Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
- Google Scholar
- SHERPA ROMEO
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2023) Volume 11, Issue 3
A Rare Case of Simultaneous Acute Embolic Occlusions of the Right Upper and Lower Extremity, Recanalized with Endovascular Thrombectomy
Stanislav Kernov* and Ivan MartinovReceived: 08-May-2023, Manuscript No. JVMS-23-21262; Editor assigned: 11-May-2023, Pre QC No. JVMS-23-21262 (PQ); Reviewed: 30-May-2023, QC No. JVMS-23-21262; Revised: 06-Jun-2023, Manuscript No. JVMS-23-21262 (R); Published: 13-Jun-2023, DOI: 10.35248/2329-6925.23.11.517
Abstract
Acute thromboembolic events are limb-threatening complications, necessitating immediate treatment. Endovascular Thrombectomy (EVT) can be a simple, safe and well-tolerated treatment modality for patients with acute limb ischemia. We report a clinical case of EVT of acute simultaneous embolism of the right upper and lower extremity, which occurred in the settings of atrial fibrillation and long-term oral anticoagulation with Edoxaban. A 74-year-old female patient was admitted to our department, because of sudden onset of numbness, coldness and weakness of right upper and lower extremities. The main factor that can improve survival of patients with acute limb ischemia is early aggressive treatment aimed at restoring the patency of occluded arteries. Faced with the threat of the both limbs loss, the patient underwent simultaneous endovascular thrombectomy with AngioJet ® thrombectomy system (Boston Scientific) and could remove the clots, despite of distal embolization. The patient was discharged after a 3-day hospital stay. The most common cause of acute extremity ischemia is emboli from a cardiac source. When acute embolism occurs, it first manifests are sensory deficit, followed by a motor deficit and muscle weakness. Endovascular thrombectomy can be a simple, safe and well-tolerated treatment modality for patients with Acute Limb Ischemia (ALI). The AngioJet ® system creates a local low-pressure zone to entrain, fragment, and aspirate thrombi with the Venturi-Bernoulli's principle of fluid dynamics. However, this treatment should be performed in very experienced centers with this endovascular technique in different vascular territories and with full access to vascular surgical intervention in case of a failed endovascular approach. Knowledge of such cases is essential in order to create specific protocols for prophylaxis of thrombotic events and giving the priority to endovascular treatment over direct surgery due to its milder invasiveness and shortened hospital stay.
Keywords
Cardiogenic embolism; Simultaneous embolic occlusions; Endovascular thrombectomy; Jet stream
Abbreviations
EVT: Endovascular Thrombectomy; ABI: Ankle-Brachial Index; IU: International Unit; SFA: Superficial Femoral Artery; PFA: Profunda Femoral Artery; PTA: Percutaneous Transluminal Angioplasty; Fr: French; INR: International Normalised Ratio; q.d.: Quaque Die; ALI: Acute Limb Ischemia
Introduction
Acute peripheral arterial events can lead to high case fatality risk and severe functional disability if emergency endovascular or surgical intervention is not performed. Moreover, cardiac events are more likely to cause upper extremity ischemia due to the formation of mural thrombi [1].
Endovascular revascularization for acute simultaneous embolic occlusive lesions of the right brachial, femoral and popliteal artery has not been established, and reports of concomitant EVT are not published.
The priority should increasingly be given to endovascular treatment over direct surgery due to its milder invasiveness and shortened hospital stay. We performed simultaneous EVT with AngioJet® thrombectomy system (Boston Scientific) and could remove the clots, despite the occurrence of distal embolizations. The AngioJet system creates a local low-pressure zone to entrain, fragment, and aspirate thrombi with the Venturi-Bernoulli's principle of fluid dynamics. Multiple high-velocity, high-pressure saline jets which are introduced through orifices in the distal tip of the catheter to create a localized low-pressure zone, resulting in a powerful vacuum effect ( ~ 600 mmHg) with the entrainment and dissociation of bulky thrombus [2]. The minimum vessel diameter in which the AngioJet can be used is 2 mm, and maximum - 20 mm, whereas catheters with up to 140 cm effective length are available.
Case Presentation
We present a 74-year-old female patient (156 cm tall, weighed 52 kg, BMI = 21.4 kg/m) who was admitted to our department, because of numbness, coldness and weakness of right upper and lower extremities.
