Indexed In
- Open J Gate
- Academic Keys
- ResearchBible
- China National Knowledge Infrastructure (CNKI)
- Centre for Agriculture and Biosciences International (CABI)
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- CABI full text
- Publons
- Geneva Foundation for Medical Education and Research
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research - (2020) Volume 8, Issue 5
Analysis of Hematological Changes and Seroprevalence of Malarial Patients Caused by Plasmodium Vivax Using Statistical Tools
Shah Faisal1, Muhammad Taj Akbar2, Abdullah2, Hamidullah Shah3*, Asma Qudrat2, Faheem Jan4 and Jafar Ali52Department of Microbiology, Abdul Wali Khan University, Mardan, KPK, Pakistan
3Department of Pathology, Lady Reading Hospital, Peshawar, KPK, Pakistan
4Programmatic Management of Drug Resistant, TB Unit Ayub Teaching Hospital, Abbottabad, KPK, Pakistan
5Medical Entomologist Integrated Vector Management Program for Merged Areas IVMP-MAS, Peshawar, Pakistan
Received: 18-Jul-2020 Published: 30-Jul-2020, DOI: 10.35248/2329-891X.20.8.354
Abstract
Malaria is a febrile illness, caused by malarial plasmodium parasite. It is the most prevalent infectious disease in the tropical and subtropical regions of the world in addition Pakistan is amongst the highly affected countries regarding infectivity rate of malaria. The main objective of the current research was to analyzed haematological changes and seroprevalence of malaria infection in patients caused by Plasmodium vivax. The study was conducted at Katlang Diagnostic Centre Mardan, Khyber Pakhtunkhwa, Pakistan. A total of 188 patients having malaria disease were enrolled, in which frequency of male patients were 122 (64.9%) while frequency of female patients was 66 (35.1%). Results indicated that there was no association between gender and BT Ring condition, because the value of chi-square (0.215) was greater than p value (0.5). Similarly, the value of chi-square (0.540) was greater than p value (0.05), which showed that there was no association between gender and B Trophozoite condition. Analysis also showed that there was close association between BT Ring and B Trophozoite condition with each other, because the value of chi-square is (0.000) which is less than p value (0.05). The present study concludes that there is a close association between BT Ring and B Trophozoite conditions.
Keywords
Malaria; Mardan; Plasmodium vivax
Introduction
Malaria is a febrile illness, caused by malarial plasmodium parasite. It results from the bite of female anopheles’ mosquito. The mosquito inoculates sporozoites in human blood which consequent upon clinical symptoms after a specific incubation period. Malaria is caused by four species of Plasmodium; Plasmodium vivax, Plasmodium falciparum, Plasmodium ovale and Plasmodium malaria [1]. Malaria is the most prevalent infectious disease in the tropical and subtropical regions of the world in addition to being the major cause of morbidity in the tropics [2]. Pakistan is amongst the highly affected countries regarding infectivity rate of malaria. Malaria is a common disease in rural India with high mortality and morbidity [1,3].
Malaria not only presents as acute episodes of fever but also as an important cause of anaemia in children and adults. It is responsible for many adverse outcomes like spontaneous abortion, stillbirth, and premature delivery among pregnant women in India and developing countries and also for low birth weight, and overall child mortality. Malaria is also an important cause of economic slowdown, an estimated average annual reduction of 1.3% in the economic growth for those countries with the highest incidence of malaria.
Thrombocytopenia has been reported to be associated with malaria with an incidence ranging from 24% to 94%, with some studies reporting a lower incidence in vivax malaria as compared to falciparum malaria [4]. Hematologic changes associated with malaria infection are well recognized, but specific changes may vary with level of malaria endemicity, background hemoglobinopathy, nutritional status, demographic factors, and malaria immunity [5]. Haemolysis in malaria leads to anaemia, altering the hemopoiesis, to a disproportionate reticulocyte counts, reduced platelets and WBC counts. Malaria is commonly associated with mild to moderate thrombocytopenia which is rarely associated with hemorrhagic outcomes or disseminated intravascular coagulation. Thrombocytopenia may occur in majority of malaria cases, laboratory variance related with malaria are well identified but it may change with type, level of immunity, demographic factors and malaria endemicity [1,6]. The main objective of the current research was to analyse haematological changes and seroprevalence of malaria infection in patients caused by Plasmodium vivax.
