Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- Google Scholar
- SHERPA ROMEO
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review Article - (2021) Volume 9, Issue 6
Adjunct Techniques to Increase Success Rate of Suture Mediated Vascular Closure Devices in Percutaneous Endovascular Procedures: a Technical ReviewArticle
Dennis H Lui, Alexander Cole, Shadeh Parsapour, Syed T Hussain, Martin Malina and Nada Selva Theivacumar*Received: 23-Sep-2021 Published: 14-Oct-2021
Abstract
Objectives: Percutaneous access is now the norm for many endovascular procedures. Suture-mediated closure devices are commonly used for vessel repair after percutaneous access. Incomplete hemostasis after device deployment is not uncommon. Several adjuncts to suture mediated closure have been described, which allow operators to optimise hemostasis, and potentially avoid surgical exposure and repair of the punctured vessel. We review and compare different adjunct techniques to augment hemostasis after suture-mediated vascular closure device deployment.
Methods: We performed a literature search of MEDLINE using a combined search strategy of Mesh terms. Articles documenting adjunct techniques and maneuvers used after suture-mediated closure of 11-25 French arteriotomies in the femoral artery were included and reviewed.
Results: Currently used adjunct techniques may be divided into two categories, compression adjuncts and plugging adjuncts. Compression adjuncts include external pneumatic compression devices, tractional compression techniques and puncture point compression techniques. Plugging adjuncts involve the directed application of hemostatic agents or reinforcing materials against the femoral artery and puncture tract. These adjuncts have demonstrated effectiveness in augmenting hemostasis, albeit in small and heterogeneous studies and series.
Conclusion: Adjunct techniques can be useful for remedying incomplete hemostasis where suture-mediated closure has been partially successful. Although not a replacement for definitive surgical repair for incomplete hemostasis, they can improve the rate of successful vessel repair in percutaneous endovascular procedures. More than one adjunct may be combined to achieve adequate hemostasis in difficult cases.
Keywords
ProGlide; Prostar XL; Percutaneous EVAR; Pledget reinforcement; Angio-seal; Glubran-2 seal
Introduction
Endovascular procedures are increasingly performed via percutaneous puncture of the arterial tree, commonly targeting the common femoral artery. Procedures requiring large-bore catheterization of the femoral artery, such as endovascular aneurysm repair, are also being increasingly performed percutaneously, and randomized controlled trials and meta-analysis showed that this approach is non-inferior to gaining femoral access via surgical exposure [1-3]. Percutaneous Endovascular Aneurysm Repair (PEVAR) with ultrasound guidance for femoral artery puncture has been found to reduce access-related complications, procedure time, length of hospital stay, and increase patient comfort, when compared to performing Endovascular Aneurysm Repair with femoral cut-down (EVAR) [3-6]. As such, current guidelines suggest that percutaneous ultrasound-guided femoral access should be considered for EVAR [7]. Ultrasound guided puncture for percutaneous EVAR is crucial to select calcium and disease free anterior wall of common femoral artery. It also is helpful to avoid lateral wall puncture. However, some practice is required to perform appropriate US guided puncture. Any puncture without US scan may occur through antero-lateral wall or at a diseased segment which will impede successful closure.
During pEVAR, vascular closure devices are inserted into the vessel prior to introduction of the large sheaths and stent delivery systems into the femoral arteries. Paraglide® (Abbott Vascular Inc., Santa Clara, CA, USA) and ProStar XL® (Abbott Vascular Inc., Santa Clara, CA, USA) are the two commonly used Suture Mediated Closure (SMC) devices for this purpose. The success rate of SMC varies in the literature but is generally accepted to be between 75%- 95% [4,8-12]. However, the definition of technical success is not uniform amongst many of the studies evaluating and comparing percutaneous access compared to surgical access. Study bias, and high heterogeneity amongst studies, has precluded meaningful meta-analysis of the existing studies. A cochrane meta-analysis of vascular closure devices examined 10 studies and found a technical failure rate of 6.7% [13]. In this situation, adjunct techniques can be used by the operator to achieve hemostasis, prior to reassessing whether either converting to a surgical cut-down to repair the vessel directly, or performing fascial closure, are necessary.
