Indexed In
- Open J Gate
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
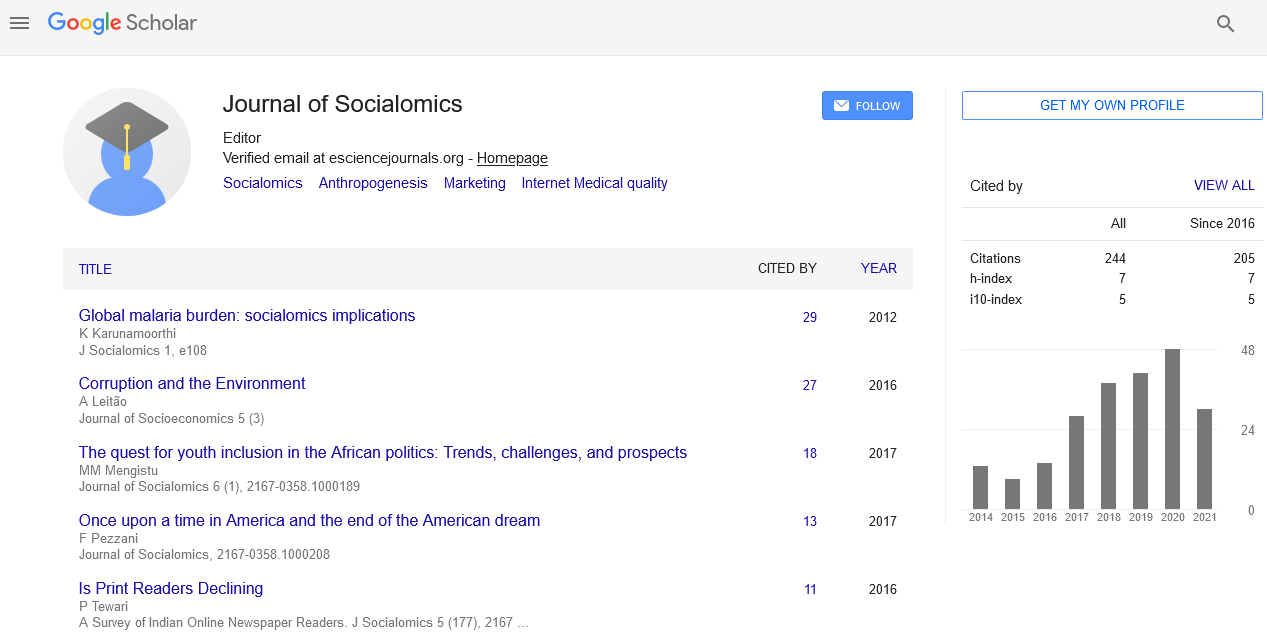
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
The role of medical cannabis in mental health: A literature review
Saranyan Senthelal
The use of cannabis in medicine is no new encounter. In fact, there is evidence that describes the use of medical cannabis dating back to 400 AD. More recently, cannabis was described as a medicine in the United States Pharmacopoeia in 1850. It was not until many years later, under the Controlled Substances Act of 1970, that cannabis became a prohibited substance in the United States. In Canada, cannabis was prohibited in 1923 under the Narcotics Drug Act Amendment Bill. Despite these attempted restrictions, according to the World Health Organization (WHO), cannabis is the most commonly abused illicit drug worldwide. With the legalization of cannabis in Canada, there has been an increasing interest regarding the psychological and physiological effects of cannabis. As cannabis use continues to steadily increase across Canada, healthcare providers must be aware of the potential indications or contraindications that this substance may provide for their patients. This review attempts to detail and highlight the necessary information found in the literature regarding the possible role of cannabis in psychiatric medicine. It should be noted that research in the field of medical cannabis is extremely limited at this point so it is difficult for any definitive conclusions to be made from the literature. The options that healthcare providers have surrounding the administration of medical cannabis include the use of cannabidiol (CBD) or delta–9– tetrahydrocannabinol (THC). Although both compounds are derived from the same plant and are associated with the endocannabinoid system in the body, they have very different psychopharmacological effects. THC binds to the cannabinoid 1 (CB1) receptors in the brain, producing the psychoactive effects commonly described by cannabis users as euphoric. CBD on the other hand, has very little interaction with CB1 receptors, if at all. In fact, CBD has been shown to even block these CB1 receptors and disrupt the THC and CB1 interaction. Although the literature remains limited, the use of cannabis in adolescents has not been shown to prove any significant benefit concerning the treatment of behavioral and intellectual disability. On the contrary, there have been unique cases that have shown the benefit of cannabis for refractory Tourette disorder and Autism Spectrum disorder. In adults, cannabis has been shown to increase the severity of depressive episodes in Major Depressive Disorder (p=0.1). However, multiple cases have shown relief of depressive and manic episodes in patients with Bipolar disorder. Next, psychotic disorders are of particular interest as rodent studies and a few cases have demonstrated the antipsychotic properties of cannabis in individuals already diagnosed with schizophrenia. Interestingly, multiple randomized controlled trials have shown an increased predilection for schizophrenia disorder in cannabis smoking individuals. The literature regarding anxiety disorders is limited but a randomized controlled trial showed relief of anxiety in patients with Social Anxiety Disorder (p=0.012), however, only a few case reports have shown similar findings in General Anxiety Disorder. Lastly, there has been improvement noted with cannabis use in both Obsessive Compulsive Disorder and Posttraumatic Stress Disorder.
Published Date: 2021-05-10; Received Date: 2021-03-27