guo1*2Department of Cardiovascular Medicine, The Affiliated Hospital of Qingdao University, Qingdao University, Shandong, China
Received: 16-Aug-2024, Manuscript No. JVMS-24-26761; Editor assigned: 20-Aug-2024, Pre QC No. JVMS-24-26761 (PQ); Reviewed: 03-Sep-2024, QC No. JVMS-24-26761; Revised: 03-Feb-2026, Manuscript No. JVMS-24-26761 (R); Published: 10-Feb-2026, DOI: 10.350310/2329-6925.26.14.600
Abstract
Intravascular Lithotripsy (IVL) using shockwave balloon has been commonly applied in patients with coronary artery calcification stenosis. IVL is a technology based on lithotripsy, where multiple emitters installed on a traditional balloon catheter to selectively emits non-focusing and pulsed shockwaves to safely disrupt arterial plaque calcification, enhancing vascular compliance, and optimizing stent expansion. The shockwave balloon does not damage the flexible vessel wall and leaves the disrupted calcification reshaped but not fragmented, providing a novel treatment approach for severe calcified vascular stenosis. However, the application of shockwave balloon in aortic branches has limited clinical experience. This report aims to present two cases of shockwave balloon angioplasty for the treatment of severe calcification of aortic branches. This is an innovative method. The operation was successful and the patient recovered well after the operation.
Keywords
Shockwave intravascular lithotripsy system; Renal artery; Subclavian artery; Atherosclerosis plaque calcification; Case report
Introduction
Arteriosclerosis is commonly considered a chronic inflammatory disease, where inflammation plays a crucial role in all stages of the arteriosclerotic process. Calcification may occur during the progression of arteriosclerosis [1]. And as the population ages and the prevalence of diabetes and renal disease continues to rise, the prevalence of cardiovascular calcium has also risen [2]. Similarly, calcified arterial disease adds to lesion complexity, representing a lower success rate of operation and an increased risk of adverse events.
In this article, we report two cases with a severe calcification of aortic branches. Both patients developed severe calcific stenosis in the major branches of the aorta. Our team decided to perform shockwave balloon angioplasty to disrupt calcified plaques, facilitating stent expansion and lumen dilation. Up to now, our patients has been followed up for 1 years. The postoperative outcomes were good, and the corresponding symptoms significantly improved. This operation achieved successful clinical results.
Case Presentation
Case 1
Patient Li, male, 63 years old, presented at The Affiliated Hospital Qingdao University on September 21, 2022, with a chief complaint of "Recurrent hypertension for over 2 years."
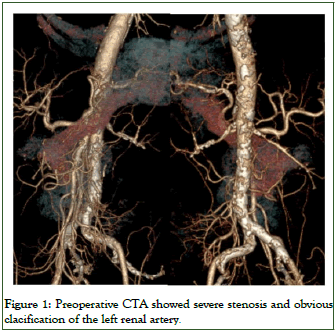
Two years ago, the patient started experiencing recurrent hypertension without any apparent triggering factors, and it was difficult to control. He had a history of hypertension for more than 20 years, with the highest blood pressure reaching 230/90 mmHg. He had a history of polycystic kidney disease for 7 years and had been undergoing regular blood dialysis. Upon admission, the patient's blood pressure 144/69 mmHg (1 mmHg=0.133 kPa). Laboratory tests: Kidney function test showed a creatinine level of 675.9 mmol/L. Abdominal aorta CT Angiography (CTA) revealed multiple calcified plaques in both renal arteries, with multiple moderate to severe stenoses in the lumen (Figure 1). Urinary system ultrasound showed unclear visualization of the main stems of both renal arteries.
Figure 1: Preoperative CTA showed severe stenosis and obvious clacification of the left renal artery.