Methodology
Enrolment of patients
This was prospective cross-sectional study. It was conducted on 188 malarial patients of different ages and gender, who attended Katlang Diagnostic Centre Mardan, Khyber Pakhtunkhwa, Pakistan.
Collection of blood samples
Approximately 4 ml blood samples were aseptically collected from every enrolled malaria patient into EDTA containers for the thick blood film preparation to detect the presence or absence of malaria parasites and determine Full Blood Counts (FBCs) involving haematocrit, haemoglobin concentration, white blood cell count, platelet count, granulocyte count, lymphocyte count, and mid-cell count (monocyte, eosinophil, and basophil count).
Statistical analysis
The collected data were checked for completeness regularly during the course of data collection. The data were entered, cleaned, and analyzed using SPSS version 20.0. Descriptive statistics including frequency, mean, and standard deviation were utilized to summarize demographic profile of the patients while Chi-square test was used for further analysis Figure 1.
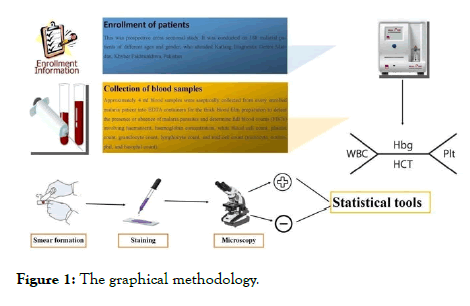
Figure 1. The graphical methodology.
Results
A haematological change and seroprevalence of malaria infection in patients caused by Plasmodium vivax were studied. There were 188 patients having malaria disease, in which frequency of male patients were 122 (64.9%) while frequency of female patients were 66 (35.1%) as shown in Table 1.
| Gender | Frequency | Percent | Cumulative percent |
|---|---|---|---|
| Male | 122 | 64.9 | 64.9 |
| Female | 66 | 35.1 | 100 |
| Total | 188 | 100 |
Table 1: Frequency of male and female patients in the current study.
Out of 122 male patients, frequency of male patients having BT Ring positive condition were 55 while having BT Ring negative condition were 67. Similarly, out of 66 female patients, frequency of female patients having BT Ring positive condition were 36 while having BT Ring negative condition were 30. Out of 188 patients, frequency of BT Ring positive condition in both male and female was 91 while frequency of BT Ring negative condition in both male and female was 97. Using Chi-square test, analysis showed that there was no association between gender and BT Ring condition, because the value of chi-square (0.215) was greater than p value (0.0.5). Therefore, it was concluded that there are no significance differences between these two variables as shown in Table 2.
| Chi-square tests | |||||
|---|---|---|---|---|---|
| Value | Df | Asymp. sig. (2-sided) | Exact sig. (2-sided) | Exact sig. (1-sided) | |
| Pearson chi-square | 1.536 | 1 | 0.215 | -- | -- |
| Continuity correction | 1.18 | 1 | 0.277 | -- | -- |
| Likelihood ratio | 1.537 | 1 | 0.215 | -- | -- |
| Fisher's exact test | -- | -- | -- | 0.225 | 0.139 |
| Linear-by-linear association | 1.528 | 1 | 0.216 | -- | -- |
| No of valid cases | 188 | -- | -- | -- | -- |
Table 2: Analysis of chi-square between gender and BT ring condition.