Different adjunct techniques are reported to be very effective in pEVAR closure when utilized after SMC devices. This review article discusses various adjunct techniques, as well as their benefits and drawbacks, in the setting of large-calibre arterial access after SMC devices have been deployed.
Whilst all of these adjunct methods may benefit patients when deployed promptly by an operator with sufficient experience, plugging adjuncts have been demonstrated by studies to be effective and beneficial in reducing groin cut down, whereas the compression adjunct techniques are not well studied in the literature. To make it more clear which of the mention adjuncts are more beneficial or effective, we have made comments regarding: “femostop is not generally as useful after large bore cannulation of the femoral vessels”, as well as “The effectiveness of these plugging adjuncts is supported by studies as listed above, whereas compression adjuncts are not well-studied in the literature.
Literature Review
A literature search of the MEDLINE database from 2000 to 2020, including Mesh terms, was performed to identify adjunct techniques used with suture mediated VCD. Adjunct techniques were included in this review if they achieved absolute haemostasis after large calibre (>11 French sheath) femoral artery access, as performed for pEVAR or percutaneous Thoracic Aorta Endovascular Aneurysm Repair (pTEVAR). Where available, data on adjunct success rates were included.
Standard deployment of Suture Mediated Closure (SMC) devices
Following percutaneous arterial access (such as for EVAR or TEVAR), the suture mediated closure devices (ProGlide®, Abbott Vascular, Santa Clara, CA, or one Prostar XL® Abbott Vascular, Santa Clara, CA) are deployed routinely with the pre-close technique, as previously described elsewhere [2,6,14-17]. These devices have been used off-label to repair the femoral artery after insertion of sheath sizes up to 25F [18]. Closure of the femoral artery begins with the controlled removal of the EVAR delivery device and sheath, and concomitant tightening of the sutures inserted by the SMC as per instructions for use. The puncture site is assessed for adequate haemostasis before the guide-wire is removed and the sutures are cut. If only partial haemostasis is achieved, the sutures may be left uncut, and adjunct techniques may be utilised by the operator. Our review of the literature identified the following adjunct techniques (Table 1).
| Adjunct technique | Benefits | Drawbacks |
|---|---|---|
| Manual compression | No added cost | Operator/professionals time consumed |
| Longer time to achieve haemostasis | ||
| Longer time on table | ||
| FemoStop® | Low cost | Possible inaccurate compression |
| Can control degree of external pressure | Compression of vessels, nerves | |
| Puncture point compression | Low cost | Can only be used with |
| Equipment is already present on set. | SMC | |
| May be used as conduit for prothrombotic agents. | ||
| Tractional compression | No added cost | Can only be used with |
| Equipment is already present on set. | SMC | |
| Pledget reinforcement | Can be useful to reinforce vascular closure devices used in large-bore puncture sites. | Can only be used with |
| Can deliver immediate haemostasis | SMC | |
| Wire access maintained | Additional cost of pledgets | |
| Gelatin sponge reinforcement | Can deliver immediate haemostasis | Can only be used with SMC |
| Can be useful to close large size puncture sites | Additional cost of gelatin sponge | |
| Wire access maintained throughout | Can compress nearby structures due to expansion [29] | |
| Can become nidus of infection [29] | ||
| May cause hypersensitivity reactions [29] | ||
| Angioseal® augmentation in addition to pre-close with ProGlide | Useful adjunct in failed proglide closure, most commonly with deep CFA’s. | Wire access must be sacrificed |
| Added cost: $200 per 5 devices | ||
| Anchor remains inside the lumen of the vessel. | ||
| Glubran 2 seal® augmentation to 1 proglide | Useful adjunct to a single ProGlide suture, | Added cost |
| Sheath access maintained during administration (8F), | Requires fluoroscopy to confirm extraluminal application | |
| Deployed over low profile sheath |
Table 1: Different adjuncts to Suture Mediated Closure (SMC) device and their benefits and drawbacks.
Plugging adjunct techniques with haemostatic agents
There are several methods and techniques for applying additional haemostatic materials onto or into the puncture site after SMC, as illustrated in Figure 1.