The preoperative diagnosis for the patient includes renal artery stenosis, uremia, refractory hypertension, stage 3 hypertension (extremely high-risk), and polycystic kidney disease. The surgery performed was bilateral renal artery balloon angioplasty with stent placement. The procedure began with a retrograde puncture of the right femoral artery, and then a super-slip guidewire was advanced in an antegrade manner. Using the 6F guiding sheath, a 0.035" super-slip guidewire and a single-curve catheter were inserted. Push the 4F single-curve catheter forward and place it in the abdominal aorta for angiography, revealing severe stenosis at the starting segment of both renal arteries and moderate stenosis in the left renal artery. The guidewire was rotated into the left renal artery, and the angiography showed severe stenosis with approximately 1 cm of calcification in the midsection of the left renal artery, and there is no stenosis in the distal artery (Figure 2a). An ATW guidewire was exchanged, and a 4.5 mm × 60 mm shockwave lithotripsy balloon was advanced. The midsection of the renal artery calcified segment was subsequently treated with the 4.5 mm × 60 mm shockwave lithotripsy balloon which was inflated at 4 atmospheres for 30s (Figure 2b). Final angiogram showed good angiographic results in the midsection of the renal artery, no overt dissection. There was no acute vessel closure and post endovascular therapy complications. A balloon-expandable stent (BIOTRONIC 5 × 12 mm) was deployed at the origin of the left renal artery using the same method. Repeat angiography showed a patent left renal artery with complete disappearance of the stenosis (Figure 2c). The same IVL technique was employed to treat the stenosis at the origin of the right renal artery (Figure 2d, e), and the angiography showed improved blood flow and the formation of a dissection at the distal end. So we put a self-expanding stent (smart control 6 mm × 60 mm) to fully cover the stenosis and the origin of arterial dissection, and angiography shows unobstructed blood flow in the right renal artery (Figure 2f). After the operation, the catheter, guidewire, and sheath were removed, and the femoral artery puncture site was sutured using a percutaneous vascular closure device. The procedure lasted for 80 minutes. Postoperatively, both renal arteries showed patency, and the stenosis was resolved (Figure 3). Post-operatively, the patient’s blood pressure was 140/70 mmHg. The patient has been followed up for 1 years and the patient's stent patency was found to be excellent.
Figure 2: Surgical process. a) DSA showed severe stenosis of the left renal artery. b) Using the shockwave balloon. c): Left renal arteries showed patency, and the stenosis was resolved. d): DSA showed severe stenosis of the right renal artery. e): Using the shockwave balloon. f): Right renal arteries showed patency, and the stenosis was resolved.
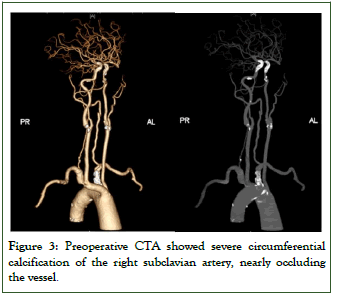
Figure 3: Preoperative CTA showed severe circumferential calcification of the right subclavian artery, nearly occluding the vessel.
Case 2
Patient Zhu, male, 67 years old, presented at The Affiliated Hospital Qingdao University on September 21, 2022, with a chief complaint of " bilateral upper limb weakness for six months"
Six months ago, the patient presented with bilateral upper limb weakness, accompanied by soreness and numbness. The patient has a medical history of diabetes for over 20 years. He also had a history of atrial fibrillation for more than 10 years, with a previous treatment of radiofrequency ablation. He had a history of coronary atherosclerotic heart disease for over 10 years. Five months ago, the patient underwent a stent implantation procedure for "left subclavian artery stenosis and steal syndrome". Upon admission, the patient's blood pressure in the right upper limb was 85/60 mmHg, and in the left upper limb was 90/51 mmHg. Laboratory examinations: Carotid ultrasound examination revealed that moderate narrowing and plaque formation in the right subclavian artery. The right vertebral artery showed abnormal spectral morphology, suggestive of right subclavian artery steal syndrome. Carotid Artery on CT Angiography (CTA) demonstrated a visible stent shadow in the proximal left subclavian artery, while the right subclavian artery exhibited severe circumferential calcification and a narrowed lumen.
The preoperative diagnosis for the patient includes Right subclavian artery stenosis, carotid artery stenosis, atrial fibrillation, type 2 diabetes mellitus, coronary atherosclerotic heart disease. The surgery performed was right subclavian artery balloon angioplasty with stent placement. The right femoral artery was punctured retrogradely, and a 6F sheath was inserted. Angiography of the iliac artery and abdominal aorta was performed, showing patent flow in the abdominal aorta and iliac artery. Using the sheath, a 0.035" super slippery guidewire was advanced to the brachiocephalic trunk and then exchanged for a 4F single-curve catheter. The guidewire was removed, and angiography of the around artery was performed. The angiogram revealed patent flow in the brachiocephalic artery, while the right subclavian artery showed severe stenosis at its origin with near occlusion and distal dilation (Figure 4a). After exchanging to an 8F-90 long sheath, the guidewire was rotated into the right subclavian artery. A balloon catheter (Medtronic 4.0 × 40 mm-130 cm) was then advanced over the guidewire to perform balloon angioplasty of the right subclavian artery (Figure 4b). Subsequently, an intravascular lithotripsy (IVL) catheter (Shockwave M5 IVL 7 mm × 60 mm-110 cm) was exchanged and used for intravascular shockwave lithotripsy of the calcified plaque in the right subclavian artery (Figure 4c). After satisfactory dilation, a stent (Dynamic 10/38) was introduced and positioned at the site of the subclavian artery stenosis, and the stent was released. Following stent placement, repeat angiography demonstrated a patent right subclavian artery without any stenosis (Figure 4d). Postoperative treatment is the same as before. The procedure was successful, lasting for 65 minutes. Post-operatively, the patient's blood pressure was 140/70 mmHg. The patient has been followed up for 1 years and the patient's stent patency was found to be excellent.
