Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- MIAR
- University Grants Commission
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2022) Volume 13, Issue 1
A Case Report: Antibody Response to 2-Dose Pfizer Vaccine and Johnson and Johnson Vaccine in a Kidney Transplant Patient
Gita Taasoobshirazi1*, Shiva Zaman2 and Katayun Taasoobshirazi22Department ofInternal Medicine, Emory University Hospital, Georgia, United States
Received: 01-Feb-2022, Manuscript No. JVV-22-470; Editor assigned: 03-Feb-2022, Pre QC No. JVV-22-470(PQ); Reviewed: 17-Feb-2022, QC No. JVV-22-470; Revised: 22-Apr-2022, Manuscript No. JVV-22-470(R); Published: 28-Feb-2022, DOI: 10.35248/2157-7560.22.13.470
Abstract
Recent research has shown that immunocompromised individuals are less likely to build detectible SARS-CoV-2 spike protein antibodies after vaccination. This is distressing for the 11.5 million individuals on some form of immunosuppressive therapy as the SARS-CoV-2 virus can lead to more severe illness and greater risk for death among these individuals. This study fills a gap in the research on COVID-19 vaccination in immunocompromised individuals with a case study of how a kidney transplant patient responded to a series of COVID-19 vaccines. The case study presented in this paper introduces the vaccination schedule and antibody testing of a kidney transplant patient in effort to assess the efficacy of a series of SARS-CoV-2 vaccines. The patient did not make SARS-CoV-2 spike protein antibodies, as assessed by a Spike Protein IgG Antibody blood test, after a two-dose schedule of the Pfizer vaccine. It was recommended that the patient receive a dose of the Johnson & Johnson vaccine. The patient then tested positive for SARS-CoV-2 spike protein antibodies. Recommendations are made, using the case study findings and current studies on COVID-19 vaccinations, for a possible approach to the vaccination of immunocompromised individuals and for future research on COVID-19 vaccination studies with immunosuppressed patients.
Keywords
Antibodies; SARS-CoV-2; mRNA; Pfizer; Johnson & Johnson; Transplant patients; Immunocompromised patients
Introduction
In a March 2021 study published in the Journal of the American Medical Association (JAMA), researchers from Johns Hopkins School of Medicine found that only 17% of 436 individuals who received solid organ transplants produced antibodies after one dose of a COVID-19 vaccine (either Moderna or Pfizer; median test for antibodies after first dose of vaccine was 20 days) [1]. The demographics of the patients as reported by the researchers were: median age was 55.9 years, 61% were women and 89% were white. Fifty-two percent received the Pfizer vaccine and 48% were given the Modern vaccine. The median time since transplant was 6.2 years, and the most common immunosuppressant regimen included tacrolimus (83%); corticosteroids (54%); and mycophenolate (66%). None of the patients had a prior COVID-19 diagnosis.
A follow-up analysis by the same team of Johns Hopkins researchers published in May 2021 found that 357 out of 658 (54%) had detectible SARS-CoV-2 antibodies after the second vaccine administration (either Moderna or Pfizer; antibody testing after a median of 29 days after second dose) [2]. Of the 658 participants, 98 (15%) had an antibody response after both doses and 259 (39%) had no antibody response after dose 1 but did show a consequent antibody response after dose 2.To test for the presence of antibodies, the researchers used blood samples that assessed antibodies using EUROIMMUN anti–SARS-CoV-2 S enzyme immunoassay, or by samples tested using the Roche Elecsys anti–SARS-CoV-2 S enzyme immunoassay. The researchers found that younger patients, patients not taking antimetabolites (63% compared with 37% antibody production), and those who received two doses of the Moderna vaccine versus Pfizer vaccine (31% compared to 9%) were more likely to show an antibody response. Dr. Boyarski, the paper’s first author, made the final recommendation that “transplant recipients should not assume immunity. Even among those who had seroconverted, their antibody levels were relatively lower than what we see in people with competent immune systems.”