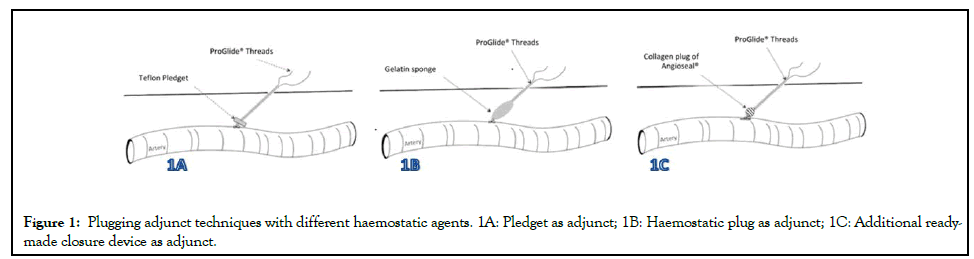
Figure 1: Plugging adjunct techniques with different haemostatic agents. 1A: Pledget as adjunct; 1B: Haemostatic plug as adjunct; 1C: Additional readymade closure device as adjunct.
Pledget reinforcement: This technique described by Theivacumar, et al. [19]. Reinforces the femoral artery puncture site with teflon pledgets to aid haemostasis [19,20]. A square (7.9 mm × 7.9 mm) Teflon Pledget (PTFE Felt Pledgets, Bard®, AZ, USA) is carefully pierced in two places (one at a time) with an 18 G needle, and each pair of sutures from the SMC is passed through the pledget with the help of a needle and the pledget is pushed through the skin puncture site using surgical forceps. The knot pusher is then used to push the Teflon Pledget along the suture to arrive at the puncture site. A second knot is tied over the Teflon pledget, and the pledget is secured over the arterial puncture site by 6 throws. The knot pusher is used after every throw to tighten the knot over the pledget. A single centre retrospective cohort study of 78 patients undergoing pEVAR found that use of this technique after SMC significantly reduced groin complications (4.9% vs 22.5%), and significantly fewer patients required surgical intervention for haemostasis (3.3% vs 14.6%), compared to manual compression only [20].
Gelatin sponge reinforcement: A compressed gelatin sponge (Gelfoam, Upjohn, Kalamazoo, Mich), cut to size (15 mm × 5 mm), has also been described as an adjunct to SMC [21]. The gelatin sponge is railroaded onto the two free ends of each preclose suture via a 19 G needle (one at a time), with all free ends passed through the sponge. Similar to the pledget technique, the needle is removed and the sponge is advanced to the puncture site with a knot pusher and a surgical slipknot is tied to secure the sponge. This reinforcement has been used for persistent oozing at the surgical site after successful suture closure, following 5-7 minutes of manual compression. One case series describes this technique applied gelatin successful in 23 patients with partial haemostasis after deployment of SMC (9 patients with femoral punctures>18 Fr). Doppler ultrasound was performed after this adjunctive technique which confirmed no immediate vascular complications [21].
Angio-Seal VIP®: The Angio-Seal VIP (Terumo Medical Corporation, Somerset, NJ, USA) VCD is an effective collagenbased VCD in its own right. The device consists of a polymer anchor deployed intraluminally against the intima of the vessel, and an external collagen plug fastened together with a suture; the materials are bioabsorbable and dissolve within 90 days. The Angio-Seal device can be used for repairing up to 8 French sheath size access under its instructions for use, but reports have demonstrated efficacy and safety in repairing vessel access up to 12 French size. However, it can also be deployed as an adjunct to ‘augment’ the preclose technique with Perclose ProGlide suture mediated VCD [22]. If the preclose technique partially repairs the vessel, but fails to achieve adequate haemostasis, and the guidewire has not been removed yet, 8 French or 6 French size Angio-seal de-vice is guided into the vessel over the guidewire. Care is taken not to disrupt the sutures or the knots from the preclose, and where the larger 8 French device does not enter the vessel easily, a 6 French device must be applied instead. Patel, et al. describes this maneuver with the Angio-Seal device to augment the repair in a small cohort of pEVARs who had failed primary repair with pre-close suture mediated VCD [23,24]. Successful haemostasis was achieved in 96% of these patients after Angio-Seal was deployed as an adjuvant device.