At 09:30 p.m. on 10th of March 2023, she suddenly noted numbness, coldness, and weakness of the right upper extremity. At 6:30 a.m. on the 11th of March - the day of admission, she felt the same signs at the right lower extremity.
The patient had medical history of paroxysmal nonvalvular atrial fibrillation, on therapy with oral anticoagulant Edoxaban 30 mg q.d., due to low body weight (52 kg). Other concomitant diseases were arterial hypertension and dyslipidemia. She had no history of smoking. Her familial history included stroke in the grandmother on the maternal side.
Findings on admission
The blood pressure was 131/77 mmHg (measured in the left upper extremity, unmeasurable in the right upper extremity), an irregular heart rate of 87 bpm. Body temperature was 36.6°C. The consciousness was clear, and no impairment was noted in higher brain functions or the nervous system. There was mild paralysis in the right upper extremity, but no laterality was noted in superficial sensation. The pulses of the right brachial, radial, ulnar; the right popliteal and tibial arteries were markedly attenuated, and the right extremities felt cold and numb.
ABI right=0/ABI left = 1.1 (Ankle-Brachial Index: ABI)
Diagnostic angiography
The patient received loading doses of dual antiplatelet therapy of Clopidogrel 600 mg p.o. and Acetylsalicylic acid 300 mg p.o. before the procedure. An intra-arterial bolus dose of Heparin (5000 IU) was administrated after sheath insertion and continued at 1000 U/h during the procedure.
The angiography was performed viathe left common femoral artery. The diagnostic catheterization of the right upper limb showed a thrombus in the origin of right brachial artery, second level of thrombosis in the brachial bifurcation into its ulnar and radial branches, and poor distal filling of the radial artery (Figures 1a and 1b).
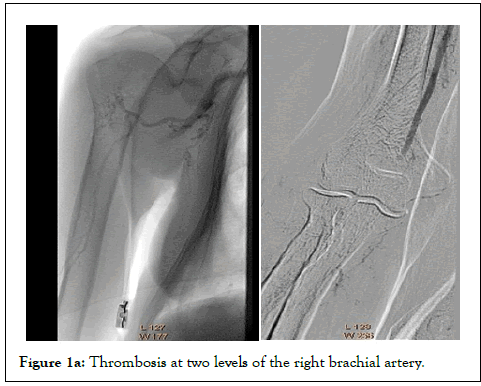
Figure 1a: Thrombosis at two levels of the right brachial artery.
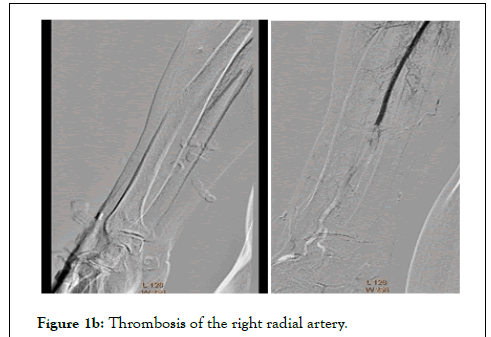
Figure 1b: Thrombosis of the right radial artery.
The diagnostic catheterization of the right lower extremity showed a “riding” thrombus at the bifurcation of Superficial Femoral Artery/ Profunda Femoral Artery (SFA/PFA) and long thrombotic occlusion starting from the middle segment of SFA, involving the popliteal artery and tibiofibular trunk (Figures 2a and 2b). In the settings of simultaneous acute Critical Limb Ischemia (CLI) of the right upper and lower limbs, we performed Ad hoc concomitant percutaneous transluminal thrombectomy.
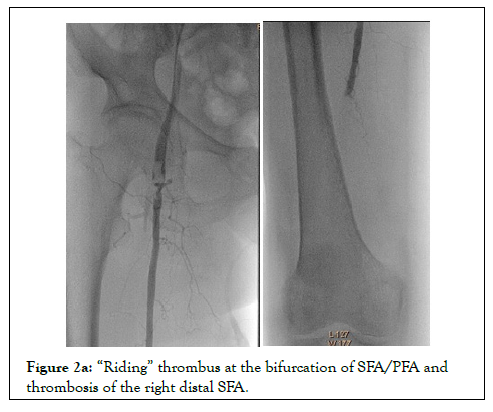
Figure 2a: “Riding” thrombus at the bifurcation of SFA/PFA and thrombosis of the right distal SFA.