Out of 122 male patients, frequency of male patients having B Trophoziate positive were 104 while having B Trophoziate negative were 18. Similarly, out of 66 female patients, frequency of female patients having B Trophoziate positive were 54 while having B Trophoziate negative were 12. Out of 188 patients, frequency of B Trophoziate positive in both male and female was 158 while frequency of B Trophoziate negative in both male and female was 30. Analysis showed that there was no association between gender and B Trophoziate condition, because the value of chi-square (0.540) was greater than p value (0.05). So, it was concluded that there are no significance differences between gender and B Trophoziate variables as shown in Table 3.
| Chi-square tests | |||||
|---|---|---|---|---|---|
| Value | Df | Asymp. sig. (2-sided) | Exact sig. (2-sided) | Exact sig. (1-sided) | |
| Pearson chi-square | 0.375 | 1 | 0.54 | ||
| Continuity correction | 0.163 | 1 | 0.686 | ||
| Likelihood ratio | 0.369 | 1 | 0.543 | ||
| Fisher's exact test | 0.539 | 0.339 | |||
| Linear-by-linear association | 0.373 | 1 | 0.541 | ||
| No of valid cases | 188 | ||||
Table 3: Analysis of chi-square between gender and B Trophoziate condition.
Out of 91 patients, frequency of patients having both BT Ring and B Trophoziate positive were 66 while having BT Ring positive and B Trophoziate negative were 25. Similarly, out of 97 patients, frequency of patients having BT Ring negative and B Trophoziate positive were 92 while having both BT Ring and B Trophoziate negative were 5. The analysis showed that there is association between BT Ring and Trophoziate disease, because the value of chi-square is (0.000) which is less than p value (0.05). So, it was concluded that there is a significance differences between BT Ring and Trophoziate variable as shown in Table 4.
| Chi-square tests | |||||
|---|---|---|---|---|---|
| Value | Df | Asymp. sig. (2-sided) | Exact sig. (2-sided) | Exact sig. (1-sided) | |
| Pearson chi-square | 17.438 | 1 | 0 | ||
| Continuity correction | 15.814 | 1 | 0 | ||
| Likelihood ratio | 18.662 | 1 | 0 | ||
| Fisher's exact test | 0 | 0 | |||
| Linear-by-linear association | 17.345 | 1 | 0 | ||
| No of valid cases | 188 | ||||
Table 4: Analysis of chi-square between BT Ring and B Trophoziate condition.
Haematological changes in malarial patients caused by Plasmodium vivax were observed. Results showed that out of 188 patients, Patients having platelets amount below 150000 were 142 (75.5%), 150000 to 450000 were 45 (23.9%), and above 450000 were 1 (0.5%). Patients having TLC amount below 4000 were 20 (10.6%), 4000 to 11000 were 161 (85.6%), and above 11000 were 7 (3.7%). Patients having MCHC amount below 32 were 36 (19.1%), 32 to 36 were 150 (79.8%), and above 36 were 2 (1.1%). Patients having MCH amount below 27 were 37 (38.8%), 27 to 33 were 111 (59.0%), and above 33 were 4 (2.1%). Patients having MCV range below 80 were 48 (25.5%), 80 to 100 were 138 (73.4%), and above 100 were 2 (1.1%).
Out of 121 male patients, patients having RBC range below 5.52 were 51 and 5.52 to 5.90 were 70, while out of 67 female patients, patients having RBC range 3 were 5, below 4.10 were 21 and 4.10 to 5.10 were 41. Out of 111 male patients, patients having HCT range below 40.00 were 61 and 40.00 to 54.00 were 50, while out of 67 female patients, patients having HCT range 36.00 were 40 and 36.00 to 46.00 were 27. Out of 121 male patients, patients having Hb range below 14.00 were 89 and 14.00 to 18.00 were 32, while out of 67 female patients, patients having Hb range 12.00 were 41, 12.00 to 16.00 were 26, and above 16.00 were zero.
