Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
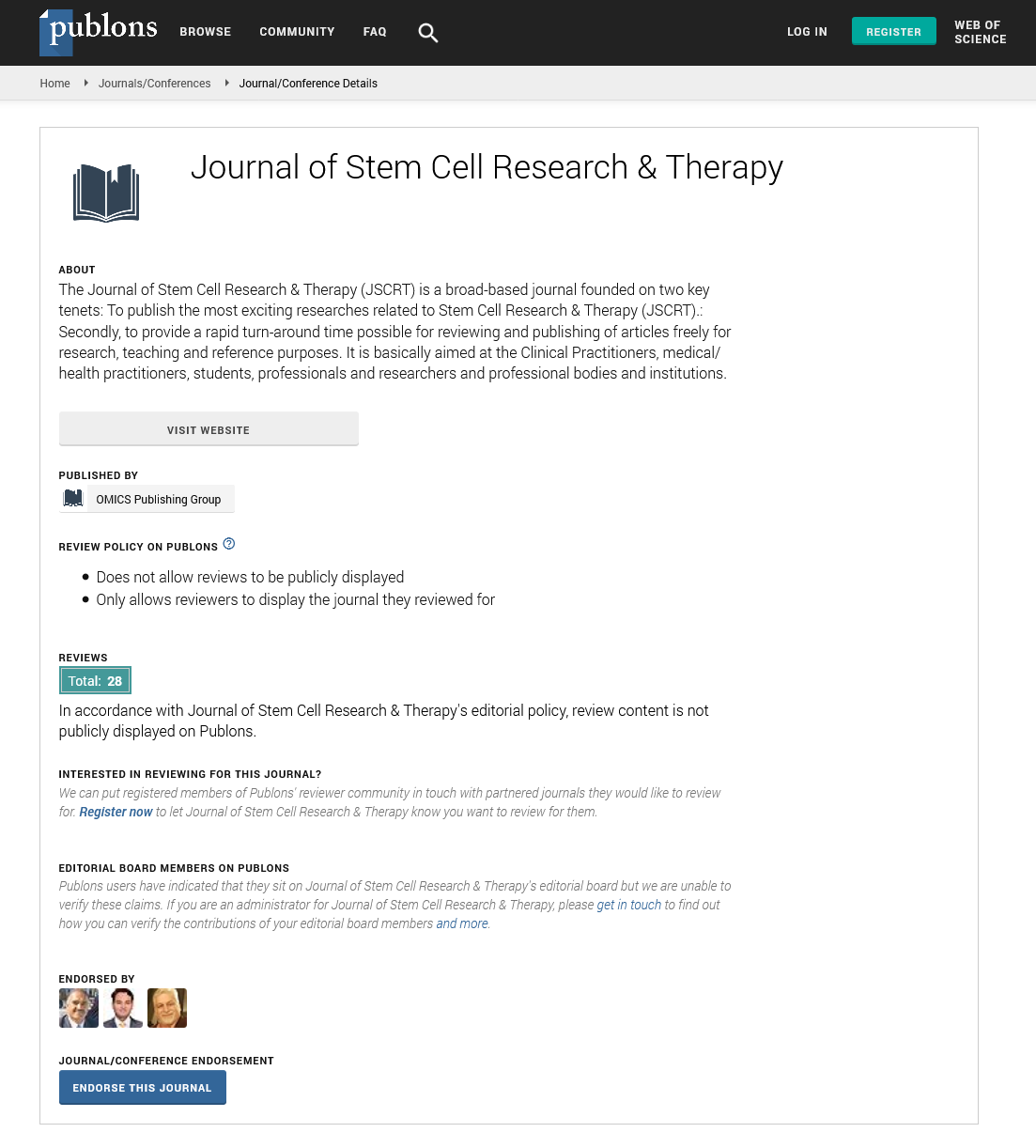
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Perspective - (2022) Volume 12, Issue 12
Actions of Non-compliance in Heart Failure Patients
Van Jaarzsma*Received: 22-Nov-2022, Manuscript No. JSCRT-22-19384; Editor assigned: 25-Nov-2022, Pre QC No. JSCRT-22-19384(PQ); Reviewed: 09-Dec-2022, QC No. JSCRT-22-19384; Revised: 16-Dec-2022, Manuscript No. JSCRT-22-19384; Published: 23-Dec-2022, DOI: 10.35248/2157-7633.22.12.571
Description
Compliance has long been seen as a significant problem in the healthcare industry. An important standard work on compliance in healthcare. Compliance is still a major issue in chronic disease today, and patients with Heart Failure (HF) are no exception. Most HF patients now have to follow a complex regimen as a result of better treatment alternatives. According to the HF recommendations of the American Heart Association/American College of Cardiology (AHA/ACC) and the European Society of Cardiology (ESC), a variety of medications (ACE-inhibitors, diuretics, beta-blockers, spironolactone, and digoxin) are advantageous for HF patients and should therefore be prescribed. It is requested that non-pharmacological lifestyle adjustments such as fluid- and sodium-restriction, daily weighing, exercise modification, influenza vaccination, smoking cessation, and alcohol consumption restriction be made. Numerous authors are aware of the issue of non-compliance in HF, yet the majority of papers only address medication compliance while ignoring other significant lifestyle changes. There is also little knowledge about the strategies that have been tried and are effective at raising patient compliance.