Figure 2b: Thrombosis of the right tibiofibular trunk.
PTA of the right upper extremity
An introducer sheath Fortress 6 Fr/90 cm (Biotronik) was placed at the right subclavian artery (Figure 3). Recanalization with 0.018" Glidewire Advatage (Terumo) and Trail Blazer Angled Support Catheter (Medtronic) (Figure 4). Balloon dilatations with Passeo-182/120 mm (Biotronik) and Passeo-183/120 mm without effect (Figures 5a and 5b). After that 0.014" Fielder wire (Asahi) was placed to the palmar arch. Thrombaspiration of red thrombotic masses with Eliminate aspiration catheter 6 Fr (Terumo). Again, no distal flow.
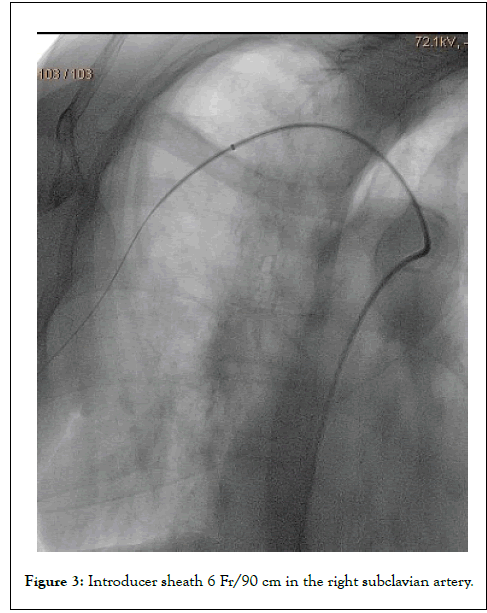
Figure 3: Introducer sheath 6 Fr/90 cm in the right subclavian artery.
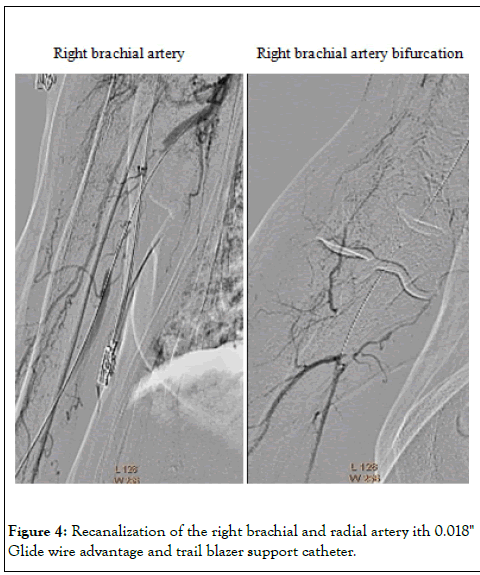
Figure 4: Recanalization of the right brachial and radial artery ith 0.018" Glide wire advantage and trail blazer support catheter.

Figure 5a: PTA - balloon dilatations of the right radial and brachial artery.
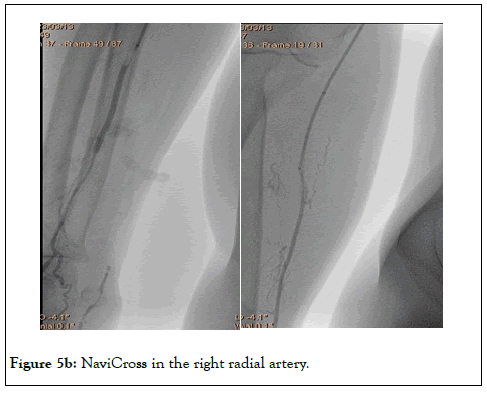
Figure 5b: NaviCross in the right radial artery.
Then 0.035" Storq wire (Cordis) was placed in the right radial artery. Effective endovascular trombectomy with AngioJet Solent Omni (2.06 mm) was performed - first in the right brachial artery, and then in the axillary artery (Figure 6). The brachial artery was successfully recanalized, but distal embolization in the brachial artery bifurcation occurred again. We repeated the EVT with the same AngioJet Solent Omni (2.06 mm) in the brachial and radial arteries. Blood flow was Figure 1a: Thrombosis at two levels of the right brachial artery. restored in right brachial and radial arteries (Figures 7a and 7b).