A similar study conducted by the Mayo Clinic and published in April, 2021 in the American Journal of Transplantation published findings from a small scale study with seven organ transplant recipients who were diagnosed with COVID-19 after receiving either the Pfizer or Moderna vaccines. Two patients had received one dose whereas five were fully vaccinated. Five of the patients were hospitalized. Only one of the patients had made antibodies against COVID-19 [3]. In a study with 88 liver transplant patients, antibodies were found in only 47.5% of patients after vaccination with the Pfizer vaccine [4]. Another study evaluated humoral response after vaccination with the Pfizer vaccine in 136 kidney transplant recipients compared to 25 controls. For the study, only participants with negative serology to SARS-CoV-2 nucleocapsid protein were included. All controls developed a positive response to spike protein whereas only 51 of 136 transplant recipients (37.5%) had positive serology [5].
Findings by these teams of researchers are crucial given that individuals with compromised immune systems were, in most part, excluded from the initial COVID-19 vaccine clinical trials. The same drugs that transplant patients take to prevent rejection also interfere with their ability to make antibodies to the substances in the COVID-19 vaccines. This is disheartening for transplant patients who have struggled to keep themselves protected during the pandemic and who were anxiously anticipating the availability of a vaccine. Additional studies regarding possible measures to increase patients’ immunological response to COVID-19 vaccination are essential. The present study attempts to fill this gap.
Dr. Dorry Segev, one of the researchers on the Johns Hopkins studies and associate vice chair for research and professor of surgery at Johns Hopkins University suggested that because the number of participants who developed antibodies after two mRNA vaccine doses was significantly higher than those who developed antibodies after one dose that “a three dose vaccine regimen could serve as a booster shot for immunocompromised patients.” No clinical trials are underway, yet, to test this hypothesis. There are also no published results from the use of the Johnson & Johnson vaccine for immunocompromised patients. This is important because the Johnson & Johnson vaccine provides a different mechanism for protection against COVID-19 than mRNA vaccines. Johnson & Johnson is an adenovirus vaccine or a viral vector vaccine that delivers DNA to cells to produce the spike protein; the immune system then creates antibodies toward the spike protein, providing protection from infection. Dr. Segev also mentioned in an interview with Editor-in-Chief Marty Makary, MD, MPH, of Johns Hopkins University in Baltimore: “I would love to see is some way for transplant patients who, after two doses, have had no immune response, to either get a third dose or to get a different agent. So maybe if the mRNA approach didn't work, get the Johnson and Johnson or something like that, to either cross over to a different system of vaccination or to just get a third dose of the vaccine they've already gotten. And I would love for that to be available to people” [6].
Dr. Segev’s recommendation is in line with a study that has shown that combining vaccines can boost COVID-19 immune response. Researchers from the Carlos III Health Institute compared 663 individuals who were administered a dose of Pfizer eight weeks after a dose of AstraZeneca (a single dose vector vaccine that is similar in mechanism to the Johnson & Johnson vaccine) to a control group that received only the one dose of AstraZeneca [7]. Those who were in the combined vaccine group had a significantly improved immune response than those in the control group. A limitation of this study was that there was no comparison of the experimental group to those who received two doses of Moderna, two doses of Pfizer, or a mix of Moderna and Pfizer vaccines.
As scientists explore different vaccine options, timelines, and combinations, preliminary findings by the University of Birmingham in collaboration with Public Health England have shown that antibodies against Sars-CoV-2 are 3.5 times higher in individuals who receive their second dose of Pfizer after 12 weeks rather than the initially recommended three weeks [8]. This may be important in improving an immune response in immunocompromised individuals. Given that the Johnson & Johnson vaccine uses a different mechanism for protecting from COVID-19 than mRNA vaccines, a combination of both may provide the best protection by stimulating both CD8T cells and an antibody response.
Research on the most potent vaccines, vaccine combinations, and inoculation scheduling is essential for providing immunosuppressed patients with the protection they need against the Sars-CoV-2 virus. Currently, it seems that transplant patients are not responding, to the same degree as the general population, to the available mRNA vaccinations. This paper presents a brief case study that describes the vaccine schedule of a kidney transplant patient who was given the recommendation to receive the two-dose Pfizer vaccine. When antibodies were not developed (as assessed by the Spike Protein IgG Antibody bloodtest) the Johnson & Johnson vaccine was administered, and the patient developed protective antibodies.`
Case Presentation
Transplant patient GG
GG is a 41-year-old, female, kidney transplant patient with no prior covid-19 diagnosis and no other medical conditions. GG is 18 years out from time of transplant. She is 5 foot, 7 inches and 150 pounds. Her transplant medication regime includes: tacrolimus (2 mg, 2x day), mycophenalate (500 mg, 2x day), metoprolol succinate (100 mg, 2x day), simvastatin (40 mg, 1x day), diovan (80 mg, 1x day), and lisinopril (20 mg, 1x day). Her creatinine, for the last year, has been on average, 1.3 mg/dL. GG worked from home since March 2020 and left her home only to visit her mother (who is also home bound). GG provided written informed consent to participate and Emory Hospital provided ethical approval for the study (Figure 1).