Glubran-2 Seal®: The Glubran-2 seal device (GEM Srl, Viareggio, Italy) has been used as an adjunct to a single ProGlide in thoracoabdominal aortic aneurysms and TAVI procedures with 16 French to 24 French sheath sizes in the femoral artery [24]. Glubran-2 is biodegradable cyanoacrylate glue with adhesive and haemostatic properties. The ProGlide knot is care-fully advanced around an 8F sheath to reduce the arteriotomy size. Subsequently the Glubran-2 seal device is advanced on the introducer sheath to the arterial wall and contrast medium is injected into the device. Fluoroscopy is required to confirm the extra-luminal position of the seal device to avoid embolisation. Glue is then injected into the subcutaneous tissue surrounding the arteriotomy, which polymerises into a thin elastic film that adheres to the local tissue anatomy. Finally, the introducer and sheath wire are then removed with external compression applied for full haemostasis. A single SB-VCD and glubran-2 technique has been used in percutaneous Aortic Valve Implantation (pAVI) and Thoracoabdominal Aneurysm Repair (TAAR) [24]. A combined total of 250 procedures the glubran adjunct technique was successful in 98.4% of cases. Once haemostasis is achieved, the skin can be closed according to surgeon preference such as skin glue.
Compression adjunct techniques
Apart from external manual compression of the puncture site, there is different way of exerting pressure over the puncture sites as illustrated in Figure 2A.
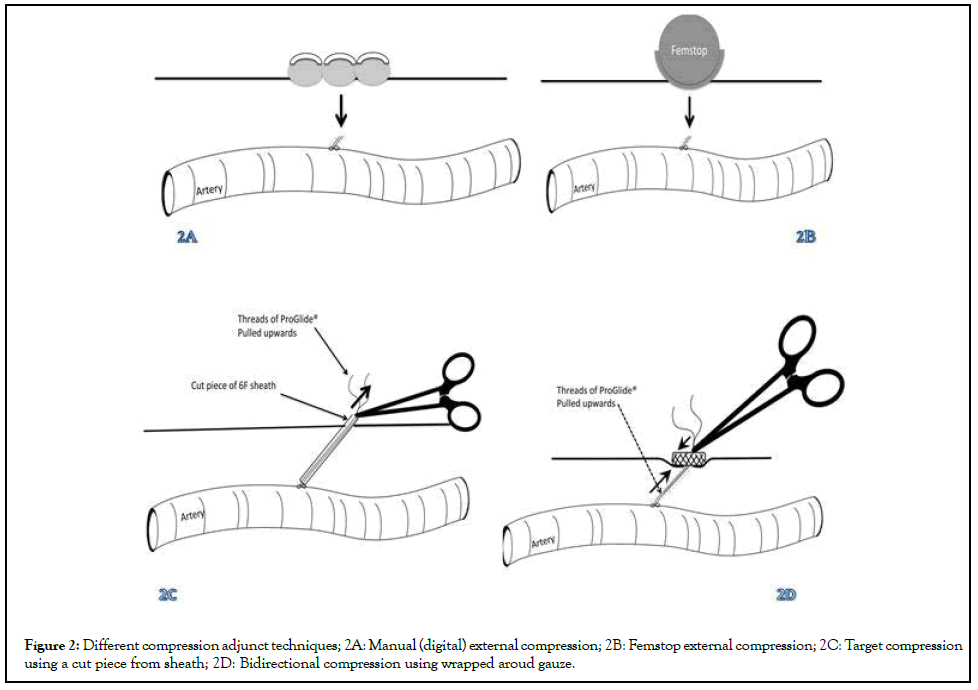
Figure 2: Different compression adjunct techniques; 2A: Manual (digital) external compression; 2B: Femstop external compression; 2C: Target compression using a cut piece from sheath; 2D: Bidirectional compression using wrapped aroud gauze.