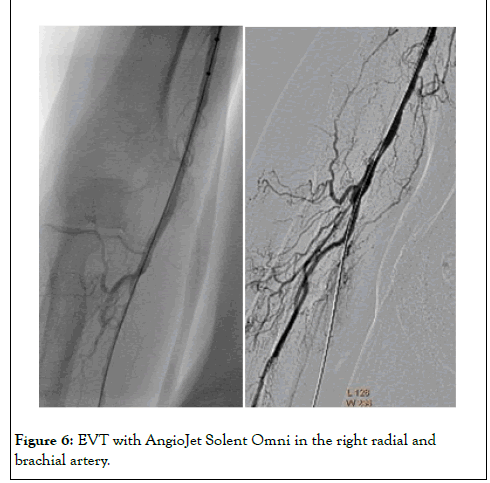
Figure 6: EVT with AngioJet Solent Omni in the right radial and brachial artery.
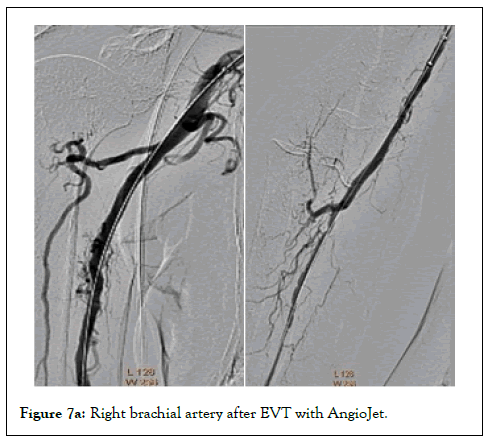
Figure 7a: Right brachial artery after EVT with AngioJet.
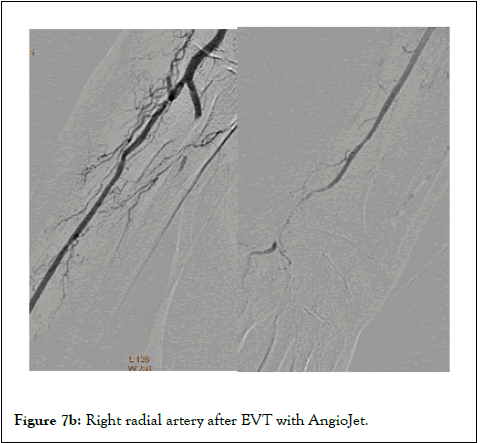
Figure 7b: Right radial artery after EVT with AngioJet.
PTA of the right lower extremity
The same introducer was redirected with tip in the right common femoral artery. PTA of the right SFA, PFA, popliteal and posterior tibial arteries was performed. Recanalization with 0.035" Terumo Stiff Glide wire (Terumo) and Navi Cross Support Catheter (Terumo). After that the “riding” thrombus at SFA/PFA bifurcation, migrated distally and occluded the SFA and PFA (Figure 8). We started EVT from the proximal segment of SFA, with the same catheter AngioJet Solent Omni (2.06 mm). After that we did EVT in the middle segment of SFA and the popliteal artery (Figure 9). Due to residual thrombosis in distal segment of SFA, a balloon dilatation with Armada 5/120 mm (Abbott) was done (Figure 10).
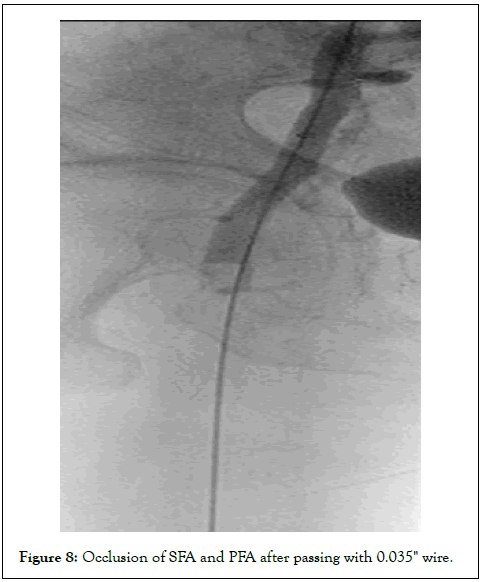
Figure 8: Occlusion of SFA and PFA after passing with 0.035" wire.