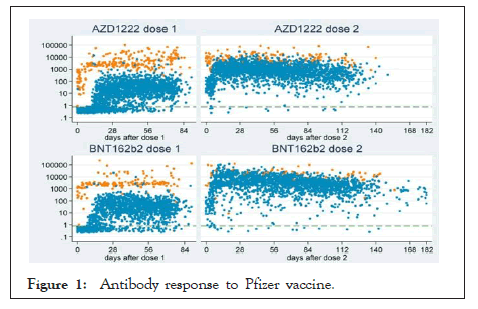
Figure 1: Antibody response to Pfizer vaccine.
GG received her first dose of the Pfizer vaccine on January 20, 2021. She did not take any pain-relieving medication the day before, day of, or day after the vaccine was administered. She noted no side effects from the vaccination. GG received her second dose of the Pfizer vaccine on February 10, 2021. She did not take any pain-relieving medication the day before, day of, or day after the vaccine was administered. She noted no side effects from the vaccination. Antibody testing, four weeks later, using an at home IgG IgM Antibody Rapid test showed no detectible antibodies. A SARS-CoV-2 Spike Protein IgG Antibody blood test taken one week later confirmed these results.
On May 10, 2021, GG was given the Johnson & Johnson vaccination. She did not take any pain-relieving medication the day before, day of, or day after the vaccine was administered. She noted that she felt body aches and chills that evening of May 10. She continued to feel mild cold symptoms the following day. Antibody testing, 13 days later, using an at home IgG IgM Antibody Rapid test showed no detectible antibodies. A SARSCoV- 2 Spike Protein IgG Antibody blood test on May 25, 2021, however, showed a positive result in COVID-19 Antibody IgG.
Results and Discussions
Given that organ transplant recipients are at higher risk for developing severe illness and/or death from COVID-19 and the fact that these same individuals have a weaker response to mRNA COVID-19 vaccinations, efforts to understand how to properly vaccinate and protect immunocompromised patients from the SARS-CoV-2 virus is critical. This is particularly true as nationwide efforts are being made to remove mask and social distancing mandates, to resume normal activities, and to lift COVID-19 travel restrictions.
Although this paper presents a case study with a single patient, it does confirm the lack of response of an immunocompromised patient to an mRNA vaccine and presents a follow up vaccination and testing approach. GG’s physician’s proposal, if antibodies were not present after the Johnson & Johnson vaccine, was to discuss a possible third Pfizer booster shot. This aggressive approach to vaccination is important given that the mortality rate among COVID-19 positive transplant patients is 24% compared to the 1% in the general population (Elias et al., 2020). This thoughtful evaluation of antibody response and vaccination adjustment provided GG protection from the COVID-19 virus. This could be lifesaving for GG and we recommend that physicians comprehensively evaluate their immunosuppressed patients’ vaccine response. We also recommend testing with an antibody blood test in the event of a negative (and potential false negative) at home IgG IgM Antibody Rapid test.
This case study with a single transplant patient showed that antibodies were not developed after a two dose Pfizer regimen but that antibodies were made after a follow-up Johnson and Johnson vaccine. The fact that GG felt ill after the Johnson & Johnson vaccine was a promising sign that she was responding to the vaccine. It may be that the Johnson & Johnson vaccine or the combination of the Pfizer and Johnson & Johnson vaccines led to an improved immune response. The Johnson & Johnson vaccine was administered 12 weeks after the second dose of Pfizer. Given the University of Birmingham study showing that antibodies against the Sars-CoV-2 are 3.5 times higher in individuals who receive their second dose of Pfizer after 12 weeks rather than the initially recommended three weeks, time between doses could be a contributing factor. Future research should disentangle the effects vaccine brand and time between inoculations. It may also be that a third dose of Moderna of Pfizer or combinations of these vaccines may be more effective than just a two-dose routine of the same vaccine. Experimental and comparison groups with different vaccine combinations and inoculation schedules can answer questions about the best vaccination schedules for immunocompromised individuals and how demographics, organ function, and immunosuppressive medications mediate humoral response.