Femostop external compression device: The Femostop (Abbott Cardiovascular, Plymouth, MN, USA) device is a pneumatic, externally applied compression device to improve haemostasis (Figure 2B). It performs the role of external manual compression by way of a stiff plastic rig and inflatable plastic half-sphere. A strap is placed underneath the patient’s hips and attached to the device, and the half-sphere is manually inflated to the desired pressure against the puncture site. This inexpensive device has been shown to be as effective as manual compression or vascular closure devices [25-27]. However, prolonged pressure on the groin can give discomfort to patients, and the device is prone to being dislodged or misaligned by patient movements. The published experience in the literature regarding this haemostatic device largely revolves around its application after smaller calibre femoral access, especially with interventional cardiology procedures. A prospective study of 150 patients undergoing coronary interventions via femoral access demonstrated that femostop is as effective at achieving haemostasis, albeit slower, compared to the Angioseal in this setting [26]. Use of the Femostop is not appropriate after large-bore cannulation of the femoral arteries.
Puncture point compression: In addition to pledget or gelatin sponge reinforcement, puncture point compression can augment the haemostasis of suture based closure devices prior to cutting the sutures. Transparent tubing cut from the injection port of any vascular access sheath can be guided over all free suture ends [10]. Alternatively, a 6F sheath with the hub removed by scissors can be used. This tubing is threaded to the base of the suture, and is subsequently clamped with a haemostat at the end furthest from the vessel (Figure 2C). This technique applies pressure to the knot and is secured for 5-10 minutes to aid haemostasis. The teflon pledge/gelatin sponge technique can also be applied prior to using puncture point compression to enhance haemostasis at the arteriotomy site, or alternatively 1 to 2 mL of thrombin may be injected into the tubing to track down to the puncture site. This technique has been used in 18 patients undergoing a pEVAR procedure, with a 100% technical success rate and no subsequent access related complications [10].
Tractional compression: If absolute haemostasis is not yet achieved, then tractional compression can be applied instead of the traditional unidirectional manual compression or application of an external compression device. A small gauze swab is wound around the closure-device sutures, and subsequently compressed downwards towards the puncture site following the path of the sutures. The bulk of the swab remains outside the body. The sutures are held taught, per-pendicular to skin. A clip is then applied to the tensioned sutures whilst they are sandwiched between the swab, to prevent damaging the suture. The resulting effect is to pull the vessel up onto the swab, while the swab is held down by forceps to compress the puncture site for a period of time that would mirror the application of manual compression (Figure 2D). The clip is then released, the swab removed, and the sutures cut once haemostasis is achieved.
Discussion
Failure of vascular closure devices following percutaneous femoral access increases patient morbidity and discomfort. As endovascular procedures are being performed increasingly with percutaneous access, and approximately 6%-7% of VCD deployments fail, adjunct maneuvers are useful for operators to become familiar with, in order to deal with incomplete haemostasis. The adjunctive procedures presented herein carry the potential to reduce the need for immediate or subsequent groin cut down, fascial closure, or prolonged manual compression. When delivered promptly, they may reduce the risk of development of groin complications such as iatrogenic pseudoaneurysm (which can arise in 2%-7% of patients with antiplatelet therapy undergoing endovascular procedures via a femoral approach) [28]. A pseudoaneurysm can form when insufficient haemostasis allows a haematoma to form with active extravasation from the puncture site, which in turn prevents platelet aggregation and sealing of the intima of the punctured vessel. These pseuoaneurysms often necessitate close doppler surveillance, or treatment with direct pressure, thrombin injection, stenting, or surgical repair, all of which increase inpatient stay and discomfort. Along with careful patient selection, consideration of risk factors, and pre-emptive planning for potential access-related complications, these techniques may provide operators with more tools to achieve success haemostasis after percutaneous cases.
The techniques described are limited to reinforcing closure with SMC such as ProGlide®/ProStar XL®. Successful initial deployment of the suture-mediated closure device is required, followed by the subsequent adjunct interventions if inadequate haemostasis is present. An additional ready-made closure device such as third ProGlide® or Angioseal® can be used, or any haemostatic plug/ pledgets can be applied as adjuncts to increase the success rate of SMC closure device. It is not possible to compare different techniques for their outcome as there are no studies comparing different techniques. For the time being, it is reasonable to assume that any method an operator comfortable with can be used increase haemostasis following percutaneous techniques. The usage of additional closure device or haemostatic plugs/pledgets is diagrammatised in Figure 1. Once satisfactory haemostasis is obtained with the closure device and adjuncts, a period of manual compression of varying length may be required, depending on the patient and risk factors (including anticoagulation, antiplatelets, anatomy, body habitus). Additional compression adjuncts to manual compression are diagrammatised in Figure 2.