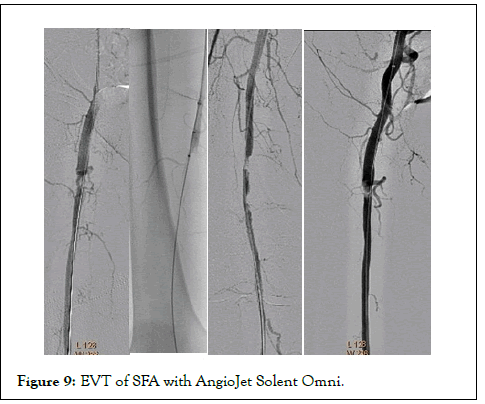
Figure 9: EVT of SFA with AngioJet Solent Omni.
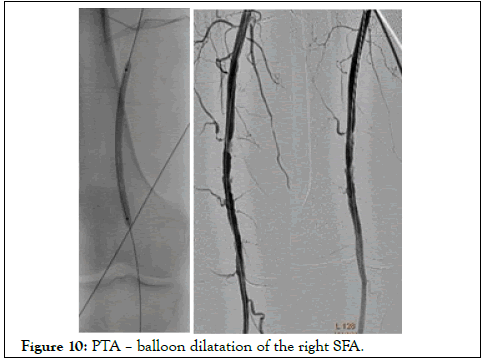
Figure 10: PTA – balloon dilatation of the right SFA.
Thereafter the right PFA was recanalized with 0.035" Angulated Terumo Glidewire (Terumo) and again EVT was performed with AngioJet Solent Omni (2.06 mm) (Figure 11).
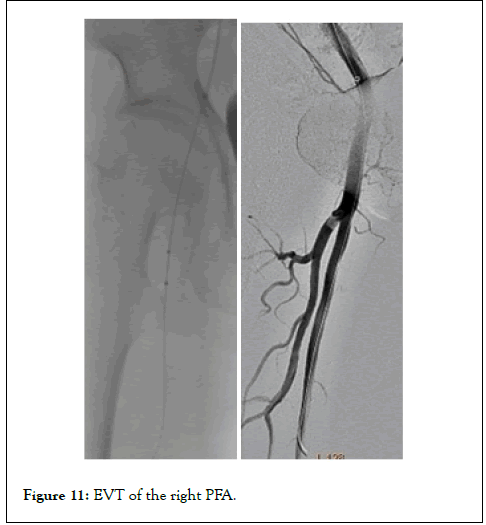
Figure 11: EVT of the right PFA.
Then balloon dilatations in posterior tibial and tibiofibular trunk - with balloons Pacific Plus 2/120 mm and 3/120 mm were done (Medtronic). Because of persistent thrombosis in the proximal segment of posterior tibial artery, again EVT was performed with AngioJet Solent Omni (2.06 mm). Finally distal blood flow was restored in the right SFA, PFA, popliteal and posterior tibial arteries (Figure 12).
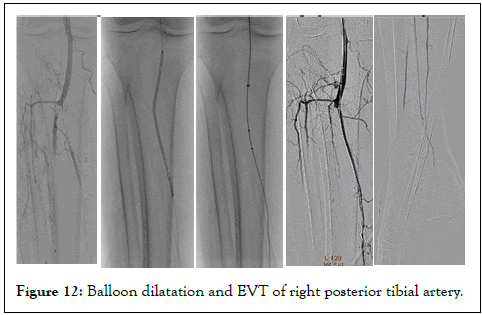
Figure 12:Balloon dilatation and EVT of right posterior tibial artery.
Post-procedural the patient received an intra-arterial infusion with unfractionated heparin (1000 IU/h), via the introducer with its tip in the right common femoral artery, for 48 hours, until therapeutic INR (2.0 to 2.5) was reached.
Medical therapy after discharge was Acetylsalicylic acid 100 mg q.d., Clopidogrel 75 mg q.d., Acenocoumarol 4 mg q.d. (INR target range 2.0 to 2.5), Bisoprolol 5 mg q.d., Rosuvastatin 20 mg q.d. and Pantoprazole 40 mg q.d.
The patient was discharged after 3 days. She returned 15 and 30 days later for a planned Doppler sonography, which objectifies preserved result of the endovascular thrombectomy of right axillary, brachial, radial, femoral, popliteal and posterior tibial artery (Figure 13).