Discussion
The hematological changes related with malaria are familiar, but precise changes may vary with category of malaria, with the background of hemoglobinopathy, nutritional status, demographic factors and malaria immunity [6]. The main aim of this study was to determine the common hematological changes among the malaria infected patients. Accordingly, the overall prevalence of anaemia was 40.3%. Anaemia is a common complication associated with malaria [7]. The magnitude of anaemia among malaria infected patients varies depending on demographic factors, nutritional status, pre-existing physiologic conditions, and co infection with other diseases [8]. A study conducted by Bega et al. in a tertiary care hospital in Karachi which showed P. vivax in 52% and P. falciparum in 46% of patients with acute malaria [9].
Malaria typically affects blood indices in various ways with anaemia and thrombocytopenia being the frequent associated hematological outcomes. Studies have reported thrombocytopenia as a sensitive marker for a malaria diagnosis in the presence of acute febrile illness, having a sensitivity of 60%, a specificity of 88%, and a positive and negative predictive value of 86% and 100%, respectively [10]. The exact mechanism of pathogenesis of malarial thrombocytopenia is not clear. Suggested mechanisms of thrombocytopenia in malaria include splenic phagocytosis of activated platelets, coagulation disturbances, and bone mar-row alterations [11]. Unless treated early, thrombocytopenia may also play role in the pathogenesis of cerebral malaria [6]. Researchers have also suggested thrombocytopenia as a result of consumption by Disseminated Intravascular Coagulation (DIC) and peripheral platelet destruction induced by P. falciparum, although the latter mechanism has not been systematically evaluated in P. vivax malaria. Similarly, studies have considered the peripheral destruction of RBCs, ineffective hematopoiesis, and sequestration in the spleen as possible causes of malaria-induced anaemia [12].
In the present study, haematological changes and seroprevalence of malaria infection in patients caused by Plasmodium vivax was analysed. A total of 188 patients having malaria disease were enrolled, in which frequency of male patients were 122 (64.9%) while frequency of female patients were 66 (35.1%). Finally, concluded that there was no association between gender and BT Ring condition, because the value of chi-square (0.215) was greater than p value (0.0.5). Similarly, the value of chi-square (0.540) was greater than p value (0.05), which showed that there was no association between gender and B Trophoziate condition. Analysis also showed that there was close association between BT Ring and B Trophoziate condition with each other, because the value of chi-square is (0.000) which is less than p value (0.05). The present study concludes that there is a close association between BT Ring and B Trophoziate conditions. Also, haematological changes in malarial patients caused by Plasmodium vivax were observed. Out of 188 patients, Patients having platelets amount below 150000 were 142 (75.5%), 150000 to 450000 were 45 (23.9%), and above 450000 were 1 (0.5%). Patients having TLC amount below 4000 were 20 (10.6%), 4000 to 11000 were 161 (85.6%), and above 11000 were 7 (3.7%). Patients having MCHC amount below 32 were 36 (19.1%), 32 to 36 were 150 (79.8%), and above 36 were 2 (1.1%). Patients having MCH amount below 27 were 37 (38.8%), 27 to 33 were 111 (59.0%), and above 33 were 4 (2.1%). Patients having MCV range below 80 were 48 (25.5%), 80 to 100 were 138 (73.4%), and above 100 were 2 (1.1%). Out of 121 male patients, patients having RBC range below 5.52 were 51 and 5.52 to 5.90 were 70, while out of 67 female patients, patients having RBC range 3 were 5, below 4.10 were 21 and 4.10 to 5.10 were 41. Out of 111 male patients, patients having HCT range below 40.00 were 61 and 40.00 to 54.00 were 50, while out of 67 female patients, patients having HCT range 36.00 were 40 and 36.00 to 46.00 were 27. Out of 121 male patients, patients having Hb range below 14.00 were 89 and 14.00 to 18.00 were 32, while out of 67 female patients, patients having Hb range 12.00 were 41, 12.00 to 16.00 were 26, and above 16.00 were zero.