The placement of additional plugging agents, such as teflon pledgets or gelatin sponge, Angioseal VIP or Glubran-2, forms one strategy to help achieve haemostasis. The effectiveness of these plugging adjuncts is supported by studies as listed above, whereas compression adjuncts are not well-studied in the literature. Complications associated with these plugging adjuncts are rare, but theoretically include infection, embolisation of injectable substances into the vessel, and allergic reaction [29]. Although there is an added cost of using these adjuncts ($100 US dollars for 10 pledgets, $190 for Angioseal closure device), the cost is fractional compared to the SMC, and furthermore the reduction in length of inpatient stay, patient discomfort, and improved patient mobilisation make this cost easily justifiable. Availability of these devices in the operating room or angiography suite may pose an issue. Teflon pledgets and thrombin are more readily available in most operating rooms, hybrid theatres, and angiography suites. However, gelatin sponge, Angioseal, and Glubran-2 may not be stocked depending on each vascular and interventional radiology department. The advantages and disadvantages of all these adjuncts are summarized in Table 1.
The application of the Angioseal device and Glubran-2 after SMC have specific considerations and limitations. In particular, Glubran-2 must be used with fluoroscopy to ensure the polymer is delivered external to the vessel. It adds an extra step where the image intensifier may already be moved out of position during deployment of the suture mediated VCD. The Angioseal device requires the operator to lose wire access during deployment. Should the deployment still fail to achieve absolute haemostasis, options would become limited to direct pressure, and failing that surgical exploration [30].
Adjunct compression techniques to manual include Femostop® external compression, puncture point and tractional. Manual compression requires additional operator time and a longer time to haemostasis compared to other techniques, but it is reliable. External compression devices (such as Femostop®) may narrow the arterial lumen, particularly if high pneumatic pressure is used. External compression also has the potential to deliver inaccurate pressure, or impinge neighbouring structures such as the femoral nerve, branches thereof, or the common femoral vein. When applied post-procedurally in the conscious patient, they may also serve as a considerable source of discomfort, and patient movement or transfer may disrupt the FemoStop device rendering it ineffective. The tractional compression and puncture point techniques allow focal application of pressure to the puncture site without restricting the arterial lumen or compromising neighbouring structures. The use of these techniques may also be particularly valuable for distal punctures that lack the underlying bony stability of the femoral head, against which the common femoral artery is traditionally compressed. Furthermore, both techniques can be carried out using equipment readily available in theatres during EVAR procedures or any other endovascular procedures with SMC as closure devices. Again, its use is limited as an adjunct to suture mediated closure devices and cannot be incorporated once the sutures are cut.
For any closure devices with adjunct techniques to work better, appropriate puncture and pre-closure deployment is necessary. We recommend US guided puncture as we believe that ultrasound guided puncture for percutaneous EVAR is crucial to select a disease free anterior wall of common femoral artery segment to be punctured. It also is helpful to avoid lateral wall puncture. However, some experience is required to perform appropriate US guided puncture. Any puncture without US scan may occur through anterolateral wall or at a diseased segment which will impede successful closure. Puncturing under or above inguinal ligament should be avoided as this is likely to fail to tighten the knot of the closure device and it will prevent any adjunct pledgets or plugs tracking towards the puncture site.
Conclusion
Adjunct techniques for suture based percutaneous arterial closure have a useful role for assisting with achieving haemostasis in large sheath punctures, where correct deployment of vascular closure devices fail to achieve absolute haemostasis. When applied with careful reversal of heparin, usage of additional haemostatic plugs/ pledgets and adjunct compression techniques (tractional or puncture point compression) discussed above may be successful in securing adequate haemostasis in percutaneous femoral access. These adjunct techniques could in turn reduce patient discomfort, procedure time, and length of patient stay in hospital. Patient selection and operator experience with vascular closure devices are key factors for success, and although these adjunct techniques may increase the success of these percutaneous procedures, they do not replace the role of surgical exposure in the event of incomplete haemostasis. Further comparative studies of these adjuncts are required in order to reveal the relative benefits, and potential complications.
