Indexed In
- Open J Gate
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
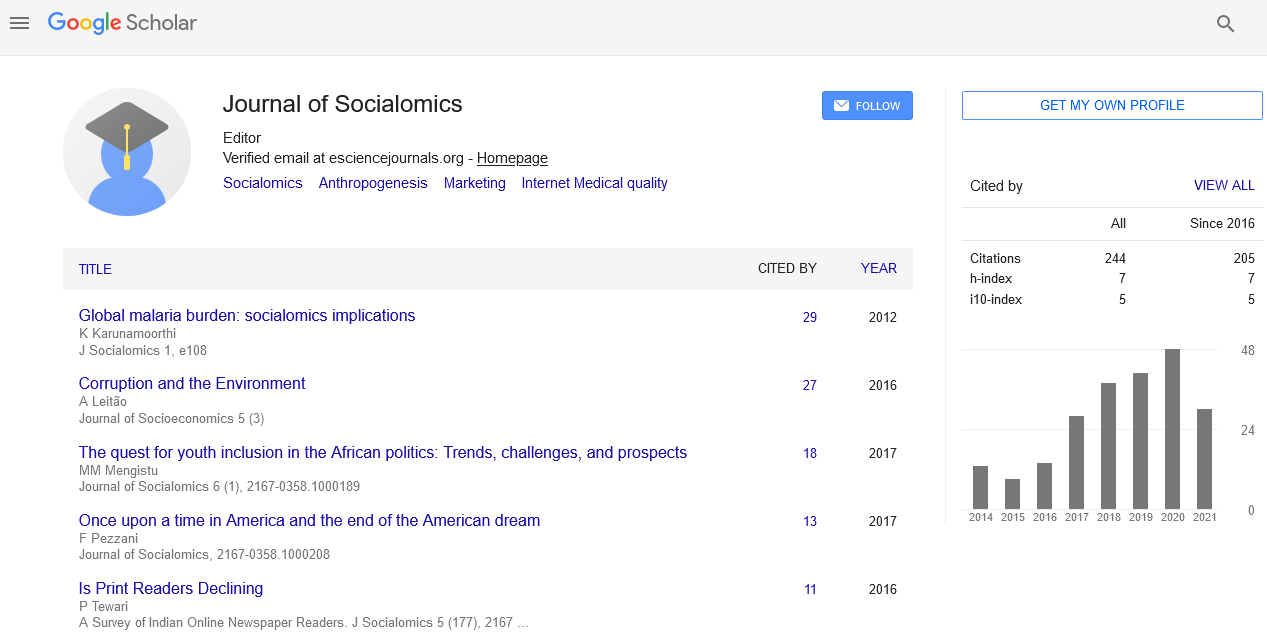
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
The risk of increasing violence against nurses and what we can do about the problem?
Sagar.k
Physical and verbal assault from our patients and their friends and relatives is not only difficult to deal with at the time but can have a long and lasting negative impact on our wellbeing and mental health. Yet, incidents appear to be on the rise with 6,245 code blacks (incidents where the safety of hospital staff is threatened) in South Australian public hospitals by February 2017 for the year 2016-17, compared to 4,765 at the same point in 2015-16. The Australian Institute of Criminology ranked healthcare facilities as the most violent workplaces in the country as far back as 1999, the trend for aggression has continued to increase both at home, and in the rest of the world. In fact, worldwide you’re more likely to be attacked at work if you are a nurse than a police officer.
The statistics make for alarming reading. According to the International Council of Nurses (ICN),
Nurses are the healthcare workers most at risk of an attack – particularly female nurses Physical assault is almost exclusively carried out by patients 97% of nurses who responded to a survey in the UK, knew of a nurse that had been physically assaulted within the past year Up to 95% of nurses report being bullied at work 72% of nurses don’t feel safe from assault in their workplace Up to 75% of nurses have been subjected to sexual harassment at work.Although emergency departments have the highest incidence of violence, with up to 90% of staff experiencing some form of violence in their careers, general patient rooms have now replaced psychiatric wards and units as the second most frequent area for attack. Violent behavior and abuse can occur to any healthcare worker in a clinical or community setting, including aged care facilities, and private practice. A recent campaign States to highlight the issue to both medical workers and the wider population. Whilst we can attempt to educate our communities about the issue and enforce a zero-abuse policy – often, this negative behavior comes from patients under the influence of drink, drugs, and other substances, or friends and relatives going through an emotionally turbulent time.
There is never an excuse for violence or abuse in the workplace from anyone, but understanding the reasons for it happening can help prevent further incidents and calm down an emotionally charged situation. The first step is recognizing what is aggressive and unwanted behavior.
We all know that extreme acts are unacceptable, but there is a spectrum of abuse ranging from swearing and eye-rolling, invasion of personal space, spitting and scratching right through to physical assault and attacks with weapons (which can range from scalpels to chairs dependent on what is close to hand).
Violent incidents are currently under-reported. When asked why victims don’t report violence, the most commonly cited reasons include:
No injury or time off work Reporting is too time-consuming Reporting lacks supervisory support Reporting won’t make any differenceIn fact, a study by Gerberich et al. found that 44% of nurses don’t report physical violence because it is just ‘part of the job’.
None of these acts of aggression are ok, and all of them should be reported. Although it might feel like it at times, violence and aggression is never ‘part of the job’, no matter what the person might be going through at that time.
Make sure you know what to do when you witness or experience violence or aggression – no matter how mild it might seem. Repetitive attacks can build and have a cumulative effect on your wellbeing, and that of your colleagues. So, use the reporting mechanisms you have in your workplace to keep your employer informed of what’s going on.
Your employer should be offering you appropriate support following aggressive incidents. If you or anyone you know needs immediate help in a crisis you can contact organizations like Nurse & Midwife Council Support or Lifeline.
One of the best things we can do as healthcare workers have a conversation with our peers and colleagues regarding aggressive behavior in our workplace. Staff that might have been affected by physical or verbal abuse might feel it’s a waste of time reporting incidents if nothing is done. What’s the point of filling in an incident report form if it gets filed away and nothing changes?
Regular briefings to go through reported incidents can not only help with identifying the triggers in that situation and how they could be addressed in the future but can also ensure that the staff affected have a full and frank opportunity to reflect on what happened. Events like these can often play on the mind and cause problems days or even weeks down the line.
One of the long-lasting effects of an aggressive incident is that it can affect the way that we interact with our patients. With less empathy and a self-imposed ‘distance’ – the quality of care can certainly suffer. In fact, there is a clearly identified link between violence experienced by nurses and subsequent adverse events in patients, including increased medication errors, patient falls, and late administration of medication (Roche et al. 2010).
Prevention is by far the best approach to take when managing violence in the workplace and some of the measures include:
Most hospitals will have security guards in ‘high risk’ areas such as emergency departments, other approaches can be taken in smaller clinics and facilities such as panic alarms, aggression minimization training for staff, and even workplace design.
Workplace design is something that is increasingly becoming used to prevent workplace violence. The Australasian College of Emergency Medicine has some recommendations for workplace design, which include:
• A lack of hiding spaces outside emergency departments
• Physical barriers such as glass screens in triage
• Restricted access areas
• Good lighting
• The use of CCTV cameras
• Visible security presence
Published Date: 2020-07-03; Received Date: 2020-04-02