The repercussions of non-compliance in HF patients, the level of compliance with the various components of the treatment regimen, and methods to increase compliance in HF patients are all included in this comprehensive literature review. Despite reviews on compliance in heart failure and cardiovascular disease, this study focuses more on the various components of compliance with the heart failure-associated regimen (for instance, compliance with medication, diet, and daily weighing) and on variables connected to non-compliance. Compliance is the degree to which a person follows the clinical prescription when it comes to taking medication, eating a healthy diet, or changing their lifestyle. Although other words like adherence, therapeutic relationship, and concordance are often used to describe the same situation, the term compliance is still frequently employed despite its negative connotation of a oneway communication from the describing healthcare provider to the obeying patient. The term compliance is now frequently used in a new context, referring to a scenario in which the patient and healthcare professional have a mutually respectful and cooperative relationship.
Self-report questionnaires or patient interviews are frequently used to measure compliance. A doctor interview, a record review, a Medication Event Monitoring System (MEMS), a measurement of serum ACE activity or drug concentration, a pill counter, patient diaries, and a measurement of medication concentration are additional instruments. A multidisciplinary intervention with a focus on teaching and counselling during hospitalisation, at home, and via telephone follow-up was able to increase medication compliance. After a nurse-led HF clinic intervention, daily weighing significantly improved after 12 months and fluid restriction compliance significantly improved after 3 months. In this study, there was no significant difference in compliance with fluid restriction between the intervention group (50%) and the control group (28%), after 12 months. There was no appreciable difference in the compliance with fluid restriction of the intervention group (50%) and the control group (28%) after 12 months in this trial. Patients who adhered to their diet plans increased during an intervention that included frequent interaction at the HF clinic and via phone. In three more randomised studies, patients received one or more sessions of medication education from a pharmacist. In every study, the intervention group's medication compliance increased significantly. However, in one study, self-reported compliance levels after 6 months showed no significant change, yet in a small population (n=23), 10 patients in the intervention group compared to three in the control group filled their prescriptions on time.
Sending educational materials and keeping daily phone or video contact with HF patients to remind them to take their medicine as directed are two more effective randomised studies. Nonrandomized studies occasionally report the outcomes of the aforementioned randomised studies, however compliance with some interventions is still low even after thorough teaching. A nurse-led intervention at the HF clinic improved patients' knowledge of sodium restriction, yet only 35% of patients consistently avoid salty meals, and only 52% of patients read food labels. In the West trial, participants received education regarding Heart Failure (HF) and the HF-related regimen during a visit to the HF clinic and during frequent telephone follow-up over a six-month period. This study, patients who received organised education about their diets saw a reduction in their self-reported sodium intake. A considerable reduction in fluid and sodium intake was the consequence of dietician-led education on diet and sodium restriction. A modest trial found that 75% of HF patients who received a home telemonitoring intervention adhered to daily weight guidelines.
Citation: Jaarzsma V (2022) Actions of Non-compliance in Heart Failure Patients. J Stem Cell Res Ther. 12:571.
Copyright: © 2022 Jaarzsma V. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.