Figure 4: Surgical process. a): Intraoperative Digital Subtraction Angiography (DSA) revealed severe stenosis at the origin of the right subclavian artery. b): Perform balloon angioplasty of the right subclavian artery c): Performed right subclavian artery intravascular shockwave lithotripsy to fragment the calcified plaque. d): After stent deployment, angiography revealed a patent right subclavian artery with no stenosis.
Results and Discussion
Vascular calcification (VC), which is categorized by intimal and medial calcification, depending on the site(s) involved within the vessel, is closely related to cardiovascular disease. VC is a common pathological manifestation of various diseases such as atherosclerosis, hypertension, diabetes mellitus, and chronic kidney disease [3]. Calcification often accompanies the development of advanced atherosclerosis, leading to the loss of intimal elasticity. With the degeneration and calcification of the middle layer of the artery, leading to arterial wall thickening and narrowing of the vessel lumen. It portends a poor prognosis and is independently associated with increased cardiovascular mortalit and morbidity risk [4]. Currently, there are two surgical treatment options for arteries stenosis ischemia: Open surgery and Intravascular intervention. Open surgery is removing the affected vascular and replacing it with an artificial vascular. For intravascular intervention, there are multiple methods of treating with severe calcification of atherosclerotic: Percutaneous Transluminal Angioplasty (PTA), atherectomy, etc. [5]. And now we have a new method: Shockwave balloon intravascular lithotripsy.
Calcification may also interfere with the endovascular therapies in which it is responsible for suboptimal vessel expansion and increased risk of vascular complications including restenosis, dissection, perforation, and distal embolization [6,7]. Percutaneous Transluminal Angioplasty (PTA) or stent placement relies on plaque rupture and vessel wall stretching. Severe arterial calcification can significantly impact blood flow within the blood vessels, reducing vascular elasticity and compliance. In the treatment of calcified lesions, conventional balloons cannot achieve ideal expansion, potentially leading to balloon rupture, vascular dissection, and perforation; stent implantation may cause incomplete stent expansion and poor wall apposition, increasing the risk of in-stent restenosis. The existing atherectomy devices carry a higher risk of dissection and vessel rupture during surgery. Once these complications occur, the procedure may be abandoned or redirected to surgical intervention due to the risk of embolism. This risk is particularly evident in severely calcified vessels. IVL is a novel technique in which multiple lithotripsy emitters deliver a small electrical discharge which vaporizes the fluid and creates a rapidly expanding bubble within the balloon. This bubble generates a series of sonic pressure waves at nearly 50- atmosphere pressure that travel through the fluid-filled balloon and pass through soft vascular tissue, selectively cracking the hardened intimal and medial calcified plaque, thereby serving as a novel vessel preparation strategy to improve luminal compliance and facilitate definitive endovascular treatment. IVL was initially applied to coronary artery disease, and has shown good results in the treatment of various peripheral artery diseases, such as lower limb arteries and major branches of the abdominal aorta, with severe calcified lesions [8,9]. Khalid et al. reported the first treatment for patients with abdominal aortic aneurysm and aortic stenosis with IVL. Chag et al. first used IVL to treat severe calcified stenosis of the abdominal aorta with kidney arterial stenosis in 2021, its gentle expansion effectively avoids the renal artery occlusion caused by calcification. Singlearm studies of IVL have reported effectiveness and safety results in the treatment of moderately and severely calcified vessels with high short-term procedural success rates, marked reduction in shortterm residual stenosis (<30%), and no major dissections, perforations, abrupt closure, or slow flow/no-reflow was reported.
Based on relevant clinical presentations and CT imaging, the diagnosis of the two cases is atherosclerosis with refractory calcification. Conventional balloon angioplasty followed by stent placement could not improve the vascular blood flow. The choice of lesion pre-treatment is crucial to minimize elastic recoil and flow-limiting dissections in the affected vessels. According to the experience of treating severe calcification of atherosclerotic plaque, the application of shockwave balloon intravascular lithotripsy is appropriate in this case. For severe calcified stenosis in the lesion area, a shockwave balloon was used for lesion pre-treatment. This played an important role in subsequent stent implantation.