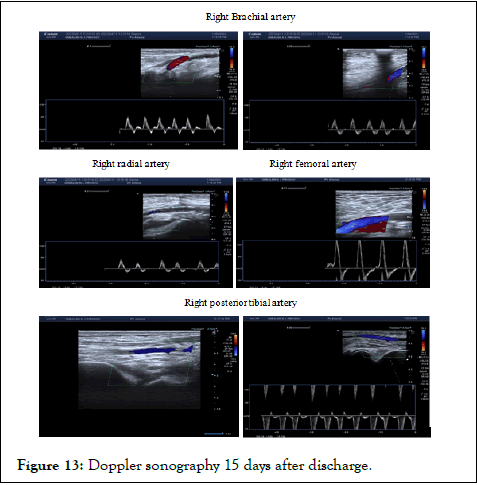
Figure 13:Doppler sonography 15 days after discharge.
Discussion
Embolism is defined as debris in the vascular system obstructing a distal artery. Acute thromboembolic events are a limb-threatening complication, necessitating immediate treatment. Lower extremity ischemia accounts for the majority of limb ischemia cases. Only 2%-18% of limb ischemia episodes are of the upper extremity [3]. The most common cause of acute upper extremity ischemia is emboli from a cardiac source. A mural thrombus mostly obstructs peripheral distal arteries, causing acute disruption of blood flow [4]. Moreover, the most common site of obstruction is at the origin of the profunda brachial artery or the bifurcation of the brachial artery. Other causes include thrombosis, atherosclerotic stenosis, arterial trauma, arterial dissection, and acute thrombosis of a stent or graft. Proximal atherosclerotic debris is a source of embolusdebris from the proximal aorta that breaks and lodges in the peripheral vessels [5].
When acute embolism occurs, it first manifests are sensory deficit, followed by a motor deficit and muscle weakness. Also, when there is an acute embolism, the limb becomes pale, and a neurosensory deficiency occurs because there are no established collaterals in a healthy artery. Rutherford classifies acute limb ischemia into three types based on clinical findings and Doppler measurements. These are viable extremities, threatened extremities, and irreversible defects. When irreversible defects occur, amputation is considered instead of revascularization [6].
Conclusion
When evaluating a patient with acute limb ischemia, it is essential to thoroughly assess the patient by taking a complete history and performing rapid diagnostic tests to preserve the patient’s limb and life. This case also emphasizes the importance of endovascular recanalization by AngioJet thrombectomy system. The main factor that can improve survival of patients with acute limb ischemia is early aggressive treatment aimed at restoring the patency of occluded arteries. Endovascular thrombectomy can be a simple, safe and welltolerated treatment modality for patients with ALI. However, such treatment should be performed in very experienced centers with this endovascular technique in different vascular territories and with full access to vascular surgical intervention in case of a failed endovascular approach.
Disclosures
Human subjects
Informed consent was obtained by all participants in this case.
Conflicts of interest
All authors declare the following:
Payment/services information: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
References
- Overview of upper extremity ischemia(2021)
- Lee MS, Singh V, Wilentz JR, Makkar RR. AngioJet thrombectomy. J Invasive Cardiol. 2004;16(10):587-591.
[Crossref] [Google Scholar] [PubMed]
- Stonebridge PA, Clason AE, Duncan AJ, Nolan B, Jenkins AM, Ruckley CV. Acute ischaemia of the upper limb compared with acute lower limb ischaemia; a 5-year review. Br J Surg. 1989;76:515-516.
[Crossref] [Google Scholar] [PubMed]
- Tawes RL, Harris EJ, Brown WH, Shoor PM, Zimmerman JJ, Sydorak GR, et al. Arterial embolism: a 20 year perspective. Arch Surg. 1985;120:595-600.
[Crossref] [Google Scholar] [PubMed]
- Javid M, Magee TR, Galland RB. Arterial thrombosis associated with malignant disease. Eur J Vasc Endovasc Surg. 2008;35:84-87.
[Crossref] [Google Scholar] [PubMed]
- Rutherford RB, Baker JD, Ernst C, Porter JM, Ahn S, Jones DN. Recommended standards for reports dealing with lower extremity ischemia: revised version. J Vasc Surg. 1997;26:518.
[Crossref] [Google Scholar] [PubMed]
Citation: Kernov S, Martinov I (2023) A Rare Case of Simultaneous Acute Embolic Occlusions of the Right Upper and Lower Extremity, Recanalized with Endovascular Thrombectomy. J Vasc Surg. 11:517.
Copyright: © 2023 Kernov S, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