Our transplant patient did not take any pain medication to mitigate her symptoms from the Johnson & Johnson vaccine. This was due to the U.S. Centers for Disease Control and Prevention’s recommendation against painkillers before a COVID-19 shot. The concern is that pre-treating with pain medications that reduce fevers and inflammation could diminish the immune system’s response to the vaccination [9]. GG chose to avoid pain medications before and after the vaccine to prevent any possible modulated immune response. This is something that should be considered in future research with immunosuppressed patients.
Conclusion
Finally, T-cells were not evaluated. It may be that mRNA vaccines do provide some protection in the form of T-cell mediation instead of antibody mediation in transplant patients. However, Dr. Peter Hoetz, dean of the National School of Tropical Medicine at Baylor University, believes that “doctors may want to have at least some indication of whether antibodies are present [among immunocompromised people] since protection against SARS-CoV-2 is especially important in people who are immunocompromised, because they are particularly at risk of severe disease and death. Having the information on antibodies at least gives us some sense they are protected”.
Author Contributions
Gita Taasoobshirazi designed the study and wrote the paper.
Introduction
Shiva Zaman designed the study and conducted the antibody testing.
Katayun Taasoobshirazi designed the study and conducted the antibody testing.
All authors approved the final version of the manuscript
REFERENCES
- Boyarsky BJ, Werbel WA, Avery RK, Tobian AA, Massie AB, Segev DL, et al. Immunogenicity of a single dose of SARS-CoV-2 messenger RNA vaccine in solid organ transplant recipients. Jama. 2021;325(17): 1784-1786.
[Crossref] [Google Scholar] [PubMed]
- Boyarsky BJ, Werbel WA, Avery RK, Tobian AA, Massie AB, Segev DL, et al. Antibody response to 2-dose SARS-CoV-2 mRNA vaccine series in solid organ transplant recipients. Jama. 2021;325(21): 2204-2206.
[Crossref] [Google Scholar] [PubMed]
- Wadei HM, Gonwa TA, Leoni JC, Shah SZ, Aslam N, Speicher LL. COVID-19 infection in solid organ transplant recipients after SARS- CoV-2 vaccination. Am J Transplant. 2021.
[Crossref] [Google Scholar] [PubMed]
- Rabinowich L, Grupper A, Baruch R, Ben-Yehoyada M, Halperin T, Turner D, et al. Low immunogenicity to SARS-CoV-2 vaccination among liver transplant recipients. J Hepatol. 2021.
[Crossref] [Google Scholar] [PubMed]
- Grupper A, Rabinowich L, Schwartz D, Schwartz IF, Ben-Yehoyada M, Shashar M, et al. Reduced humoral response to mRNA SARS-CoV-2 BNT162b2 vaccine in kidney transplant recipients without prior exposure to the virus. Am J Transplant. 2021.
[Crossref] [Google Scholar] [PubMed]
- Makary M. It's Kind of a Catch-22: Immunosuppression and COVID-19 Vaccines. 2021.
- Hogan A. This is what happens when you mix pfizer with another vaccine, study says. Bestlife. 2021.
- Sample I. Delay in giving second jabs of Pfizer vaccine improves immunity. The Guardian 2021.
- Chen JS, Alfajaro MM, Chow RD, Wei J, Filler RB, Eisenbarth SC, et al. Nonsteroidal anti-inflammatory drugs dampen the cytokine and antibody response to SARS-CoV-2 infection. J virol. 2021; 95(7): 00014-00021.
[Crossref] [Google Scholar] [PubMed]
Citation: Taasoobshirazi G, Zaman S, Taasoobshirazi K (2022) A Case Report: Antibody Response to 2-Dose Pfizer Vaccine and Johnson and Johnson Vaccine in a Kidney Transplant Patient. J Vaccines Vaccin. 13:470
Copyright: © 2022 Taasoobshirazi G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