REFERENCES
- Torsello GB, Kasprzak B, Klenk E, Tessarek J, Osada N, Torsello GF. Endovascular suture versus cutdown for endovascular aneurysm repair: A prospective randomized pilot study. J Vasc Surg. 2003; 38 (1): 78-82.
- Nelson PR, Kracjer Z, Kansal N, Rao V, Bianchi C, Hashemi H, et al. A multicenter, randomized, controlled trial of totally percutaneous access versus open femoral exposure for endovascular aortic aneurysm repair (the PEVAR trial). J Vasc Surg. 2014; 59 (5): 1181-1193.
- Gimzewska M, Jackson AI, Yeoh SE, Clarke M. Totally percutaneous versus surgical cut‐down femoral artery access for elective bifurcated abdominal endovascular aneurysm repair. Cochrane Database Syst Rev. 2017: 2.
- Malkawi AH, Hinchliffe RJ, Holt PJ, Loftus IM, Thompson MM. Percutaneous access for endovascular aneurysm repair: A systematic review. Eur J Vasc Endovasc Surg. 2010; 39 (6): 676-682.
- Huff CM, Silver MJ, Ansel GM. Percutaneous endovascular aortic aneurysm repair for abdominal aortic aneurysm. Curr Cardiol Rep. 2018; 20 (9): 1-5.
- Hajibandeh S, Hajibandeh S, Antoniou SA, Child E, Torella F, Antoniou GA. Percutaneous access for endovascular aortic aneurysm repair: A systematic review and meta-analysis. Vasc. 2016; 24 (6): 638-648.
- Wahainen A, Verzini F, Van Herzeele I, Allaire E, Bown M, Cohnert T. European society for vascular Surgery (ESVS) 2019 clinical practice guidelines on the management of abdominal aortoiliac artery aneurysm. Eur J Vasc Surg. 2019; 57.
- Biancari F, Romppanen H, Savontaus M, Siljander A, Mäkikallio T, Piira OP, et al. MANTA versus ProGlide vascular closure devices in transfemoral transcatheter aortic valve implantation. Int J Cardiol. 2018; 263: 29-31.
- Karaolanis G, Kostakis ID, Moris D, Palla VV, Moulakakis KG. Fascia suture technique and suture-mediated closure devices: Systematic review. Int J Angiol. 2018; 27 (1): 13-22.
- Furlough CL, Desai SS, Azizzadeh A. Adjunctive technique for the use of ProGlide vascular closure device to improve hemostasis. J Vasc Surg. 2014; 60 (6): 1693-1694.
- Ashrafi M, Al-Jarrah Q, Anandarajah M, Ashleigh R, Welch M, Baguneid M. Single center experience following the introduction of a percutaneous endovascular aneurysm repair first approach. Angiology. 2017; 68: 119-123.
- Jaffan AAA, Prince EA, Hampson CO, Murphy TP. The preclose technique in percutaneous endovascular aortic repair: A systematic literature review and meta-analysis. Cardiovasc Intervent Radiol. 2013; 36: 567-577.
- Robertson L, Andras A, Colgan F, Jackson R. Vascular closure devices for femoral arterial puncture site haemostasis. Cochrane Database Syst Rev. 2016; 3: CD009541.
- Griese DP, Reents W, Diegeler A, Kerber S, Babin-Ebell J. Simple, effective and safe vascular access site closure with the double-ProGlide preclose technique in 162 patients receiving transfemoral transcatheter aortic valve implantation. Catheter Cardiovasc Interv. 2013; 82: E734-741.
- Lee WA, Brown MP, Nelson PR, Huber TS. Total percutaneous access for endovascular aortic aneurysm repair (“Preclose” technique). J Vasc Surg. 2007; 45 (6): 1095-1101.
- Teh LG, Sieunarine K, Van Schie G, Goodman MA, Lawrence-Brown M, Prendergast FJ, et al. Use of the percutaneous vascular surgery device for closure of femoral access sites during endovascular aneurysm repair: Lessons from our experience. Eur J Vasc Endovasc Surg. 2001; 22 (5): 418-423.