Conclusion
Various hematological parameters significantly affected the malaria disease outcome among the studied patients. The presence different hematological parameters should be considered in the management of patients with malaria in the study area. A total of 188 patients having malaria disease were enrolled, in which frequency of male patients were 122 (64.9%) while frequency of female patients were 66 (35.1%). Results indicate that there is no association between gender and BT Ring condition. Similarly, there is no association between gender and B Trophoziate condition. Analysis also showed that there is close association between BT Ring and B Trophoziate condition with each other.
Acknowledgment
The authors are thankful to the administration and faculty Katlang Diagnostic Centre Mardan, Khyber Pakhtunkhwa, Pakistan for supporting and facilitating this research work.
Funding Source
None
Conflict of Interest
The authors declare no conflict of interest.
REFERENCES
- Akbar W, Anwar J, Jamil A, Ali U, Shaheen F, Kaleemullah. Anaemia and thrombocytopenia in malaria: An observational study of 115 patients in Mardan, KPK, Pakistan. Biomedica. 2016;32:25-28.
- Imoru M, Shehu UA, Ihesiulor UG, Kwaru AH. Haematological changes in malaria-infected children in North-West Nigeria. Turkish J Med Sci. 2013;43:838-842.
- Murray CJ, Rosenfeld LC, Lim SS, Andrews KG, Foreman KJ, Haring D, et al. Global malaria mortality between 1980 and 2010: A systematic analysis. The Lancet. 2012;379:413-431.
- Srikanth J, Srinivas S, Krishna C, Ramulu P. Prevalence of thrombocytopenia in a diagnosed case of malaria in rural population of South India. J Dr. NTR Univ Healt Sci. 2012;1:152.
- Erhart LM, Yingyuen K, Chuanak N, Buathong N, Laoboonchai A, Miller RC, et al. Hematologic and clinical indices of malaria in a semi-immune population of western Thailand. American J Trop Med Hyg. 2004;70:8-14.
- Rehman A, Haq I, Asghar M, Afridi GZ, Faisal S. Sero-epidemiological Identification of Dengue Virus in Individuals at District Shangla, Khyber Pakhtunkhwar, Pakistan. J Biomedical Sci. 2020;9:10.
- Birhanu M, Asres Y, Adissu W, Yemane T, Zemene E, Gedefaw L. Hematological parameters and hemozoin-containing leukocytes and their association with disease severity among malaria infected children: a cross-sectional study at Pawe General Hospital, Northwest Ethiopia. Interdis Perspect Infect Dis. 2017;2017:8965729.
- Haroon M, Jan H, Faisal S, Ali N, Kamran M, Ullah F. Dengue outbreak in Peshawar: clinical features and laboratory markers of dengue virus infection. J Infect Pub Health. 2019;12:258-262.
- Beg MA, Sani N, Mehraj V, Jafri W, Khan MA, Malik A, et al. Comparative features and outcomes of malaria at a tertiary care hospital in Karachi, Pakistan. Int J Infect Dis. 2008;12:37-42.
- Ullah I, Ali MU, Ali S, Rafiq A, Sattar Z, Hussain S. Hematological profile of patients having malaria-positive peripheral blood smears: A Cross-sectional study at a diagnostic research center in Khyber Pakhtunkhwa, Pakistan. Cureus. 2018;10:e3376.
- Coelho HCC, Lopes SCP, Pimentel JPD, Nogueira PA, Costa FTM, Siqueira AM. Thrombocytopenia in Plasmodium vivax malaria is related to platelets phagocytosis. PLoS One. 2013;8:e63410.
- Sajjanar A, Dinesh US, Kanbur D, Mane V, Athanikaret V. Hematological parameters in Plasmodium vivax and falciparum malaria-A study at tertiary care centre in North Karnataka. Natl J Lab Med. 2013;2:23-26.
Citation: Faisal S, Akbar MT, Abdulla, Shah H, Qudrat A, Jan F, et al. (2020) Analysis of Hematological Changes and Seroprevalence of Malarial Patients Caused by Plasmodium vivax Using Statistical Tools. J Trop Dis 8:354. doi: 10.35248/2329-891X.20.8.354.
Copyright: © 2020 Shah M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.