We successfully use a novel combination of IVL and balloonmounted stenting angioplasty to treat the severe calcification of aortic branches. The results show a dramatic reduction in stenosis severity with high acute gain and minimal vessel injury. There were no major adverse events or revascularizations after the index procedure, and vessel patency was durable out to 10 months.
Conclusion
In summary, the use of a shockwave balloon in aortic branch lesions can reduce procedure time, minimize balloon slippage, achieve good immediate lumen gain, and result in larger in-stent areas. Postoperative follow-up shows no increase in mortality or in-stent restenosis, indicating good efficacy and safety.
This case successfully demonstrates the efficacy of using IVL for severe calcified aortic branch lesions, with excellent lumen reconstruction, highlighting IVL is a safe and effective vessel preparation strategy. And IVL have shown the great potential in treating heavily calcified aortic lesions, but its safety and longterm patency still require validation with larger samples and longer follow-up studies.
Acknowledgments
We acknowledge the contributions of specific colleagues, institutions, or agencies that aided the efforts of the authors.
Author Contributions
Conception and design: Jianli Luan; Collection of data: Guanzhi Zhou, Xingyi Tang, Huibo Ma; Data analysis and interpretation: Jianli Luan, Zhihui Wang, Huichao Xu, Yangshuo Liu, Zhenyuan Zhao; Manuscript writing and approval of manuscript: all authors.
Sources of Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Conflict of Interest
None to report.
References
- Geovanini GR, Libby P. Atherosclerosis and inflammation: overview and updates. Clin Sci (Lond). 2018;132(12):1243-1252.
[Crossref] [Google Scholar] [PubMed]
- Rocha-Singh KJ, Zeller T, Jaff MR. Peripheral arterial calcification: prevalence, mechanism, detection, and clinical implications. Catheter Cardiovasc Interv. 2014;83(6).
[Crossref] [Google Scholar] [PubMed]
- Yahagi K, Kolodgie FD, Lutter C, Mori H, Romero ME, Finn AV, et al. Pathology of human coronary and carotid artery atherosclerosis and vascular calcification in diabetes mellitus. Arterioscler Thromb Vasc Biol. 2017;37(2):191-204.
[Crossref] [Google Scholar] [PubMed]
- Vinci MC, Chowdhury MM, Makris GC, Tarkin JM, Joshi FR, Hayes PD, et al. Lower limb arterial calcification (LLAC) scores in patients with symptomatic peripheral arterial disease are associated with increased cardiac mortality and morbidity. PLoS One. 2017;12(9):e0182952.
[Crossref] [Google Scholar] [PubMed]
- Schlieper G, Schurgers L, Brandenburg V, Reutelingsperger C, Floege J. Vascular calcification in chronic kidney disease: an update. Nephrol Dial Transplant. 2016;31(1):31-39.
[Crossref] [Google Scholar] [PubMed]
- Lee MS, Canan T, Rha SW, Mustapha J, Adams GL. Pooled analysis of the CONFIRM registries. J Endovasc Ther. 2015;22(1):57-62.
- Babaev A, Zavlunova S, Attubato MJ, Martinsen BJ, Mintz GS, Maehara A. Orbital atherectomy plaque modification assessment of the femoropopliteal artery via intravascular ultrasound (TRUTH study). Vasc Endovascular Surg. 2015;49(7):188-194.
[Crossref] [Google Scholar] [PubMed]
- Case BC, Yerasi C, Forrestal BJ, Khalid N, Shlofmitz E, Satler LF, et al. Intravascular lithotripsy facilitated percutaneous endovascular intervention of the aortic arch: a single-center experience. Cardiovasc Revasc Med. 2020;21(8):1006-1015.
[Crossref] [Google Scholar] [PubMed]
- Tayal R, Sohal S, Okoh A, Wasty N, Waxman S, Salemi A. Intravascular lithotripsy enabled transfemoral transcatheter aortic valve implantation via percutaneous axillary access approach. Cardiovasc Revasc Med. 2021;28:89-93.
[Crossref] [Google Scholar] [PubMed]
Citation: Luan J, Zhou G, Tang X, Ma H, Wang Z, Xu H, et al. (2025) Application of Shockwave Balloon Intravascular Lithotripsy in the Treatment of Severe Calcification of Aortic Branches: Two Cases Report. J Vasc Surg. 14:600.
Copyright: © 2026 Luan J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.