- Dosluoglu HH, Cherr GS, Harris LM, Dryjski ML. Total percutaneous endovascular repair of abdominal aortic aneurysms using Perclose ProGlide closure devices. J Endovasc Ther. 2007; 14: 184-188.
- Starnes BW, Andersen CA, Ronsivalle JA, Stockmaster NR, Mullenix PS, Statler JD. Totally percutaneous aortic aneurysm repair: Experience and prudence. J Vasc Surg. 2006; 43: 270-276.
- Theivacumar NS, Glasgow S, Najem M, Qureshi MI. Pledget reinforcement and bidirectional compression as adjunctive techniques for suture-based closure of arterial cannulation sites in percutaneous endovascular aneurysm repair. Ann R Coll Surg Engl. 2020; 102: 636-637.
- Theivacumar NS, Qureshi MI, Glasgow S, Najem M. Pledget reinforcement and traction compression as adjunctive techniques for suture-based closure of arterial cannulation sites in percutaneous endovascular aneurysm repair: Initial experience. J Vasc Surg Cases Inn Tech. 2021; 7: 183-187.
- Najem M, Martin G, Patrone L, Malina M, Theivacumar NS. Pledget reinforcement and tractional compression as adjunctive techniques for Suture-Mediated Closure (SMC) in Percutaneous Endovascular Aneurysm Repair (pEVAR): A retrospective observational cohort study. Ann Vasc Surg 2021.
- Pua U. Application of gelatin sponge sandwich as a hemostatic aid to percutaneous suture-mediated arteriotomy closure. J Vasc Surg. 2013; 57: 583-585.
- Chaudhuri A. Femoral arterial haemostasis using an anchored collagen plug after percutaneous evar with an ultra-low profile device: Prospective audit of an evolving “Post-Close” technique. Eur J Vasc Endovasc Surg. 2017; 54: 241-246.
- Patel R, Juszczak MT, Bratby MJ, Sideso E, Anthony S, Tapping CR, et al. Efficacy and safety of augmenting the preclose technique with a collagen-based closure device for percutaneous endovascular aneurysm repair. Cardiovasc Intervent Radiol. 2015; 38: 821-826.
- Sorropago G, Singh G, Sorropago A, Sole A, Rossi J, Tolva VS, et al. A new percutaneous technique for effective vascular access site closure in patients undergoing transfemoral aortic valve implantation and thoraco-abdominal aortic aneurysm rEpair: The PASTE study. EuroIntervention. 2018; 14: e1278–1285.
- Walker SB, Cleary S, Higgins M. Comparison of the FemoStop device and manual pressure in reducing groin puncture site complications following coronary angioplasty and coronary stent placement. Int J Nurs Pract. 2001; 7: 366-375.
- Amin FR, Yousufuddin M, Stables R, Shamim W, Al-Nasser F, Coats AJ, et al. Femoral haemostasis after transcatheter therapeutic intervention: A prospective randomised study of the angioseal device vs the femostop device. Int J Cardiol. 2000; 76: 235-240.
- Juergens CP, Leung DYC, Crozier JA, Wong AM, Robinson JTC, Lo S, et al. Patient tolerance and resource utilization associated with an arterial closure versus an external compression device after percutaneous coronary intervention. Catheter Cardiovasc Interv. 2004; 63: 166-170.
- Webber GW, Jang J, Gustavson S, Olin JW. Contemporary management of post-catheterization pseudoaneurysms. Circulation. 2007; 115: 2666-2674.
- Tompeck AJ, Gajdhar AUR, Dowling M, Johnson SB, Barie PS, Winchell RJ, et al. A comprehensive review of topical hemostatic agents: The good, the bad, and the novel. J Trauma Acute Care Surg. 2020; 88: e1-e21.
Citation: Lui DH, Cole A, Parsapour S, Hussain ST, Malina M,Theivacumar NS (2021) Adjunct Techniques to Increase Success Rate of Suture Mediated Vascular Closure Devices in Percutaneous Endovascular Procedures: A Technical Review Article. J Vasc Med Surg. 9: 435.
Copyright: © 2021 Lui DH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

